Abstract
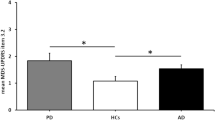
Parkinson’s disease (PD) patients frequently have an impairment of facial expression both in voluntary and spontaneous emotional expression. Aim of this study was to evaluate the feasibility of a rehabilitation program for hypomimia in patients with PD, comparing two different approaches. Thirty-six patients with PD were included: 20 patients received a rehabilitative intervention for hypomimia either with a DVD showing exercises focused on facial muscles (PD-group-A) or with a therapist-guided facial rehabilitation with a proprioceptive/recognition approach (PD-group-B). Sixteen patients (PD-Ctrl group) did not receive any treatment and served as control group. The feasibility of the proposed rehabilitation techniques was the main focus of this evaluation. We also evaluate the efficacy of the treatments by means of the sub-item 19 of the Unified Parkinson’s disease Rating Scale motor score (UPDRS-III) and by a computerized analysis of facial expression (E-Motion), which was assessed prior to (T0) and after therapy (T1). The proposed rehabilitative program for the treatment of hypomimia was shown to be feasible. Our data show a significant improvement in UPDRS-III sub-item 19 in PD-group-B compared to PD-group-A, (p = 0.005) and to PD-Ctrl (p = 0.003) and in expressivity of fear in PD-group-B compared to PD-Ctrl (p = 0.01). The proposed rehabilitative program showed to be feasible. A larger multi-center trial is now warranted to establish its efficacy to improve facial expression over long time period.

Similar content being viewed by others
References
Bologna M, Fabbrini G, Marsili L, Defazio G, Thompson PD, Berardelli A (2013) Facial Bradykinesia. J Neurol Neurosurg Psychiatry 84(6):681–685
Tickle-Degnen L, Lyons KD (2004) Practitioners impressions of patients with Parkinson’s disease: the social ecology of the expressive mask. Soc Sci Med 58(3):603–614
Metman LV, Myre B, Verwey N, Hassin-Baer S, Arzbaecher J, Sierens D, Bakay R (2004) Test- retest reliability of UPDRS-III, dyskinesia scales, and timed motor tests in patients with advanced Parkinson’s disease: an argument against multiple baseline assessments. Mov Disord 19(9):1079–1084
Katsikitis M, Pilowsky I (1996) A controlled study of facial mobility treatment in Parkinson’s disease. J Psychosom Res 40(4):387–396
Hughes AJ, Ben-Shlomo Y, Daniel SE, Lees AJ (1992) What features improve the accuracy of clinical diagnosis in Parkinson’s disease: a clinicopathologic study. Neurology 42(6):1142–1146
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17(5):427–442
Calvo MG, Beltrán D (2013) Recognition advantage of happy faces: tracing the neurocognitive processes. Neuropsychologia 51(11):2051–2061
Van de Winckel A, Sunaert S, Wenderoth N, Peeters R, Van Hecke P, Feys H, Horemans E, Marchal G, Swinnen SP, Perfetti C, De Weerdt W (2005) Passive somatosensory discrimination tasks in healthy volunteers: differential networks involved in familiar versus unfamiliar shape and length discrimination. Neuroimage 26(2):441–453 Epub 2005 Mar 24
Hastorf AH, Osgood CE, Ono H (1966) The semantics of facial expressions and the prediction of the meanings of stereoscopically fused facial expressions. Scand J Psychol 7(3):179–188
Lee AC, Tang SW, Yu GK, Cheung RT (2008) The smiley as a simple screening tool for depression after stroke: a preliminary study. Int J NursStud 45(7):1081–1089 Epub 2007 Aug 20
Said CP, Sebe N, Todorov A (2009) Structural resemblance to emotional expressions predicts evaluation of emotionally neutral faces. Emotion 9(2):260–264
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Gallese V, Fadiga L, Rizzolatti FL (1996) Action recognition in premotor cortex. Brain 119:593–609
Gallese V, Goldman A (1998) Mirror neurons and the simulation theory of mind-reading. Trends Cogn Sci 8:396–403
Jacobs DH, Shuren J, Bowers D, Heilman KM (1995) Emotional facial imagery, perception, and expression in Parkinson’s disease. Neurology 45(9):1696–1702
Ricciardi L, Bologna M, Morgante F, Ricciardi D, Morabito B, Volpe D, Martino D, Tessitore A, Pomponi M, Bentivoglio AR, Bernabei R, Fasano A (2015) Reduced facial expressiveness in Parkinson’s disease: a pure motor disorder? J Neurol Sci 358(1–2):125–130
Garrison KA, Winstein CJ, Aziz-Zadeh L (2010) The mirror neuron system: a neural substrate for methods in stroke rehabilitation. Neurorehabil Neural Repair. 24(5):404–412
Abbruzzese G, Berardelli A (2003) Sensorimotor integration in movement disorders. Mov Disord 18:231–240
Gibson JJ (1966) The senses considered as perceptual systems. Houghton Mifflin, Oxford
Abbruzzese G, Trompetto C, Mori L, Pelosin E (2014) Proprioceptive rehabilitation of upper limb dysfunction in movement disorders: a clinical perspective. Front Hum Neurosci. 25(8):961
Acknowledgments
I dedicate this note to Dario, Roberta and Marina, and to the memory of Ettore Grimaldi and Oscar Ravera.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Rights and permissions
About this article
Cite this article
Ricciardi, L., Baggio, P., Ricciardi, D. et al. Rehabilitation of hypomimia in Parkinson’s disease: a feasibility study of two different approaches. Neurol Sci 37, 431–436 (2016). https://doi.org/10.1007/s10072-015-2421-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-015-2421-9