Abstract
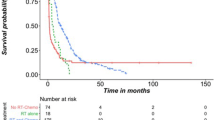
The purpose of this study is to investigate the patient characteristics and clinical outcomes of children with pediatric brainstem glioma. Between 2004 and 2009, a total of 42 children were diagnosed with brainstem gliomas at the Neurosurgical Center of Beijing Tiantan Hospital, China. A retrospective study including the 33 patients of this cohort with complete follow-up was conducted in an attempt to better understand clinical outcomes following multidisciplinary treatment modalities for pediatric brainstem gliomas. Investigational variables including clinical presentations, anatomical distribution, radiological findings, and clinical outcomes were analyzed. Survival time difference was computed using a Kaplan–Meier method with a log-rank test between groups. The Cox proportional hazards regression model was utilized in the multivariate analysis to determine the independent prognostic factors. Overall median survival of the entire series of patients was 11 months with a 1-year actuarial survival rate of 43.6 %. In nine patients who received no treatment after diagnosis, all patients expired within 8 months with a median time of 3.5 months. On univariate analysis, the following variables including older age at diagnosis, higher Karnofsky Performance Status score at diagnosis, the lower pathological grade, surgical resection modality, increasing diagnostic latency, and focal growth pattern were associated with better survival. On multivariate analysis, only the last two variables were associated with survival advantage. Focal pediatric brainstem gliomas amenable to a surgical resection are likely to achieve a prolonged survival. Clinical trials on larger number of patients are of importance in further understanding this spectrum of devastating diseases.









Similar content being viewed by others
References
Albright AL, Guthkelch AN, Packer RJ, Price RA, Rourke LB (1986) Prognostic factors in pediatric brain-stem gliomas. J Neurosurg 65:751–755
Albright AL, Packer RJ, Zimmerman R, Rorke LB, Boyett J, Hammond GD (1993) Magnetic resonance scans should replace biopsies for the diagnosis of diffuse brain stem gliomas: a report from the Children’s Cancer Group. Neurosurgery 33:1026–1029, discussion 1029-1030
Barkovich AJ (2000) Pediatric neuroimaging. In: Barkovich AJ (ed) Intracranial, orbital, and neck tumors of childhood. Lippincott Williams & Wilkins, Philadelphia, pp 462–470
Bouffet E, Raquin M, Doz F, Gentet JC, Rodary C, Demeocq F, Chastagner P, Lutz P, Hartmann O, Kalifa C (2000) Radiotherapy followed by high dose busulfan and thiotepa: a prospective assessment of high dose chemotherapy in children with diffuse pontine gliomas. Cancer 88:685–692
Bowers DC, Georgiades C, Aronson LJ, Carson BS, Weingart JD, Wharam MD, Melhem ER, Burger PC, Cohen KJ (2000) Tectal gliomas: natural history of an indolent lesion in pediatric patients. Pediatr Neurosurg 32:24–29
Bricolo A, Turazzi S, Cristofori L, Talacchi A (1991) Direct surgery for brainstem tumours. Acta Neurochir Suppl (Wien) 53:148–158
Broniscer A, Baker JN, Tagen M, Onar-Thomas A, Gilbertson RJ, Davidoff AM, Panandiker AS, Leung W, Chin TK, Stewart CF, Kocak M, Rowland C, Merchant TE, Kaste SC, Gajjar A (2010) Phase I study of vandetanib during and after radiotherapy in children with diffuse intrinsic pontine glioma. J Clin Oncol 28:4762–4768
Chang DY, Yoo SW, Hong Y, Kim S, Kim SJ, Yoon SH, Cho KG, Paek SH, Lee YD, Kim SS, Suh-Kim H (2010) The growth of brain tumors can be suppressed by multiple transplantation of mesenchymal stem cells expressing cytosine deaminase. Int J Cancer 127:1975–1983
