Abstract
Background
The diagnostic and therapeutic procedures performed in a series of patients with primary parapharyngeal space (PPS) tumours treated at the ENT Departments of San Giovanni Bosco Hospital, Turin, and of the Pugliese-Ciaccio Hospital, Catanzaro, Italy, in the period 2001–2010 are evaluated.
Materials and methods
The retrospective review included 20 patients, 11 male and 9 female, average age of 41 years operated on for 21 primary PPS tumours. The most common tumours found were neurogenic neoplasms, while those of salivary origin were the next most common.
Results
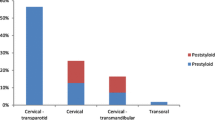
There were 14 paragangliomas (7 originating from carotid glomus, 5 from vagal and 2 from tympanicum), 1 sympathetic chain schwannoma and 6 pleomorphic adenomas. All the tumours were benign in nature and gave rise to few signs or symptoms. Patients underwent preoperative computed tomography (CT) scan or magnetic resonance imaging (MRI) or both. Most contrast-enhanced masses were submitted to some type of angiography. Most of the surgeries were planned through imaging alone, as preoperative fine needle aspiration (FNA) biopsy was performed only in six cases. Four different approaches were adopted for tumour removal: transcervical, transcervical/transparotid, cervical-transparotid-transmandibular and infratemporal fossa approach. There was no operative mortality, though neurologic morbidity was significant. Follow-up, extended to a maximum of 11 years, did not reveal any recurrences. In conclusion, neurogenic tumours may be the most common of PPS masses. Surgery is the mainstay treatment and external approaches offer the potential for satisfactory tumour resection. Of such external approaches, transcervical and cervical/transparotid are the most often used in benign forms.
Conclusion
The number of perioperative complications encountered in this series confirms the difficulty of performing surgery in this complex area, even in benign cases. The chances of avoiding vascular damage and saving the trunks or most of the nerve fibres involved depend not only on the skill and experience of the surgeon but also on the anatomy of the lesion, the type of connection between the tumour and the nerve from which it originates and the distribution of neural fibres in or around the tumour mass.



Similar content being viewed by others
References
Allison RS, Van der Waal I, Snow GB (1989) Parapharyngeal tumours: a review of 23 cases. Clin Otolaryngol Allied Sci 14:199–203
Hughes KV, Olsen RD, McCaffrey TV (1995) Parapharyngeal space neoplasms. Head Neck 17:124–130
Luna-Ortiz K, Navarrete-Aleman JE, Granados-Garcia M, Herrera-Gomez A (2005) Primary parapharyngeal space tumours in a Mexican cancer centre. Otolaryngol Head Neck Surg 132:587–591
Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. Diagnosis and treatment of the parapharyngeal space tumors. Pediatrics central 25:676-8.2011
Köhler HF, Carvalho AL, Mattos Granja NV, Nishinari K, Kowalski LP (2004) Surgical treatment of paragangliomas of the carotid bifurcation: results of 36 patients. Head Neck 26:1058–1063
Som PM, Sacher M, Stollmann A, Biller H, Lawson W (1988) Common tumors of the parapharyngeal space-imaging diagnosis. Head Neck Radiol 169:81–85
Gourin CG in AD Meyers: Parapharyngeal space tumors treatment and management. emedicine Medscape com/849385
Shahinian H, Dornier C, Fish U (1995) Parapharyngeal space tumors: the infratemporal fossa approach. Skull Base Surg 5:73–81
Sergi B, Limongelli A, Scarano E, Fetoni AR, Paludetti G (2008) Giant deep lobe parotid gland pleomorphic adenoma involving the parapharyngeal space. Report of three cases and review of the diagnostic and therapeutic approaches. Acta Otorhinolaryngol Ital 28:261–265
