Abstract
Background
The use of cyclooxygenase (COX) inhibitors is increasingly common. Most of them are available for self-medication, either as analgesic or for cardio- and cerebrovascular prevention.
Objectives
We aimed to analyze adverse drug events (ADE) related to COX inhibitors and the concomitant use of proton pump inhibitors (PPI) according to guidelines in patients presenting at an emergency department (ED).
Methods
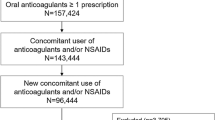
In a prospective study, 2262 patients presenting consecutively at the ED of a tertiary care university teaching hospital were evaluated by intensive chart review in order to detect and classify all ADE. In this cross-sectional analysis all patients taking COX inhibitors at home were evaluated further.
Results
Of all evaluated patients, 753 (33.3 %) took COX inhibitors at home, 258 (34.3 %) with concomitant PPI. A total of 168 (22.3 %) patients suffered from at least one ADE related to COX inhibitors. The most common ADE observed were anemia (55.9 %) and gastrointestinal ADE (31.6 %, e. g., bleeding, gastritis, and ulcer). In 10.1 % of patients, a medication error (e. g., intake without proper clinical indication) contributed to the ADE and in 40.8 % of the ADE involved further contributing drugs. Only 38.8–42.1 % of patients with a high gastrointestinal risk were prescribed a PPI concomitantly.
Conclusion
ADE related to COX inhibitors were found in every fifth patient taking COX inhibitors. One-tenth of all ADE involving COX inhibitors were related to medication errors. The guideline-based concomitant use of PPI was only in part implemented.
Zusammenfassung
Hintergrund
Cyclooxygenase (COX)-Hemmer werden immer häufiger angewendet. Viele sind zur Selbstmedikation erhältlich, entweder als Analgetikum oder zur kardio- und zerebrovaskulären Prävention.
Ziel der Arbeit
Ziel dieser Untersuchung war es, durch COX-Hemmer verursachte unerwünschte Arzneimittelereignisse (UAE) und die leitliniengerechte Begleitmedikation durch Protonenpumpenhemmer (PPI) zu analysieren.
Methode
In die prospektive Beobachtungsstudie wurden 2262 Patienten eingeschlossen, die sich konsekutiv in der zentralen Notaufnahme (ZNA) eines Schwerpunktversorgers vorstellten. Alle UAE wurden durch Intensivdokumentation erfasst und klassifiziert.
Ergebnis
Von allen evaluierten Patienten nahmen 753 (33,3 %) COX-Hemmer zuhause ein, 258 (34,3 %) zusammen mit einem PPI. Unter mindestens einer durch COX-Hemmer verursachten UAE litten 168 (22,3 %). Die am häufigsten beobachteten UAE waren Anämie (55,9 %) und gastrointestinale UAE (31,6 %, z. B. Blutungen, Gastritis und Ulkus). Bei 10,1 % der Patienten war ein Medikationsfehler (z. B. die Einnahme ohne bekannte Indikation) am UAE beteiligt, an 40,8 % aller UAE eine Interaktion. Nur 38,8–42,1 % aller Patienten mit hohem Risiko für gastrointestinale UAE erhielten begleitend ein PPI.
Diskussion
Bei jedem fünften Patienten, der NSAR einnahm, wurde eine durch COX-Hemmer verursachte UAE gefunden. An jeder zehnten UAE durch COX-Hemmer war ein Medikationsfehler beteiligt. Die leitliniengerechte begleitende Anwendung von PPI wurde nur zum Teil umgesetzt.