Chiang KL, Chang KP, Lee YY, Huang PI, Hsu TR, Chen YW, Chang FC, Wong TT (2010) Role of temozolomide in the treatment of newly diagnosed diffuse brainstem glioma in children: experience at a single institution. Childs Nerv Syst 26:1035–1041
Constantini S, Epstein F (1996) Surgical indication and technical considerations in the management of benign brain stem gliomas. J Neurooncol 28:193–205
Epstein F, Constantini S (1996) Practical decisions in the treatment of pediatric brain stem tumors. Pediatr Neurosurg 24:24–34
Fischbein NJ, Prados MD, Wara W, Russo C, Edwards MS, Barkovich AJ (1996) Radiologic classification of brain stem tumors: correlation of magnetic resonance imaging appearance with clinical outcome. Pediatr Neurosurg 24:9–23
Fisher PG, Breiter SN, Carson BS, Wharam MD, Williams JA, Weingart JD, Foer DR, Goldthwaite PT, Tihan T, Burger PC (2000) A clinicopathologic reappraisal of brain stem tumor classification. Identification of pilocystic astrocytoma and fibrillary astrocytoma as distinct entities. Cancer 89:1569–1576
Freeman CR, Farmer JP (1998) Pediatric brain stem gliomas: a review. Int J Radiat Oncol Biol Phys 40:265–271
Giussani C, Poliakov A, Ferri RT, Plawner LL, Browd SR, Shaw DW, Filardi TZ, Hoeppner C, Geyer JR, Olson JM, Douglas JG, Villavicencio EH, Ellenbogen RG, Ojemann JG (2010) DTI fiber tracking to differentiate demyelinating diseases from diffuse brain stem glioma. NeuroImage 52:217–223
Guillamo JS, Doz F, Delattre JY (2001) Brain stem gliomas. Curr Opin Neurol 14:711–715
Gururangan S, Chi SN, Young Poussaint T, Onar-Thomas A, Gilbertson RJ, Vajapeyam S, Friedman HS, Packer RJ, Rood BN, Boyett JM, Kun LE (2010) Lack of efficacy of bevacizumab plus irinotecan in children with recurrent malignant glioma and diffuse brainstem glioma: a Pediatric Brain Tumor Consortium study. J Clin Oncol 28:3069–3075
Jalali R, Raut N, Arora B, Gupta T, Dutta D, Munshi A, Sarin R, Kurkure P (2010) Prospective evaluation of radiotherapy with concurrent and adjuvant temozolomide in children with newly diagnosed diffuse intrinsic pontine glioma. Int J Radiat Oncol Biol Phys 77:113–118
Kalkanis SN, Kondziolka D, Gaspar LE, Burri SH, Asher AL, Cobbs CS, Ammirati M, Robinson PD, Andrews DW, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Linskey ME (2010) The role of surgical resection in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96:33–43
Karajannis M, Allen JC, Newcomb EW (2008) Treatment of pediatric brain tumors. J Cell Physiol 217:584–589
Korones DN, Fisher PG, Kretschmar C, Zhou T, Chen Z, Kepner J, Freeman C (2008) Treatment of children with diffuse intrinsic brain stem glioma with radiotherapy, vincristine and oral VP-16: a Children’s Oncology Group phase II study. Pediatr Blood Cancer 50:227–230
Laigle-Donadey F, Doz F, Delattre JY (2008) Brainstem gliomas in children and adults. Curr Opin Oncol 20:662–667
Landolfi JC, Thaler HT, DeAngelis LM (1998) Adult brainstem gliomas. Neurology 51:1136–1139
Mandell LR, Kadota R, Freeman C, Douglass EC, Fontanesi J, Cohen ME, Kovnar E, Burger P, Sanford RA, Kepner J, Friedman H, Kun LE (1999) There is no role for hyperfractionated radiotherapy in the management of children with newly diagnosed diffuse intrinsic brainstem tumors: results of a Pediatric Oncology Group phase III trial comparing conventional vs. hyperfractionated radiotherapy. Int J Radiat Oncol Biol Phys 43:959–964
Maria BL, Rehder K, Eskin TA, Hamed LM, Fennell EB, Quisling RG, Mickle JP, Marcus RB Jr, Drane WE, Mendenhall NP et al (1993) Brainstem glioma: I. Pathology, clinical features, and therapy. J Child Neurol 8:112–128
Massimino M, Spreafico F, Biassoni V, Simonetti F, Riva D, Trecate G, Giombini S, Poggi G, Pecori E, Pignoli E, Casanova M, Ferrari A, Meazza C, Luksch R, Terenziani M, Cefalo G, Podda M, Polastri D, Clerici CA, Fossati-Bellani F, Gandola L (2008) Diffuse pontine gliomas in children: changing strategies, changing results? A mono-institutional 20-year experience. J Neurooncol 87:355–361
