Abstract
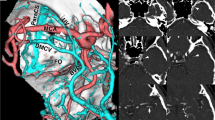
In cavernous sinus (CS) surgery, venous complication may occur in some types of venous drainage. The sphenobasal vein (SBV) drains from the superficial middle cerebral vein (SMCV) to the pterygoid venous plexus at the temporal skull base. A frontotemporal epi- and interdural approach (Dolenc approach), which is one of the CS approaches, may damage the SBV’s route. We report a case of intracavernous trigeminal schwannoma that contained the SBV and discuss our modified surgical procedure that combined epi- and subdural approaches to preserve the SBV. A 64-year-old man complained of right progressive oculomotor palsy and was referred to our hospital for surgery. MR images revealed a hemorrhagic tumor in the right CS. Three-dimensional venography revealed that the SMCV drained into the pterygoid venous plexus via the SBV. After identifying the first branch of the trigeminal nerve epidurally, we incised the dura linearly along the sylvian fissure and entered the subdural space to visualize the SBV. The incision was continued to the meningeal dura of the lateral wall of the CS along the superior margin of the first branch of the trigeminal nerve, and the Parkinson’s triangle was opened from the subdural side. The tumor was grossly totally removed, and the SBV was preserved. In conclusion, a frontotemporal epi- and subdural approach to the intracavernous trigeminal schwannoma can effectively preserve the SBV.




Similar content being viewed by others
References
Di Chiro G (1962) Angiographic patterns of cerebral convexity veins and superficial dural sinuses. Am J Roentgenol Radium Ther Nucl Med 87:308–321
Dolenc VV (1994) Frontotemporal epidural approach to trigeminal neurinomas. Acta Neurochir (Wien) 130:55–65
Dolenc V (2003) Petroclival meningiomas. In: Dolenc V (ed) Microsurgical anatomy and surgery of the central skull base. Springer, New York, pp 185–192
Genka S, Terao H, Matsutani M, Hori T, Ikeda A (1981) A choice of two-stage operation and the microsurgical anatomy for large trigeminal neurinoma (author’s transl). No Shinkei Geka 9:747–751
Hacker H (1974) Normal supratentorial veins and dural sinus. Mosby, St Louis
Hakuba A, Tanaka K, Suzuki T, Nishimura S (1989) A combined orbitozygomatic infratemporal epidural and subdural approach for lesions involving the entire cavernous sinus. J Neurosurg 71:699–704
Hayashi N, Sato H, Tsuboi Y, Nagai S, Kuwayama N, Endo S (2010) Consequences of preoperative evaluation of patterns of drainage of the cavernous sinus in patients treated using the anterior transpetrosal approach. Neurol Med Chir (Tokyo) 50:373–377
Ichimura S, Yoshida K, Kagami H, Inaba M, Orii M, Kitamura Y, Saga I, Toda M (2012) Epidural anterior petrosectomy with subdural visualization of sphenobasal vein via the anterior transpetrosal approach—technical case report. Neurosurg Rev 35:609–613, discussion 613–604
Jones F (1950) Buchanan’s manual of anatomy. Bailliere, Tindall & Cox, London, p 262
Kawase T, van Loveren H, Keller JT, Tew JM (1996) Meningeal architecture of the cavernous sinus: clinical and surgical implications. Neurosurgery 39:527–534, discussion 534–526
Kobayashi M, Yoshida K, Kawase T (2010) Inter-dural approach to parasellar tumors. Acta Neurochir (Wien) 152:279–284, discussion 284–275
McCormick PC, Bello JA, Post KD (1988) Trigeminal schwannoma. Surgical series of 14 cases with review of the literature. J Neurosurg 69:850–860
Nakase H, Shin Y, Nakagawa I, Kimura R, Sakaki T (2005) Clinical features of postoperative cerebral venous infarction. Acta Neurochir (Wien) 147:621–626, discussion 626
Otsuka H, Nakase H, Nagata K, Ueda K, Kempski O, Sakaki T (2000) Effect of age on cerebral venous circulation disturbances in the rat. J Neurosurg 93:298–304
Pelissou I, Sindou M, Goutelle A, Pialat J, Duquesnel J (1988) Neurinoma of the trigeminal nerve. Excision by combined suboccipital and pteriono-temporal approach. Neurochirurgie 34:8–16
Pollack IF, Sekhar LN, Jannetta PJ, Janecka IP (1989) Neurilemomas of the trigeminal nerve. J Neurosurg 70:737–745
Sekhar LN, Moller AR (1986) Operative management of tumors involving the cavernous sinus. J Neurosurg 64:879–889
Shibao S, Toda M, Orii M, Fujiwara H, Yoshida K (2015) Various patterns of the middle cerebral vein and preservation of venous drainage during the anterior transpetrosal approach. J Neurosurg
Suzuki Y, Matsumoto K (2000) Variations of the superficial middle cerebral vein: classification using three-dimensional CT angiography. AJNR Am J Neuroradiol 21:932–938
Tanoue S, Kiyosue H, Okahara M, Sagara Y, Hori Y, Kashiwagi J, Mori H (2006) Para-cavernous sinus venous structures: anatomic variations and pathologic conditions evaluated on fat-suppressed 3D fast gradient-echo MR images. AJNR Am J Neuroradiol 27:1083–1089
Wolf BS, Huang YP, Newman CM (1963) The superficial sylvian venous drainage system. Am J Roentgenol Radium Ther Nucl Med 89:398–410
Yamakami I, Hirai S, Yamaura A, Ono J (1998) Venous system playing a key role in transpetrosal approach. No Shinkei Geka 26:699–707
Yasuda A, Campero A, Martins C, Rhoton AL Jr, Ribas GC (2004) The medial wall of the cavernous sinus: microsurgical anatomy. Neurosurgery 55:179–189, discussion 189-190
Yoshida K, Kawase T (1999) Trigeminal neurinomas extending into multiple fossae: surgical methods and review of the literature. J Neurosurg 91:202–211
Conflict of interest
The authors declare that they have no competing interests.
