Abstract
Objectives
Previous investigations have confirmed that every fifth dental patient suffers from clinically significant depressive symptoms. However, the putative impact of depressive symptoms on the prosthetic status has not been addressed in these studies. The objective of this study was to investigate the association between depressive symptoms and prosthetic status based on data from the Study of Health in Pomerania (SHIP-0).
Methods
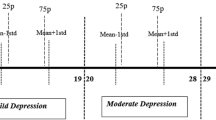
Data from 2,135 participants aged 30 to 59 years were analyzed. A classification (six classes regarding the number and position of missing teeth per jaw) was used to identify the degree of prosthetic status (no/suboptimal/optimal tooth replacement). The presence of depressive symptoms was assessed with a modified version of von Zerssen’s complaints scale. Screening for lifetime diagnoses of mental disorders was performed with the Composite International Diagnostic-Screener (CID-S). Multivariable logistic regressions including several confounders were calculated.
Results
A significant protective dose–response effect of depressive symptoms on prosthetic status was found only in men for the lower jaw [0–1 depressive symptoms: odds ratio (OR) = 3.84, 95 % confidence interval (CI, 1.65–8.92), p < 0.01; 2–3: OR = 2.87 (CI, 1.22–6.74), p < 0.05; reference, ≥8; adjusted for age, school education, smoking status, household income, marital status, living without a partner, risky alcohol consumption, obesity, diabetes, and physical activity]. There was no such association in women or for the upper jaw. The analyses using the CID-S confirmed these results.
Conclusions
In the lower jaw, men with depressive symptoms had a better prosthetic status than men without depressive symptoms suggesting a higher level of concern regarding their personal health.
Clinical relevance
If dentists might have an opportunity to identify men with depressive symptoms they can provide a wide range of treatment options that may enhance patients’ self-esteem and contribute to the patient’ well-being. Furthermore, depressive symptoms could indicate a discrepancy between self-perception of the dental health and the actual status which influence the dentists’ treatment decision making.

Similar content being viewed by others
References
Kressin NR, Spiro A 3rd, Atchison KA, Kazis L, Jones JA (2002) Is depressive symptomatology associated with worse oral functioning and well-being among older adults? J Public Health Dent 62(1):5–12
Slade GD, Spencer AJ, Locker D, Hunt RJ, Strauss RP, Beck JD (1996) Variations in the social impact of oral conditions among older adults in South Australia, Ontario, and North Carolina. J Dent Res 75(7):1439–1450
D’Mello DA (2003) Are your patients depressed? Implications for dental practice. J Mich Dent Assoc 85:26–32
Mundt T, Schwahn C, Mack F, Polzer I, Samietz S, Kocher T, Biffar R (2007) Risk indicators for missing teeth in working-age Pomeranians—an evaluation of high-risk populations. J Public Health Dent 67(4):243–249
Desvarieux M, Schwahn C, Volzke H, Demmer RT, Ludemann J, Kessler C, Jacobs DR Jr, John U, Kocher T (2004) Gender differences in the relationship between periodontal disease, tooth loss, and atherosclerosis. Stroke 35(9):2029–2035. doi:10.1161/01.STR.0000136767.71518.36
Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH (2010) Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes 8:126. doi:10.1186/1477-7525-8-126
Mack F, Schwahn C, Feine JS, Mundt T, Bernhardt O, John U, Kocher PT, Biffar R (2005) The impact of tooth loss on general health related to quality of life among elderly Pomeranians: results from the study of health in Pomerania (SHIP-O). Int J Prosthodont 18(5):414–419
Anttila S, Knuuttila M, Ylostalo P, Joukamaa M (2006) Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci 114(2):109–114
WHO (2000) International consortium in psychiatric epidemiology. Cross-national comparisons of the prevalences and correlates of mental disorders. Bull World Health Organ 78:413–426
