Abstract
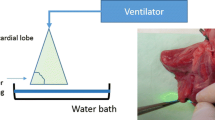
A diode-pump Nd:YAG high-power laser (wavelength 1320 nm, power 100 W) is routinely used to surgically remove lung metastases. Even pulmonary lesions in central locations are resectable via this method, yet it also carries a potential risk of damaging the larger bronchi and vessels in the vicinity. Studies investigating the safety of using high-power lasers are lacking. We therefore aimed to examine the direct effects of a 100-watt laser on the bronchi and pulmonary artery at a standard working velocity. From freshly slaughtered pigs, we isolated cylindrical specimens of the trachea, the main and lobar bronchi, and the central pulmonary artery from the both lungs. These specimens were fixed consecutively in rows behind each other on a Styrofoam surface in the laboratory. The laser’s handle was clamped into a hydraulic feed unit so that the laser was focused at constant distance perpendicular to the tissue and would move at 10 mm/s over the specimens. The Nd:YAG Laser LIMAX® 120 functioned at a consistent power of 100 W during all the experiments. The lasered specimens were examined macroscopically and histologically for tissue damage. None of the trachea or bronchial walls were perforated. Compared to the pulmonary parenchyma, we observed no vaporization effects—only minor superficial coagulation (with a mean depth of 2.1 ± 0.8 mm). This finding was histologically confirmed in each specimen, which revealed mild superficial coagulation and no damage to the cartilage. In the presence of a residual peribronchial fatty tissue, the laser effect was even attenuated. The pulmonary arteries presented no lumen openings whatsoever, merely a discrete trace of coagulation. The vessel wall revealed increased vacuolization without alteration of the remaining vessel wall. In conclusion, laser resection at 100 W of the central lung areas is safe with respect to airways and blood vessels and the laser output does not need to be reduced when treating these areas.






Similar content being viewed by others
References
Internullo E et al (2008) Pulmonary metastasectomy: a survey of current practice amongst members of the European Society of Thoracic Surgeons. J Thorac Oncol 3(11):1257–1266
Osei-Agyemang T, Ploenes T, Passlick B (2012) Pulmonary metastasectomy: indication and technique. Zentralbl Chir 137(3):234–241
Erhunmwunsee L, D’Amico TA (2009) Surgical management of pulmonary metastases. Ann Thorac Surg 88(6):2052–2060
Pfannschmidt J, Dienemann H (2009) Current surgical management of pulmonary metastases. Zentralbl Chir 134(5):418–424
Rolle A, Kozlowski M (2005) Laser resection of lung parenchyma—a new technical and clinical approach. Rocz Akad Med Bialymst 50:193–196
Treasure T (2007) Pulmonary metastasectomy: a common practice based on weak evidence. Ann R Coll Surg Engl 89(8):744–748
Scanagatta P et al (2012) Pulmonary resections: cytostructural effects of different-wavelength lasers versus electrocautery. Tumori 98(1):90–93
Kirschbaum A et al (2012) Local effects of high-powered neodymium-doped yttrium aluminium garnet laser systems on the pulmonary parenchyma: an experimental study on the isolated perfused pig lung lobe. Interact Cardiovasc Thorac Surg 15(2):191–193
Kawano R et al (2009) Primary lung cancer protruding into right main bronchus, successfully treated with endoscopic neodymium yttrium aluminum garnet (Nd-YAG) laser. Kyobu Geka 62(9):807–811
Perin B et al (2012) Patient-related independent clinical risk factors for early complications following Nd: YAG laser resection of lung cancer. Ann Thorac Med 7(4):233–237
Vodicka J et al (2009) Use of the KLS Martin Nd:YAG laser MY 40 13 in lung parenchyma surgery. Rozhl Chir 88(5):248–252
Lesser TG (2012) Laser application enables awake thoracoscopic resection of pulmonary nodules with minimal access. Surg Endosc 26(4):1181–1186
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were performed on slaughtered animals. An ethical approval was not needed.
Informed consent
Informed consent was not needed.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kirschbaum, A., Rexin, P., Bartsch, D.K. et al. Effect of high laser output on the central bronchi and pulmonary artery. Lasers Med Sci 32, 881–886 (2017). https://doi.org/10.1007/s10103-017-2188-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2188-8