Mauffrey C (2006) Paediatric brainstem gliomas: prognostic factors and management. J Clin Neurosci 13:431–437
Mehta VS, Chandra PS, Singh PK, Garg A, Rath GK (2009) Surgical considerations for ‘intrinsic’ brainstem gliomas: proposal of a modification in classification. Neurol India 57:274–281
Michalski A, Bouffet E, Taylor RE, Hargrave D, Walker D, Picton S, Robinson K, Pizer B, Bujkiewicz S (2010) The addition of high-dose tamoxifen to standard radiotherapy does not improve the survival of patients with diffuse intrinsic pontine glioma. J Neurooncol 100:81–88
Minturn JE, Janss AJ, Fisher PG, Allen JC, Patti R, Phillips PC, Belasco JB (2011) A phase II study of metronomic oral topotecan for recurrent childhood brain tumors. Pediatr Blood Cancer 56:39–44
Pollack IF, Hoffman HJ, Humphreys RP, Becker L (1993) The long-term outcome after surgical treatment of dorsally exophytic brain-stem gliomas. J Neurosurg 78:859–863
Pollack IF, Stewart CF, Kocak M, Poussaint TY, Broniscer A, Banerjee A, Douglas JG, Kun LE, Boyett JM, Geyer JR (2011) A phase II study of gefitinib and irradiation in children with newly diagnosed brainstem gliomas: a report from the Pediatric Brain Tumor Consortium. Neuro Oncol 13:290–297
Ragheb JEF (2000) The surgical classification and management of brainstem tumors in children. Int Pediatr 15:6
Recinos PF, Sciubba DM, Jallo GI (2007) Brainstem tumors: where are we today? Pediatr Neurosurg 43:192–201
Rineer J, Schreiber D, Choi K, Rotman M (2010) Characterization and outcomes of infratentorial malignant glioma: a population-based study using the Surveillance Epidemiology and End-Results database. Radiother Oncol 95:321–326
Sandri A, Sardi N, Genitori L, Giordano F, Peretta P, Basso ME, Bertin D, Mastrodicasa L, Todisco L, Mussa F, Forni M, Ricardi U, Cordero di Montezemolo L, Madon E (2006) Diffuse and focal brain stem tumors in childhood: prognostic factors and surgical outcome. Experience in a single institution. Childs Nerv Syst 22:1127–1135
Sanford RA, Freeman CR, Burger P, Cohen ME (1988) Prognostic criteria for experimental protocols in pediatric brainstem gliomas. Surg Neurol 30:276–280
Smith MA, Freidlin B, Ries LA, Simon R (1998) Trends in reported incidence of primary malignant brain tumors in children in the United States. J Natl Cancer Inst 90:1269–1277
Squires LA, Allen JC, Abbott R, Epstein FJ (1994) Focal tectal tumors: management and prognosis. Neurology 44:953–956
Stokland T, Liu JF, Ironside JW, Ellison DW, Taylor R, Robinson KJ, Picton SV, Walker DA (2010) A multivariate analysis of factors determining tumor progression in childhood low-grade glioma: a population-based cohort study (CCLG CNS9702). Neuro Oncol 12:1257–1268
Suri A, Chabbra RP, Mehta VS, Gaikwad S, Pandey RM (2003) Effect of intramedullary signal changes on the surgical outcome of patients with cervical spondylotic myelopathy. Spine J 3:33–45
Walker DA, Punt JA, Sokal M (1999) Clinical management of brain stem glioma. Arch Dis Child 80:558–564
Yazici N, Varan A, Soylemezoglu F, Zorlu F, Kutluk T, Akyuz C, Buyukpamukcu M (2009) Pineal region tumors in children: a single center experience. Neuropediatrics 40:15–21
Zarghooni M, Bartels U, Lee E, Buczkowicz P, Morrison A, Huang A, Bouffet E, Hawkins C (2010) Whole-genome profiling of pediatric diffuse intrinsic pontine gliomas highlights platelet-derived growth factor receptor alpha and poly (ADP-ribose) polymerase as potential therapeutic targets. J Clin Oncol 28:1337–1344
Acknowledgments
The study is supported by the National Natural Science Foundation of China for Weiqing Wan (no. 81172192).