Similar content being viewed by others
References
Anglin R, Yuan Y, Moayyedi P et al (2014) Risk of upper gastrointestinal bleeding with selective serotonin reuptake inhibitors with or without concurrent nonsteroidal anti-inflammatory use: a systematic review and meta-analysis. Am J Gastroenterol 109:811–819
Arasaradnam RP, Woodward T, Parrack L et al (2003) Audit of proton pump inhibitor (PPI) prescribing: are NICE guidelines being followed? Clin Med 3:387–388
Bates DW, Leape LL, Petrycki S (1993) Incidence and preventability of adverse drug events in hospitalized adults. J Gen Intern Med 8:289–294
Böger R, Schmidt G (2012) Antirheumatika und Antiphlogistika. In: Schwabe U, Paffrath D (eds) Arzneiverordnungs-Report 2012. Springer, Berlin, pp 447–449
Bradley MC, Motterlini N, Padmanabhan S et al (2014) Potentially inappropriate prescribing among older people in the United Kingdom. BioMed Cent Geriatr 14:72
Brun J, Jones R (2001) Nonsteroidal anti-inflammatory drug-associated dyspepsia: the scale of the problem. Am J Med 110:12S–13S
Bürkle T, Müller F, Patapovas A et al (2013) A new approach to identify, classify and count drug-related events. Br J Clin Pharmacol 76(Suppl 1):56–68
Capuano A, Motola G, Russo F et al (2004) Adverse drug events in two emergency departments in Naples, Italy: an observational study. Pharmacol Res 50:631–636
Charlot M, Ahlehoff O, Norgaard ML et al (2010) Proton-pump inhibitors are associated with increased cardiovascular risk independent of clopidogrel use: a nationwide cohort study. Ann Intern Med 153:378–386
Ctis Common Terminology Criteria for adverse events. https://safetyprofiler-ctep.nci.nih.gov/CTC/CTC.aspx. Accessed 20 November 2013
De Jong HJ, Korevaar JC, Van Dijk L et al (2013) Suboptimal prescribing of proton-pump inhibitors in low-dose aspirin users: a cohort study in primary care. BMJ Open 3(7):e003044
Dormann H, Sonst A, Müller F et al (2013) Adverse drug events in older patients admitted as an emergency: the role of potentially inappropriate medication in elderly people (PRISCUS). Dtsch Arztebl Int 110:213–219
Dries AM, Richardson P, Cavazos J et al (2009) Therapeutic intent of proton pump inhibitor prescription among elderly nonsteroidal anti-inflammatory drug users. Aliment Pharmacol Ther 30:652–661
Fischbach W, Darius H, Gross M et al (2010) Concomitant use of platelet aggregation inhibitors and proton pump inhibitors (PPIs): Position paper of the German Society for Digestive and Metabolic Diseases (DGVS) and the German Society of Cardiology (DGK). Z Gastroenterol 48:1156–1163
Ghebremariam YT, Lependu P, Lee JC et al (2013) Unexpected effect of proton pump inhibitors: elevation of the cardiovascular risk factor asymmetric dimethylarginine. Circulation 128:845–853
Gnjidic D, Blyth FM, Le Couteur DG et al (2014) Non-steroidal anti-inflammatory drugs (NSAIDs) in older people: prescribing patterns according to pain prevalence and adherence to clinical guidelines. Pain 155:1814–1820
Hernández-Díaz S, García Rodríguez LA (2006) Cardioprotective aspirin users and their excess risk of upper gastrointestinal complications. BioMed Cent Med 4:22
Ito T, Jensen RT (2010) Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium. Curr Gastroenterol Rep 12:448–457
Karbach U, Schubert I, Hagemeister J et al (2011) Physicians’ knowledge of and compliance with guidelines: an exploratory study in cardiovascular diseases. Dtsch Arztebl Int 108:61–69
Kirchner M, Bürkle T, Patapovas A et al (2011) Building the technical infrastructure to support a study on drug safety in a general hospital. Stud Health Technol Inform 169:325–329
Ladd AM, Panagopoulos G, Cohen J et al (2014) Potential costs of inappropriate use of proton pump inhibitors. Am J Med Sci 347:446–451
Laine L, Connors L, Griffin MR et al (2009) Prescription rates of protective co-therapy for NSAID users at high GI risk and results of attempts to improve adherence to guidelines. Aliment Pharmacol Ther 30:767–774
Lanas A, Bajador E, Serrano P et al (2000) Nitrovasodilators, low-dose aspirin, other nonsteroidal antiinflammatory drugs, and the risk of upper gastrointestinal bleeding. N Engl J Med 343:834–839
Langman MJ, Weil J, Wainwright P et al (1994) Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet 343:1075–1078
Lanza FL, Chan FK, Quigley EM (2009) Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol 104:728–738