Papadogeorgakis N, Petsinis V, Goutzanis L, Kostakis G, Alexandridis C (2010) Parapharyngeal space tumors: surgical approaches in a series of 13 cases. Int J Oral Maxillofac Surg 39:243–250
Fisch U (1978) Infratemporal fossa approach to tumours of the temporal bone and base of the skull. J Laryngol Otol 92(11):949–967
Myers EN, Johnson JT, Curtin HG (2003) Tumors of parapharyngeal space. In: Myers EN, Suen JY, Myers JN, Hanna EY (eds) Cancer of the Head and Neck, vol 22, 4th edn. WB Saunders, Philadelphia, pp 511–513
Khafif A, Segev Y, Kaplan DM, Gil Z, Fliss DM (2005) Surgical management of parapharyngealspace tumors: a 10years review. Otolaryngol Head Neck Surg 132:401–406
Bozza F, Vigili MG, Ruscito P, Marzetti A, Marzetti F (2009) Surgical management of parapharyngeal space tumours: results of 10-years follow-up. Acta Othorinolaryngol Ital 29:10–15
Dimitrijevic MV, Jesic SD, Mikic AA, Arsovic NA, Tomanovic RM (2010) Parapharyngeal spacetumours: 61 cases review. Int J Oral Maxillofac Surg 39(19):983–989
Shoss SM, Donovan DT, Alford BR (1985) Tumours of the parapharybgeal space. Arch Otolaryngol 111:753–757
Carrau RL, Myers EN, Johnson JT (1999) Management of tumors arising in the parapharyngeal space. Laryngoscope 100:583–589
Tincani AJ, Martin AS, Altemani A, Scanavini Jr. RC, Barreto G, Lage HT, Valerio JB, Molina G (1999) Parapharyngeal space tumours: considerations in 26 cases. Sao Paulo Med J 117(1):34–37
Riitesh S, Rashmi J, Nita K, Shelley C, Ashish MK (2009) Paraphqaryngeal space tumors: a review of 10-Year Experience. Int J Pathol 8(2)
Zhi K, Ren H, Zhou Y, Wen Y, Zhang Y (2009) Management of parapharyngeal space tumours. J Oral Maxillofac Surg 67:1239–1244
Pang KP, Goh CHK, Tan HM (2002) Parapharyngeal Space Tumors: an 18years review. J Laryngol Otol 116:170–175
Wenhao R, Lu Z, Ling G, Hong Z, Keqian Z, Shaa X (2010) Letters to editor. In reply. J Oral Maxillofac Surg 68:1209–1214
Sanna M, Jain Y, de Donato G (2004) Management of jugular paragangliomas: the Gruppo Otologico experience. Otol Neurotol 25:797–804
Cosetti M, Linstrom C, Alexiades G, Tessema B, Parisier S (2008) Glomus tumors in patients of advanced age: a conservative approach. Laryngoscope 118:270
Miller RB, Boon MS, Atkins JP, Lowry LD (2000) Vagal paraganglioma: the Jefferson experience. Otolaryngol Head Neck Surg 122:482–487
Miani S, Boneschi R, Erba M, Giordanengo F (1993) Il paraganglioma vagale. Minerva Chir 48:1449–1453
Biller HF, Lawson W, Som P, Rosenfeld R (1989) Glomus vagale tumors. Ann Otol Rhinol Laryngol 98:21–26
Barnes I, Taylor SR (1990) Carotid body paragangliomas. A clinic-pathologic and DNA analysis of tumours. Arch Otolaryngol Head and Neck Surg 116:447–453
Machado N, Ryan N, Rao BH (1991) Vagal paraganglioma (two case reports). J Postgrad Med 37:56–58, 58A
Toshiki T (2009) Diagnosis and treatment of CSCS: a review of 9 cases. Acta Otolaryngol 129:324–329
Hinerman RW, Mendenhall WM, Amdur RJ, Stringer SP, Antonelli PJ, Cassisi NJ (2001) Definitive radiotherapy in the management of chemodectomas arising in the temporal bone, carotid body and glomus vagale. Head Neck 23:363–371
Weissman JI (2000) Case 21: Glomus Vagale Tumour. Radiology 215:237–242
Valdagni R, Amichetti M (1990) Radiation therapy of carotid body tumors. Am J Clin Oncol 13:45
Cole JM, Beiler D (1994) Long-term results of treatment for glomus jugulare and glomus vagale tumors with radiotherapy. Laryngoscope 4:1461–1465
Patetsios P, Gable DR, Garrett WV et al (2002) Management of carotid body paragangliomas and review of a 30-year experience. Ann Vasc Surg 16:331–338
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caldarelli, C., Bucolo, S., Spisni, R. et al. Primary parapharyngeal tumours: a review of 21 cases. Oral Maxillofac Surg 18, 283–292 (2014). https://doi.org/10.1007/s10006-014-0451-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-014-0451-8