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Oliver Bozinov, Zurich, Switzerland
The article “Clinical outcomes and natural history of pediatric brainstem tumors: with 33 cases follow-ups” by Tao Sun et al. is a series of brainstem gliomas in a pediatric population with and without treatment. The study was performed in a retrospective way, and conclusions were drawn based on their single-center results. This is a 5-year series with 42 pediatric patients, but only 33 children were included because of missing medical records or failed histological proof. Regarding this special illness, such a series is still considered large. However, the histology and especially the natural course of these patients remain very heterogeneous. The presented Kaplan–Meier curves illustrate very nicely such a course of progression and survival. I still do not agree completely how the conclusion is drawn, that prolonged survival is achieved by surgery. The authors have not proved this scientifically as both groups are very heterogeneous. I agree that surgery in selected (benign) cases should be considered and most likely prolongs life, but the authors could not prove this in a homogenous group statistically. Most likely, such a difficult answer can only be achieved in a multicenter prospective study, which will be a very difficult task. My conclusion based on the presented data is that focal gliomas lead to more surgical interventions and seem to have a prolonged survival outcome in an interdisciplinary approach; thus, careful surgery remains a therapy of choice in selected cases of pediatric brainstem gliomas.
James T. Rutka, Toronto, Canada
The authors have reviewed their experience over 5 years with 42 children with brainstem tumours. The overall median survival of this series was 11 months. Children who had a focal brainstem tumour did better in terms of survival after surgery. It is critical these days to categorize paediatric brainstem tumours into their recognized subgroups primarily based on location by MRI. These categories include: focal midbrain (tectal or tegmental) gliomas, dorsally exophytic pontine, focal pontine, and diffuse intrinsic pontine gliomas; and cervicomedullary brainstem gliomas. Surgery is rarely offered for tectal gliomas, except for CSF diversionary procedures to overcome hydrocephalus, and for diffuse intrinsic pontine gliomas, unless there are some atypical features about these tumours which mandate a biopsy. The gliomas in other locations of the brainstem frequently require neurosurgical approaches and resection. Sadly, the diffuse intrinsic pontine glioma, which is the most aggressive and fatal tumour, is the most common of all paediatric brainstem gliomas.
The authors performed surgery for the most part on the focal brainstem tumours which is a suggested treatment option. The use of advanced microneurosurgical techniques, intraoperative neuromonitoring, and neuronavigation can provide the required safety to ensure that patients will not suffer undue consequences neurologically from surgery. For patients with focal tegmental midbrain gliomas which are pilocytic astrocytomas, surgery alone can be curative, and the authors have shown us such a case.
The future of paediatric brainstem gliomas will be to develop an increased understanding of the molecular genetics of the diffuse gliomas, as these are the lesions that require our utmost attention and help. Fortunately, a number of clinical trials are evolving throughout the world where procurement of tissue will be mandated, and sophisticated high-resolution genotyping of these tumours will be performed. This will then lead us to improved therapies for these tumours with rather dismal prognosis at this time.
Dr. Sun and Dr. Wan contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Sun, T., Wan, W., Wu, Z. et al. Clinical outcomes and natural history of pediatric brainstem tumors: with 33 cases follow-ups. Neurosurg Rev 36, 311–320 (2013). https://doi.org/10.1007/s10143-012-0428-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0428-8