Abstract
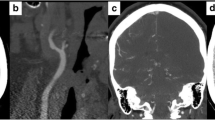
Traumatic carotid artery dissection (tCAD) bears the risk of hypoperfusion inducing delayed cerebral ischemia. The lack of consensus on standard treatment of tCAD remains a great challenge. Here, we present our successes on a series of patients with delayed tCAD diagnosis and treatment using multimodality treatment strategies. We retrospectively reviewed 21 patients with tCAD treated with carotid artery stent placement or anticoagulation therapy. There were 14 dissection locations (66.67 %) which involved extracranial internal carotid artery (ICA) and seven locations (33.33 %) which involved both extracranial and intracranial ICA. Stenosis severity was 70–99 % in 16 cases (76.19 %) and <70 % in 5 cases (23.81 %). Endovascular stents were administrated to 17 patients with hypoperfusion as evaluated by radiological methods, while anticoagulation therapy was administrated to the other four patients. Carotid revascularization was performed with one (9/17 patients) or multiple (8/17 patients) stents. None of the patients experienced a procedure-related complication. At discharge, the mean modified Rankin Scale (mRS) score of patients was 1.08 ± 0.76. Neither additional neurological deficient nor restenosis happened during the follow-up period. More vigilance is required to assure timely diagnosis of patients with delayed tCAD. Assessment of cerebral perfusion is an effective approach in tCAD treatment in our experience.



Similar content being viewed by others
References
Beletsky V, Nadareishvili Z, Lynch J, Shuaib A, Woolfenden A, Norris JW (2003) Cervical arterial dissection: time for a therapeutic trial? Stroke 34(12):2856–2860
Benninger DH, Georgiadis D, Kremer C, Studer A, Nedeltchev K, Baumgartner RW (2004) Mechanism of ischemic infarct in spontaneous carotid dissection. Stroke 35(2):482–485
Berne JD, Cook A, Rowe SA, Norwood SH (2010) A multivariate logistic regression analysis of risk factors for blunt cerebrovascular injury. J Vasc Surg 51(1):57–64
Biondi A, Katz JM, Vallabh J, Segal AZ, Gobin YP (2005) Progressive symptomatic carotid dissection treated with multiple stents. Stroke 36(9):e80–e82
Chandra A, Suliman A, Angle N (2007) Spontaneous dissection of the carotid and vertebral arteries: the 10-year UCSD experience. Ann Vasc Surg 21(2):178–185
Chang AJ, Mylonakis E, Karanasias P, De Orchis DF, Gold R (1999) Spontaneous bilateral vertebral artery dissections: case report and literature review. Mayo Clin Proc 74(9):893–896
Chen CJ, Tseng YC, Lee TH, Hsu HL, See LC (2004) Multisection CT angiography compared with catheter angiography in diagnosing vertebral artery dissection. AJNR Am J Neuroradiol 25(5):769–774
Chomel A, Vernet M, Lile A, Messant I, Combes JC, Freysz M (2002) Traumatic bilateral dissections of the internal carotid artery: an infrequent diagnosis not to be missed. J Neurosurg Anesthesiol 14(4):309–312
Debette S, Leys D (2009) Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurology 8(7):668–678
Donas KP, Mayer D, Guber I, Baumgartner R, Genoni M, Lachat M (2008) Endovascular repair of extracranial carotid artery dissection: current status and level of evidence. J Vasc Interv Radiol 19(12):1693–1698
Duke BJ, Ryu RK, Coldwell DM, Brega KE (1997) Treatment of blunt injury to the carotid artery by using endovascular stents: an early experience. J Neurosurg 87:825–829
Fabian TC, Patton JH Jr, Croce MA, Minard G, Kudsk KA, Pritchard FE (1996) Blunt carotid injury. Importance of early diagnosis and anticoagulant therapy. Ann Surg 223:513–525
Furie KL et al (2011) Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42(1):227–276
Gopalan D, Thomas SM (2006) Pharmacotherapy for patients undergoing carotid stenting. Eur J Radiol 60(1):14–19
Gortler D, Schlosser FJ, Muhs BE, Nelson MA, Dardik A (2008) Periprocedural drug therapy in carotid artery stenting: the need for more evidence. Vascular 16(6):303–309
Ohta H, Natarajan SK, Hauck EF, Khalessi AA, Siddiqui AH, Hopkins LN, Levy EI (2011) Endovascular stent therapy for extracranial and intracranial carotid artery dissection: single-center experience. J Neurosurg 115:91–100
Cohen JE, Gomori JM, Itshayek E, Spektor S, Shoshan Y, Rosenthal G, Moscovici S (2011) Single-center experience on endovascular reconstruction of traumatic internal carotid artery dissections. J Trauma 72(1):216–221
Linskey ME, Jungreis CA, Yonas H, Hirsch WL Jr, Sekhar LN, Horton JA, Janosky JE (1994) Stroke risk after abrupt internal carotid artery sacrifice: accuracy of preoperative assessment with balloon test occlusion and stable xenon-enhanced CT. AJNR Am J Neuroradiol 15(5):829–843