Masclee GM, Valkhoff VE, Coloma PM et al (2014) Risk for upper gastrointestinal bleeding from different drug combinations. Gastroenterology doi:10.1053/j.gastro.2014.06.007
Meier F, Maas R, Sonst A et al (2015) Adverse drug events in patients admitted to an emergency department: an analysis of direct costs. Pharmacoepidemiol Drug Saf 24:176–186
Müller F, Dormann H, Pfistermeister B et al (2014) Application of the Pareto principle to identify and address drug-therapy safety issues. Eur J Clin Pharmacol 70:727–736
Nebeker JR, Barach P, Samore MH (2004) Clarifying adverse drug events: a clinician’s guide to terminology, documentation, and reporting. Ann Intern Med 140:795–801
Patapovas A, Dormann H, Sedlmayr B et al (2013) Medication safety and knowledge-based functions: a stepwise approach against information overload. Br J Clin Pharmacol 76(Suppl 1):14–24
Schmiedl S, Rottenkolber M, Hasford J et al (2014) Self-Medication with over-the-counter and prescribed drugs causing adverse-drug-reaction-related hospital admissions: results of a prospective, long-term multi-centre study. Drug Saf 37:225–235
Sedlmayr B, Patapovas A, Kirchner M et al (2013) Comparative evaluation of different medication safety measures for the emergency department: physicians’ usage and acceptance of training, poster, checklist and computerized decision support. BMC Med Inform Decis Mak 13:79
The Uppsala Monitoring Centre The use of the WHO-UMC system for standardised case causality assessment. www.who-umc.org/Graphics/24734.pdf. Accessed 20 November 2013
Tielemans MM, Van Rossum LG, Eikendal T et al (2014) Gastrointestinal symptoms in NSAID users in an ‘average risk population’: results of a large population-based study in randomly selected Dutch inhabitants. Int J Clin Pract 68:512–519
Varga Z, Kriška M, Kristová V et al (2013) Analysis of non-steroidal anti-inflammatory drug use in hospitalized patients and perception of their risk. Interdiscip Toxicol 6:141–144
Vonkeman HE, Fernandes RW, Van De Laar MA (2007) Under-utilization of gastroprotective drugs in patients with NSAID-related ulcers. Int J Clin Pharmacol Ther 45:281–288
Wallace JL, Syer S, Denou E et al (2011) Proton pump inhibitors exacerbate NSAID-induced small intestinal injury by inducing dysbiosis. Gastroenterology 141:1314–1322
Wang YP, Chen YT, Tsai CF et al (2014) Short-term use of serotonin reuptake inhibitors and risk of upper gastrointestinal bleeding. Am J Psychiatry 171:54–61
Yeomans ND, Lanas AI, Talley NJ et al (2005) Prevalence and incidence of gastroduodenal ulcers during treatment with vascular protective doses of aspirin. Aliment Pharmacol Ther 22:795–801
Zhang S, Chao GQ, Lu B (2013) Proton pump inhibitors are not the key for therapying non-steroidal anti-inflammatory drugs-induced small intestinal injury. Rheumatol Int 33:2513–2521
Acknowledgements
We would like to thank board chairman Peter Krappmann and the business management committee of Fürth Hospital, led by Martin Vitzithum, for supporting the care research project and collaboration in designing the technical infrastructure for study conduct.
Medizinische Medien Informations GmbH (MMI, Neu-Isenburg, Germany) made its drug and drug interaction databases Pharmindex Plus® and OntoDrug® AMTS available to the study free of charge.
Sponsor
This research project was supported by The German Federal Ministry of Health within the “German Coalition for Patient Safety” by a BMG grant II A 5 – 2509 ATS 003 to HD, RM and TB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Müller holds shares in Novartis and has been an employee of Boehringer Ingelheim Pharma GmbH & Co. KG since 2014. B. Pfistermeister, H. Dormann, A. Patapovas, A. Sonst, H. Glaeser, B. Plank-Kiegele, T. Bürkle, and R. Maas state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or animals.
Additional information
B. Pfistermeister and H. Dormann contributed equally
Rights and permissions
About this article
Cite this article
Pfistermeister, B., Dormann, H., Patapovas, A. et al. Adverse drug events related to COX inhibitors in patients presenting at an emergency department. Notfall Rettungsmed 19, 671–678 (2016). https://doi.org/10.1007/s10049-016-0184-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10049-016-0184-3
Keywords
- Self medication
- Proton pump inhibitor
- Drug–drug interaction
- Gastrointestinal hemorrhage
- Cyclooxygenase inhibitors