Grabe HJ, Baumeister SE, John U, Freyberger HJ, Volzke H (2009) Association of mental distress with health care utilization and costs: a 5-year observation in a general population. Soc Psychiatry Psychiatr Epidemiol 44(10):835–844. doi:10.1007/s00127-009-0005-9
Pu C, Bai YM, Chou YJ (2012) The impact of self-rated health on medical care utilization for older people with depressive symptoms. Int J Geriatr Psychiatry. doi:10.1002/gps.3849
Simon GE, Katzelnick DJ (1997) Depression, use of medical services and cost-offset effects. J Psychosom Res 42(4):333–344
Locker D (2009) Self-esteem and socioeconomic disparities in self-perceived oral health. J Public Health Dent 69(1):1–8. doi:10.1111/j.1752-7325.2008.00087.x
Khokhar WA, Clifton A, Jones H, Tosh G (2011) Oral health advice for people with serious mental illness. Cochrane Database Syst Rev (11):CD008802. doi:10.1002/14651858.CD008802.pub2
Purandare N, Woods E, Butler S, Morris J, Vernon M, McCord JF, Burns A (2010) Dental health of community-living older people attending secondary healthcare: a cross-sectional comparison between those with and without diagnosed mental illness. Int Psychogeriatr 22(3):417–425. doi:10.1017/S1041610209991438
Fenwick JE, Batchelor PA, Samarawickrama DY (1998) Reasons for referral of very elderly patients to the community dental service in rural England and the implications for developing oral health care services. Gerodontology 15(2):67–72
Stewart R, Hirani V (2007) Dental health and cognitive impairment in an English national survey population. J Am Geriatr Soc 55(9):1410–1414. doi:10.1111/j.1532-5415.2007.01298.x
Wu B, Plassman BL, Liang J, Wei L (2007) Cognitive function and dental care utilization among community-dwelling older adults. Am J Public Health 97(12):2216–2221. doi:10.2105/AJPH.2007.109934
Al Quran F, Clifford T, Cooper C, Lamey PJ (2001) Influence of psychological factors on the acceptance of complete dentures. Gerodontology 18(1):35–40
Friedman N, Landesman HM, Wexler M (1987) The influences of fear, anxiety, and depression on the patient’s adaptive responses to complete dentures. Part I J Prosthet Dent 58(6):687–689
Friedman N, Landesman HM, Wexler M (1988) The influences of fear, anxiety, and depression on the patient’s adaptive responses to complete dentures. Part II. J Prosthet Dent 59(1):45–48
Hensel E, Gesch D, Biffar R, Bernhardt O, Kocher T, Splieth C, Born G, John U (2003) Study of Health in Pomerania (SHIP): a health survey in an East German region. Objectives and design of the oral health section. Quintessence Int 34(5):370–378
Volzke H, Alte D, Schmidt CO, Radke D, Lorbeer R, Friedrich N, Aumann N, Lau K, Piontek M, Born G, Havemann C, Ittermann T, Schipf S, Haring R, Baumeister SE, Wallaschofski H, Nauck M, Frick S, Arnold A, Junger M, Mayerle J, Kraft M, Lerch MM, Dorr M, Reffelmann T, Empen K, Felix SB, Obst A, Koch B, Glaser S, Ewert R, Fietze I, Penzel T, Doren M, Rathmann W, Haerting J, Hannemann M, Ropcke J, Schminke U, Jurgens C, Tost F, Rettig R, Kors JA, Ungerer S, Hegenscheid K, Kuhn JP, Kuhn J, Hosten N, Puls R, Henke J, Gloger O, Teumer A, Homuth G, Volker U, Schwahn C, Holtfreter B, Polzer I, Kohlmann T, Grabe HJ, Rosskopf D, Kroemer HK, Kocher T, Biffar R, John U, Hoffmann W (2011) Cohort profile: the study of health in pomerania. Int J Epidemiol 40(2):294–307. doi:10.1093/ije/dyp394
Keil U, Stieber J, Doring A, Chambless L, Hartel U, Filipiak B, Hense HW, Tietze M, Gostomzyk JG (1988) The cardiovascular risk factor profile in the study area Augsburg. Results from the first MONICA survey 1984/85. Acta Med Scand Suppl 728:119–128
John U, Greiner B, Hensel E, Ludemann J, Piek M, Sauer S, Adam C, Born G, Alte D, Greiser E, Haertel U, Hense HW, Haerting J, Willich S, Kessler C (2001) Study of Health in Pomerania (SHIP): a health examination survey in an east German region: objectives and design. Soz Praventivmed 46(3):186–194
Mundt T, Polzer I, Samietz S, Grabe HJ, Messerschmidt H, Doren M, Schwarz S, Kocher T, Biffar R, Schwahn C (2009) Socioeconomic indicators and prosthetic replacement of missing teeth in a working-age population—results of the Study of Health in Pomerania (SHIP). Community Dent Oral Epidemiol 37(2):104–115. doi:10.1111/j.1600-0528.2009.00463.x