Ono H, Nakatomi H, Tsutsumi K, Inoue T, Teraoka A, Yoshimoto Y, Ide T, Kitanaka C, Ueki K, Imai H, Saito N (2013) Symptomatic recurrence of intracranial arterial dissections: follow-up study of 143 consecutive cases and pathological investigation. Stroke 44(1):126–131
Schelfaut D, Dhondt E, De Raedt S, Nieboer K, Hubloue I (2012) Carotid artery dissection: three cases and a review of the literature. Eur J Emerg Med 19(3):181–187
Schievink WI (2001) Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 344(12):898–906
Schievink WI, Roiter V (2005) Epidemiology of cervical artery dissection. Front Neurol Neurosci 20:12–15
Server A, Dullerud R, Haakonsen M, Nakstad PH, Johnsen UL (2001) Post-traumatic cerebral infarction. Neuroimaging findings, etiology and outcome. Acta Radiol 42(3):254–260
Seth R, Obuchowski AM, Zoarski GH (2013) Endovascular repair of traumatic cervical internal carotid artery injuries: a safe and effective treatment option. AJNR Am J Neuroradiol 34(6):1219–1226
Stein DM, Boswell S, Sliker CW (2009) Blunt cerebrovascular injuries: does treatment always matter? J Trauma, 66(1): p. 132-43; discussion 143-4.
Taschner CA, Leclerc X, Lucas C, Pruvo JP (2005) Computed tomography angiography for the evaluation of carotid artery dissections. Front Neurol Neurosci 20:119–128
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Daphne D. Li and Christopher M. Loftus, Maywood, USA
The authors of this article conducted a retrospective review of treatment and management of 21 patients with traumatic carotid artery dissection (tCAD). tCAD is a leading cause of stroke in young people, but there is a lack of consensus regarding a standard of treatment. In addition, the authors believe that tCAD warrants alternative strategies of treatment, as opposed to spontaneous CAD, because of inadequate response to conservative therapy and increased vulnerability to ischemic secondary to traumatic injury. The authors of this retrospective study hope to provide some insight into guiding management.
The authors of this study review the diagnosis and treatment algorithm for patients with traumatic injury and a high suspicion for tCAD. Initial evaluation with CTA/MRA and subsequent diagnosis and/or treatment through formal angiography resulted in good outcomes and zero complications for the patients included in this study.
Based on their experience, the authors conclude that assessment of cerebral perfusion may be an effective approach to guiding tCAD. As well, vigilance is key in assuring timely diagnosis, as tCAD may make a delayed appearance in a patient’s hospital course or symptoms may be masked by coexisting traumatic injuries. They also identify patients with injuries involving sudden neck movements and cervical spine or skull base fractures as high-risk patients.
The authors present a retrospective study on a small sample size of patients in an effort to optimize management of tCAD. Follow-up length was limited to 72 months at most, with 43 months on average. No patients had complete carotid occlusion. The aforementioned are limitations that prevent us from making generalized conclusions regarding tCAD management and applying it to all patients with carotid stenosis. Future investigations may be better guided in their study design, with a larger sample size and longer follow-up in order to contribute to the growing body of literature on optimal AVM management.
Tamer Hassan, Alexandria, Egypt
Zhengxing et al. have discussed very important category of cerebrovascular diseases namely TCAD that still lack consensus of appropriate clear treatment methodology. Although 21 patients are few number to have solid conclusion, still the authors combine the use of perfusion and angiographic studies to make the appropriate judgment of treatment methodology in a very wise and logic way. The combination of different treatment methodology options also like anticoagulation therapy, bypass surgery, and endovascular stenting in the same neurosurgery department hit the ring of important message that they offer all possible options for patient care for patients’ own sake in the same department. I believe that the paper is interesting to read and congratulate the group for their work.
Rights and permissions
About this article
Cite this article
Zhengxing, X., Zhenwen, C., Yuhao, S. et al. Management of traumatic carotid artery dissection: initial experience of a single center. Neurosurg Rev 39, 393–399 (2016). https://doi.org/10.1007/s10143-015-0689-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0689-0