Compliance with ethical standards
Informed consent was obtained from the patient.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Antonio Bernardo, New York, USA
The authors present a case report on a modified epidural/subdural approach with preservation of the sphenobasal sinus and discussed the complications associated with damage to the sinus. The surgical procedure and its rationale are very well described and justified by the positive clinical and radiological outcomes. We applaud the authors for this interesting report on a technically challenging procedure. In the case of the superior middle cerebral vein (SMCV) draining into the pterygoid venous plexus via the sphenobasal vein (SBV), the epi- and interdural approach may interrupt these drainage routes and result in postoperative temporal lobe swelling when the SBV is the main route of venous drainage. The combined epidural/subdural variation of this approach described by the authors would effectively preserve the SBV. The epidural portion of this procedure is simply used to localize V1 and has nothing to do with the primary goal of preserving the sphenobasal sinus—as that is the objective of the subdural step. Nonetheless, this step is important as it facilitates safe entry into Parkinson’s triangle from the subdural space after epidural visualization of V1. Given that a tumor may distort the anatomy, the epidural orientation is seemingly justified. I concur with the authors that epidural exposure could reasonably increase the risk of damage to venous structures. As stated in the paper, the emissary sphenoid foramen, present in 20 % of individuals, contains an emissary vein connecting the CS and the pterygoid venous plexus and its presence may hinder lateral extradural approaches to the skull base. However, it should be considered that in a number of cases, particularly those with smaller lesions, it is not necessary to expose the foramen ovale and the entire lateral wall of the cavernous sinus. In these cases, extradural exposure can be minimal and should consist of removal of the anterior clinoid process, exposure of the entire superior ophthalmic fissure, identification of CN IV and V1, and extradural entrance into Parkinson’s triangle avoiding exposure of the foramen ovale and the entire Gasserian ganglion. There is also no need to open the optic canal unless mobilization of the optic nerve is required due to the size and location of the lesion.
Alternatively, the SBV can be visualized intradurally, as performed herein. The authors decided to open the cavernous sinus intradurally to avoid injuring the SBV. In my opinion, given that the figures clearly depict the confluence of the SMCV into the SBV, from the intradural perspective caudal to V1, the Parkinson’s triangle could have been entered extradurally as the extradural surgical corridor is above V1. The combination of subdural visualization of the venous drainage routes and extradural access to the cavernous sinus would mitigate the need for direct retraction of the frontal or temporal lobe and sparing of the SBV.
Kenji Ohata, Osaka, Japan
This study is interesting in highlighting the preservation of the sphenobasal vein in cavernous sinus surgery. It concludes that a frontotemporal epidural and subdural approach to the intracavernous trigeminal schwannoma can effectively preserve the sphenobasal vein.
Recently developed radiological studies including high resolution computerized tomography and magnetic resonance imaging have provided valuable preoperative evaluations of cavernous sinus lesions.
The concept of this procedure of frontotemporal epidural and subdural approach to cavernous sinus tumor is more or less similar to Hakuba’s procedure. The surgical technique of Hakuba’s combined orbitozygomatic infratemporal epidural and subdural approach focused on lesions involving the entire cavernous sinus. In case of tumors involving the entire cavernous sinus, significant venous bleeding is not encountered because of compression of the venous pathways by the tumor itself. The author here described a case of trigeminal schwannoma with hemorrhage and the superficial middle cerebral vein draining into the pterygoid plexus via the sphenobasal vein without other collateral drainage, enabling them to visualize the first branch of the trigeminal nerve from both the epidural and subdural sides without sphenobasal vein injury. This part of the procedure differs from Hakuba’s procedure.
Major draining veins with relation to the temporal lobe are encountered in the skull base surgery and are at potential risk of venous hemorrhagic complications. Surgical procedure should be designed in a way to prevent injury of these veins.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(M4V 84892 kb)
Rights and permissions
About this article
Cite this article
Shibao, S., Akiyama, T., Tomita, H. et al. Frontotemporal epi- and subdural approach to a cavernous sinus tumor for sphenobasal vein preservation—technical case report. Neurosurg Rev 39, 169–174 (2016). https://doi.org/10.1007/s10143-015-0670-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0670-y