Abstract
Introduction
Complex ventral hernia repair (VHR) is associated with a greater than 30 % wound complication rate. Perfusion mapping using indocyanine green fluorescence angiography (ICG-FA) has been demonstrated to predict skin and soft tissue necrosis in many reconstructive procedures; however, it has yet to be evaluated in VHR.
Methods
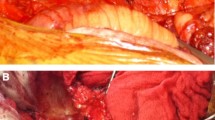
Patients undergoing complex VHR involving component separation and/or extensive subcutaneous advancement flaps were included in a prospective, blinded study. Patients with active infection were excluded. ICG-FA was performed prior to incision and prior to closure, but the surgeon was not allowed to view it. An additional blinded surgeon documented wound complications and evaluated postoperative photographs. The operative ICG-FA was reviewed blinded, and investigators were then unblinded to determine its ability to predict wound complications.
Results
Fifteen consecutive patients were enrolled with mean age of 56.1 years and average BMI of 34.9, of which 60 % were female. Most (73.3 %) had prior hernia repairs (average of 1.8 prior repairs). Mean defect area was 210.4 cm2, mean OR time was 206 min, 66.6 % of patients underwent concomitant panniculectomy, and 40 % had component separation. Mean follow-up was 7 months. Two patients developed wound breakdown requiring reoperation, while 1 had significant fat necrosis and another a wound infection, requiring operative intervention. ICG-FA was objectively reviewed and predicted all 4 wound complications. Of the 12 patients without complications, 1 had an area of low perfusion on ICG-FA. This study found a sensitivity of 100 % and specificity of 90.9 % for predicting wound complications using ICG-FA.
Conclusion
In complex VHR patients, subcutaneous perfusion mapping with ICG-FA is very sensitive and has the potential to reduce cost and improve patient quality of life by reducing wound complications and reoperation.






Similar content being viewed by others
References
Poulose BK et al (2012) Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 16(2):179–183
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237(1):129–135
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86(3):519–526
Albright E et al (2011) The component separation technique for hernia repair: a comparison of open and endoscopic techniques. Am Surg 77(7):839–843
Ko JH et al (2009) Abdominal wall reconstruction: lessons learned from 200 “components separation” procedures. Arch Surg 144(11):1047–1055
Huger WE Jr (1979) The anatomic rationale for abdominal lipectomy. Am Surg 45(9):612–617
Harth KC, Blatnik JA, Rosen MJ (2011) Optimum repair for massive ventral hernias in the morbidly obese patient–is panniculectomy helpful? Am J Surg 201(3):396–400 discussion 400
Saxe A et al (2008) Simultaneous panniculectomy and ventral hernia repair following weight reduction after gastric bypass surgery: is it safe? Obes Surg 18(2):192–195 discussion 196
Downey SE et al (2005) Review of technique for combined closed incisional hernia repair and panniculectomy status post-open bariatric surgery. Surg Obes Relat Dis 1(5):458–461
Leevy CM, Stein SW, Cherrick GR, Davidson CS (1959) Indocyanine green clearence: a test of liver excretory function. Clin Res 7:290–294
Flower RW, Hochheimer BF (1972) Clinical infrared absorption angiography of the choroid. Am J Ophthalmol 73(3):458–459
Eren S et al (1995) Assessment of microcirculation of an axial skin flap using indocyanine green fluorescence angiography. Plast Reconstr Surg 96(7):1636–1649
Rubben A et al (1994) Infrared videoangiofluorography of the skin with indocyanine green–rat random cutaneous flap model and results in man. Microvasc Res 47(2):240–251
Holm C et al (2002) Monitoring free flaps using laser-induced fluorescence of indocyanine green: a preliminary experience. Microsurgery 22(7):278–287
Holm C et al (2002) Intraoperative evaluation of skin-flap viability using laser-induced fluorescence of indocyanine green. Br J Plast Surg 55(8):635–644
Still J et al (1999) Evaluation of the circulation of reconstructive flaps using laser-induced fluorescence of indocyanine green. Ann Plast Surg 42(3):266–274
Desai ND et al (2006) A randomized comparison of intraoperative indocyanine green angiography and transit-time flow measurement to detect technical errors in coronary bypass grafts. J Thorac Cardiovasc Surg 132(3):585–594
Takahashi M et al (2004) SPY: an innovative intra-operative imaging system to evaluate graft patency during off-pump coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 3(3):479–483
Sanchez EQ et al (2008) Intraoperative imaging of pancreas transplant allografts using indocyanine green with laser fluorescence. Proc (Bayl Univ Med Cent) 21(3):258–260
Sekijima M et al (2004) An intraoperative fluorescent imaging system in organ transplantation. Transplant Proc 36(7):2188–2190
