Abstract
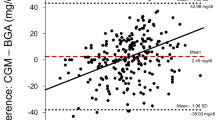
Although we have used an intravenous continuous glucose monitor for blood glucose management, a previous study reported that a subcutaneous continuous glucose monitor was also reliable for use in critically ill patients. The aim of this study was to compare the subcutaneous and intravenous continuous glucose monitors. This was an observational trial (UMIN-CTR, ID:000013338). We included patients who were admitted to our intensive care units (ICU) after hepato-biliary pancreatic surgery. Continuous blood glucose measurement was performed from the beginning of the operation to ICU discharge using the intravenous continuous monitor STG-55 (Nikkiso, Tokyo, Japan) and the subcutaneous continuous monitor iPro2 (Medtronic Japan, Tokyo, Japan). The STG-55 measured the glucose level in real time, and the iPro2 measured this every 5 min. We compared glucose levels obtained using the two devices every 5 min using a Bland–Altman plot and a regression analyses. A total of 3592 comparative samples in 15 cases were analyzed. The mean glucose level measured using the STG-55 was 139 ± 21 mg/dl, and that measured using the iPro2 was 144 ± 31 mg/dl. A linear regression line had the equation of the form y = 0.225x + 106. The coefficient of determination was 0.11, and the F-test significance level was set as p < 0.01. The mean of the differences was −5.2 mg/dl, with a 95 % agreement limit of −67 to + 57 mg/dL. The percent error was 44 %. In conclusion, the current study suggests that subcutaneous and intravenous continuous glucose monitoring was not highly correlated during either surgery or ICU stay.




Similar content being viewed by others
References
Hanazaki K, Maeda H, Okabayashi T. Tight perioperative glycemic control using an artificial endocrine pancreas. Surg Today. 2010;40:1–7.
Sebranek JJ, Lugli AK, Coursin DB. Glycaemic control in the perioperative period. Br J Anaesth. 2013;111(Suppl 1):i18–34.
Badawi O, Waite MD, Fuhrman SA, Zuckerman IH. Association between intensive care unit-acquired dysglycemia and in-hospital mortality. Crit Care Med. 2012;40:3180–8.
Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Taori G, Hegarty C, Bailey M. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010;85:217–24.
Mibu K, Yatabe T, Hanazaki K. Blood glucose control using an artificial pancreas reduces the workload of ICU nurses. J Artif Organ. 2012;15:71–6.
Yatabe T, Yamazaki R, Kitagawa H, Okabayashi T, Yamashita K, Hanazaki K, Yokoyama M. The evaluation of the ability of closed-loop glycemic control device to maintain the blood glucose concentration in intensive care unit patients. Crit Care Med. 2011;39:575–8.
Brunner R, Kitzberger R, Miehsler W, Herkner H, Madl C, Holzinger U. Accuracy and reliability of a subcutaneous continuous glucose-monitoring system in critically ill patients. Crit Care Med. 2011;39:659–64.
Sechterberger MK, van der Voort PH, Strasma PJ, DeVries JH. Accuracy of intra-arterial and subcutaneous continuous glucose monitoring in postoperative cardiac surgery patients in the ICU. J Diabetes Sci Technol. 2015;9:663–7.
van Hooijdonk RT, Leopold JH, Winters T, Binnekade JM, Juffermans NP, Horn J, Fischer JC, van Dongen-Lases EC, Schultz MJ. Point accuracy and reliability of an interstitial continuous glucose-monitoring device in critically ill patients: a prospective study. Crit Care. 2015;19:34.
Vriesendorp TM, DeVries JH, Holleman F, Dzoljic M, Hoekstra JB. The use of two continuous glucose sensors during and after surgery. Diabetes Technol Ther. 2005;7:315–22.
Yamashita K, Okabayashi T, Yokoyama T, Yatabe T, Maeda H, Manabe M, Hanazaki K. The accuracy of a continuous blood glucose monitor during surgery. Anesth Analg. 2008;106:160–3.
Yamashita K, Okabayashi T, Yokoyama T, Yatabe T, Maeda H, Manabe M, Hanazaki K. Accuracy and reliability of continuous blood glucose monitor in post-surgical patients. Acta Anaesthesiol Scand. 2009;53:66–71.
Signal M, Thomas F, Shaw GM, Chase JG. Complexity of continuous glucose monitoring data in critically ill patients: continuous glucose monitoring devices, sensor locations, and detrended fluctuation analysis methods. J Diabetes Sci Technol. 2013;7:1492–506.
International Standards Organization. In vitro diagnostic test systems-requirements for blood-glucose monitoring systems for self-testing in managing Diabetes mellitus. Reference number ISO 15197:2013. Geneva: International Organization for Standardization; 2013.
Jacobi J, Bircher N, Krinsley J, Agus M, Braithwaite SS, Deutschman C, Freire AX, Geehan D, Kohl B, Nasraway SA, Rigby M, Sands K, Schallom L, Taylor B, Umpierrez G, Mazuski J, Schunemann H. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med. 2012;40:3251–76.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Ellis MF, Benjamin K, Cornell M, Decker K, Farrell D, McGugan L, Porter GP, Shearin H, Zhao Y, Granger BB. Suitability of capillary blood glucose analysis in patients receiving vasopressors. Am J Crit Care. 2013;22:423–9.
Kanji S, Buffie J, Hutton B, Bunting PS, Singh A, McDonald K, Fergusson D, McIntyre LA, Hebert PC. Reliability of point-of-care testing for glucose measurement in critically ill adults. Crit Care Med. 2005;33:2778–85.
DuBose JJ, Inaba K, Branco BC, Barmparas G, Lam L, Teixeira PG, Belzberg H, Demetriades D. Discrepancies between capillary glucose measurements and traditional laboratory assessments in both shock and non-shock states after trauma. J Surg Res. 2012;178:820–6.
Boom DT, Sechterberger MK, Rijkenberg S, Kreder S, Bosman RJ, Wester JP, van Stijn I, DeVries JH, van der Voort PH. Insulin treatment guided by subcutaneous continuous glucose monitoring compared to frequent point-of-care measurement in critically ill patients: a randomized controlled trial. Crit Care. 2014;18:453.
Maeda H, Okabayashi T, Nishimori I, Yamashita K, Sugimoto T, Hanazaki K. Hyperglycemia during hepatic resection: continuous monitoring of blood glucose concentration. Am J Surg. 2010;199:8–13.
Yatabe T, Kitagawa H, Kawano T, Munekage M, Okabayashi T, Yamashita K, Hanazaki K, Yokoyama M. Continuous monitoring of glucose levels in the hepatic vein and systemic circulation during the Pringle maneuver in beagles. J Artif Organ. 2011;14:232–7.
Cengiz E, Tamborlane WV. A tale of two compartments: interstitial versus blood glucose monitoring. Diabetes Technol Ther. 2009;11(Suppl 1):S11–6.
Wernerman J, Desaive T, Finfer S, Foubert L, Furnary A, Holzinger U, Hovorka R, Joseph J, Kosiborod M, Krinsley J, Mesotten D, Nasraway S, Rooyackers O, Schultz MJ, Van Herpe T, Vigersky RA, Preiser JC. Continuous glucose control in the ICU: report of a 2013 round table meeting. Crit Care. 2014;18:226.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Munekage, M., Yatabe, T., Sakaguchi, M. et al. Comparison of subcutaneous and intravenous continuous glucose monitoring accuracy in an operating room and an intensive care unit. J Artif Organs 19, 159–166 (2016). https://doi.org/10.1007/s10047-015-0877-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-015-0877-2