Baltes PBMKE (1999) The Berlin Aging Study: aging from 70 to 100. Cambridge University Press, New York
Bauer M, Priebe S, Berghofer A, Bschor T, Kiesslinger U, Whybrow PC (2001) Subjective response to and tolerability of long-term supraphysiological doses of levothyroxine in refractory mood disorders. J Affect Disord 64(1):35–42
Von Zerssen D (1976) KD Beschwerden-Liste [complaints schedule]. Weinheim, Beltz
Grabe HJ, Volzke H, Ludemann J, Wolff B, Schwahn C, John U, Meng W, Freyberger HJ (2005) Mental and physical complaints in thyroid disorders in the general population. Acta Psychiatr Scand 112(4):286–293. doi:10.1111/j.1600-0447.2005.00586.x
Konerding U, Kohlmann T, Alte D, John U (2006) Subjective health complaints, health-related quality of life and physician visits: results of the study of health in Pomerania (SHIP). Soz Praventivmed 51(3):162–173
Wittchen H, Höfler M, Gander F (1999) Screening for mental disorders: performance of the Composite International Diagnostic-Screener (CID-S). Int J Meth Psychiat Res 8:59–70
McMunn A, Breeze E, Goodman A, Nazroo J, Oldfield Z (2006) Social determinants of health in older age. In: Marmot M, Wilkinson RG (eds) Social determinants of health. University Press, Oxford
D’Agostino RB Jr, D’Agostino RB Sr (2007) Estimating treatment effects using observational data. JAMA 297(3):314–316. doi:10.1001/jama.297.3.314
Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ (2007) Analysis of observational studies in the presence of treatment selection bias: effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA 297(3):278–285. doi:10.1001/jama.297.3.278
Rothman KJ (ed) (2002) Epidemiology: an introduction. Oxford University Press, New York
Knol MJ, van der Tweel I, Grobbee DE, Numans ME, Geerlings MI (2007) Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int J Epidemiol 36(5):1111–1118. doi:10.1093/ije/dym157
Wolfersdorf M, Rupprecht U (2009) Depressive disorders: diagnostics and treatment by the general practitioner. MMW Fortschr Med 151(14):107–110, quiz 112
Sheiham ACA, Maizels J (1997) The social impacts of dental disease. In: Slade GD (ed) Measuring oral health and quality of life. University of North Carolina, Dental Ecology, Chapel Hill (NC)
Branchi R, Boddi V, Corti D, Hardoy MJ (2001) Can a prosthesis cause psychological disturbances? J Oral Rehabil 28(12):1133–1138
Marbach JJ (1985) Psychosocial factors for failure to adapt to dental prostheses. Dent Clin North Am 29(1):215–233
Sato Y, Hamada S, Akagawa Y, Tsuga K (2000) A method for quantifying overall satisfaction of complete denture patients. J Oral Rehabil 27(11):952–957
Kent GG, Blinkhorn AS (1993) Psychologie in der Zahnheilkunde [Psychology in dentistry]. Hogrefe-Verlag für Psychologie, Göttingen-Bern-Toronto-Seatle
Birner U (1993) Psychologie in der Zahnmedizin [Psychology in dentistry]. Quintessenz, Berlin
Johnke G (1997) Klinische Psychologie in der zahnärztlichen Praxis [Clinical Psychology in dental practice]. Schlüter-Verlag, Hannover
John MT, Micheelis W, Steele JG (2007) Depression as a risk factor for denture dissatisfaction. J Dent Res 86(9):852–856
Acknowledgments
This study was supported by the German Federal Ministry for Education and Research (NBL3 program, reference 01 ZZ 0403).
SHIP is part of the Community Medicine Research Net (http://www.medizin.uni-greifswald.de/cm) of the University of Greifswald, Germany, which is funded by the German Federal Ministry of Education and Research (BMBF, grant no. 01ZZ96030); the Ministry for Cultural Affairs and the Ministry for Social Affairs of the Federal State of Mecklenburg–West Pomerania (SHIP; http://www.medizin.uni-greifswald.de/cm).
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Samietz, S.A., Kindler, S., Schwahn, C. et al. Impact of depressive symptoms on prosthetic status—results of the study of health in Pomerania (SHIP). Clin Oral Invest 17, 1191–1200 (2013). https://doi.org/10.1007/s00784-012-0806-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0806-1