Stanga PE, Lim JI, Hamilton P (2003) Indocyanine green angiography in chorioretinal diseases: indications and interpretation: an evidence-based update. Ophthalmology 110(1):15–21 quiz 22–3
Gurtner GC et al (2013) Intraoperative laser angiography using the SPY system: review of the literature and recommendations for use. Ann Surg Innov Res 7(1):1
Phillips BT et al (2012) Intraoperative perfusion techniques can accurately predict mastectomy skin flap necrosis in breast reconstruction: results of a prospective trial. Plast Reconstr Surg 129(5):778e–788e
Moyer HR, Losken A (2012) Predicting mastectomy skin flap necrosis with indocyanine green angiography: the gray area defined. Plast Reconstr Surg 129(5):1043–1048
Newman MI et al (2011) An investigation of the application of laser-assisted indocyanine green fluorescent dye angiography in pedicle transverse rectus abdominus myocutaneous breast reconstruction. Can J Plast Surg 19(1):e1–e5
Komorowska-Timek E, Gurtner GC (2010) Intraoperative perfusion mapping with laser-assisted indocyanine green imaging can predict and prevent complications in immediate breast reconstruction. Plast Reconstr Surg 125(4):1065–1073
Pestana IA et al (2009) Early experience with fluorescent angiography in free-tissue transfer reconstruction. Plast Reconstr Surg 123(4):1239–1244
Azuma R et al (2008) Detection of skin perforators by indocyanine green fluorescence nearly infrared angiography. Plast Reconstr Surg 122(4):1062–1067
Giunta RE et al (2005) Prediction of flap necrosis with laser induced indocyanine green fluorescence in a rat model. Br J Plast Surg 58(5):695–701
Wang HD, Singh DP (2012) The use of indocyanine green angiography to prevent wound complications in ventral hernia repair with open components separation technique. Hernia 17(3):397–402
Benya R, Quintana J, Brundage B (1989) Adverse reactions to indocyanine green: a case report and a review of the literature. Cathet Cardiovasc Diagn 17(4):231–233
Ishihara H et al (1998) Detection of capillary protein leakage by glucose and indocyanine green dilutions during the early post-burn period. Burns 24(6):525–531
Lifecell corp (2012) SPY Elite intraoperative perfusion assessment system: SPY Elite Pack and SPY Elite Kit Instructions for Use. Branchburg, Lifecell corp
Iseki K et al (1980) Shock caused by indocyanine green dye in chronic hemodialysis patients. Clin Nephrol 14(4):210
Hope-Ross M et al (1994) Adverse reactions due to indocyanine green. Ophthalmology 101(3):529–533
Newman MI, Samson MC (2009) The application of laser-assisted indocyanine green fluorescent dye angiography in microsurgical breast reconstruction. J Reconstr Microsurg 25(1):21–26
Keats AS (1978) The ASA classification of physical status–a recapitulation. Anesthesiology 49(4):233–236
Harris PA et al (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Jones RS, Brown C, Opelka F (2005) Surgeon compensation: “Pay for performance,” the American College of Surgeons National Surgical Quality Improvement Program, the Surgical Care Improvement Program, and other considerations. Surgery 138(5):829–836
Novitsky YW et al (2006) Open preperitoneal retrofascial mesh repair for multiply recurrent ventral incisional hernias. J Am Coll Surg 203(3):283–289
Patel KM et al (2013) Use of intraoperative indocyanin-green angiography to minimize wound healing complications in abdominal wall reconstruction. J Plast Surg Hand Surg 47(6):476–480
American Burn Association (1990) Hospital and prehospital resources for optimal care of patients with burn injury: guidelines for development and operation of burn centers. J Burn Care Rehabil 11(2):98–104
Mothes H et al (2004) Indocyanine-green fluorescence video angiography used clinically to evaluate tissue perfusion in microsurgery. J Trauma 57(5):1018–1024
McEvoy GK (ed) (1988) Cardiac function. Indocyanine green. Drug info 88: American Hospital Formulary Service. American Society of Hospital Pharmacists, Bethesda, pp 1190–1191
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study was conducted with a grant from LifeCell for materials only. PC declares no other conflicts of interest. BW declares no other conflicts of interest. IB declares no pertinent conflicts of interest, but is a speaker for W. L. Gore and Lifecell. AL declares no other conflicts of interest. SG declares no other conflicts of interest. BH has received grants from LifeCell and W. L. Gore. BH has received personal fees from W. L. Gore, LifeCell, Ethicon, and Davol. VA is a consultant for LifeCell.
Rights and permissions
About this article
Cite this article
Colavita, P.D., Wormer, B.A., Belyansky, I. et al. Intraoperative indocyanine green fluorescence angiography to predict wound complications in complex ventral hernia repair. Hernia 20, 139–149 (2016). https://doi.org/10.1007/s10029-015-1411-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-015-1411-4