Abstract
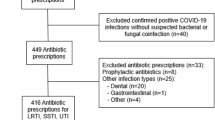
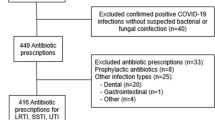
Inappropriate antibiotic use contributes to antimicrobial resistance. Multi-faceted antimicrobial stewardship programmes (ASPs) are recommended for sustainable changes in prescribing practices. A multi-disciplinary ASP was established in October 2008 and piloted in the Departments of General Surgery, Renal Medicine and Endocrinology sequentially. To improve the quality of patient care via optimising the (1) choice, (2) dose, (3) route and (4) duration of antibiotics, a “whole-system” approach incorporating prospective review with immediate concurrent feedback (ICF), prescriber education (public or individualised), de-escalation of therapy, dose optimisation and parenteral-to-oral conversion, while recognising the autonomy of primary prescribers, was adopted. The audited department received a quarterly outcomes report and any common unaccepted practices would be addressed. Outcomes were analysed for 12 months post-ASP implementation. A total of 1,535 antibiotic prescriptions were reviewed. Antimicrobial use in 376 (24.5%) prescriptions was inappropriate. Of 596 interventions made, 70.2% were accepted. A reduction in audited antibiotics consumption resulted in acquisition cost savings of S$198,575 for the hospital. Patients’ cost-savings attributable to ASP-initiated interventions were $91,194. The overall all-cause mortality rate and median monthly inpatient-days pre- and post-intervention remained stable. A “whole-system” ASP was effective in optimising antibiotic use in our hospital, without compromising clinical outcomes.



Similar content being viewed by others
References
National Nosocomial Infections Surveillance System (2004) National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 32:470–485
Hsu LY, Tan TY, Jureen R, Koh TH, Krishnan P, Tzer-Pin Lin R, Wen-Sin Tee N, Tambyah PA (2007) Antimicrobial drug resistance in Singapore hospitals. Emerg Infect Dis 13(12):1944–1947
Kwa AL, Low JG, Lee E, Kurup A, Chee HL, Tam VH (2007) The impact of multidrug resistance on the outcomes of critically ill patients with Gram-negative bacterial pneumonia. Diagn Microbiol Infect Dis 58(1):99–104
Hsu LY, Tan TY, Tam VH, Kwa A, Fisher DA, Koh TH, Network for Antimicrobial Resistance Surveillance (Singapore) (2010) Surveillance and correlation of antibiotic prescription and resistance of Gram-negative bacteria in Singaporean hospitals. Antimicrob Agents Chemother 54(3):1173–1178
Quek CL (2007) A retrospective study evaluating the use of imipenem and meropenem in a tertiary referral hospital in Singapore. Abstracts of Singapore General Hospital (SGH) 16th Annual Scientific Meeting, Singapore, 27–28 April 2007
Shlaes DM, Gerding DN, John JF Jr, Craig WA, Bornstein DL, Duncan RA, Eckman MR, Farrer WE, Greene WH, Lorian V, Levy S, McGowan JE Jr, Paul SM, Ruskin J, Tenover FC, Watanakunakorn C (1997) Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis 25:584–599
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM, Infectious Diseases Society of America, Society for Healthcare Epidemiology of America (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44:159–177
Lawton RM, Fridkin SK, Gaynes RP, McGowan JE Jr (2000) Practices to improve antimicrobial use at 47 US hospitals: the status of the 1997 SHEA/IDSA position paper recommendations. Society for Healthcare Epidemiology of America/Infectious Diseases Society of America. Infect Control Hosp Epidemiol 21(4):256–259
Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ (1989) Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med 321(19):1306–1311
Grol R (2001) Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 39(Suppl 2):II46–II54
Hulscher ME, Grol RP, van der Meer JW (2010) Antibiotic prescribing in hospitals: a social and behavioural scientific approach. Lancet Infect Dis 10:167–175
Charani E, Cooke J, Holmes A (2010) Antibiotic stewardship programmes—what’s missing? J Antimicrob Chemother 65:2275–2277
Ansari F, Gray K, Nathwani D, Phillips G, Ogston S, Ramsay C, Davey P (2003) Outcomes of an intervention to improve hospital antibiotic prescribing: interrupted time series with segmented regression analysis. J Antimicrob Chemother 52:842–848
Ng CK, Wu TC, Chan WM, Leung YS, Li CK, Tsang DN, Leung GM (2008) Clinical and economic impact of an antibiotics stewardship programme in a regional hospital in Hong Kong. Qual Saf Health Care 17(5):387–392
Raineri E, Pan A, Mondello P, Acquarolo A, Candiani A, Crema L (2008) Role of the infectious diseases specialist consultant on the appropriateness of antimicrobial therapy prescription in an intensive care unit. Am J Infect Control 36(4):283–290
Halm EA, Horowitz C, Silver A, Fein A, Dlugacz YD, Hirsch B, Chassin MR (2004) Limited impact of a multicenter intervention to improve the quality and efficiency of pneumonia care. Chest 126(1):100–107
Cosgrove SE, Patel A, Song XY, Miller RE, Speck K, Banowetz A, Hadler R, Sinkowitz-Cochran RL, Cardo DM, Srinivasan A (2007) Impact of different methods of feedback to clinicians after postprescription antimicrobial review based on the Centers for Disease Control and Prevention’s 12 Steps to Prevent Antimicrobial Resistance Among Hospitalized Adults. Infect Control Hosp Epidemiol 28(6):641–646
LaRocco A Jr (2003) Concurrent antibiotic review programs—a role for infectious diseases specialists at small community hospitals. Clin Infect Dis 37(5):742–743
Chia J (2011) The rise of the superbug. Singapore Health Services HealthXchange. Available online at: http://www.healthxchange.com.sg/healthyliving/SpecialFocus/Pages/The-rise-of-the-superbug.aspx. Last accessed 11th June 2011
Schentag JJ (1998) Antibiotic dosing—does one size fit all? JAMA 279:159–160
Tonna AP, Stewart D, West B, Gould I, McCaig D (2008) Antimicrobial optimisation in secondary care: the pharmacist as part of a multidisciplinary antimicrobial programme—a literature review. Int J Antimicrob Agents 31(6):511–517
American Society of Health System Pharmacists (ASHP) (2010) ASHP statement on the pharmacist’s role in antimicrobial stewardship and infection prevention and control. Am J Health Syst Pharm 67(7):575–577
Thaler R, Sunstein C (2008) Nudge: improving decisions about health, wealth and happiness. Yale University Press, New Haven, CT
Acknowledgements
The authors would like to thank Ms Yixin Liew, Ms Rachel Ong, Ms Yiying Cai, Ms Sarah Tang, Ms Cheryl Lim and Ms Noor'ain Bte Gulambas for their assistance in running the antimicrobial stewardship programme; and the physicians of the participating departments for their support of the programme. The results included in this manuscript were presented, in part, as an oral paper at the 12th Western Pacific Congress on Chemotherapy and Infectious Diseases, Singapore, 4 December 2010.
Transparency declarations
This work was supported by a grant from the SingHealth Foundation (SHF/IIC003/2009; $50,000). Dr. Andrea Kwa Lay Hoon and Ms. Winnie Lee have received funding for research from Johnson & Johnson (Janssen-Cilag), Merck Sharp & Dohme (I.A.) Corp and Pfizer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teo, J., Kwa, A.L.H., Loh, J. et al. The effect of a whole-system approach in an antimicrobial stewardship programme at the Singapore General Hospital. Eur J Clin Microbiol Infect Dis 31, 947–955 (2012). https://doi.org/10.1007/s10096-011-1391-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1391-y