Abstract
Background
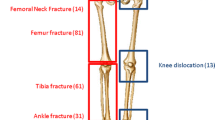
Trauma patients have the highest risk of developing venous thromboembolism (VTE) among hospitalised patients, with a reported 13-fold greater risk of developing VTE over non-trauma patients. This study examines the incidence of VTE and associated complications in trauma patients with lower limb fractures or injuries.
Methods
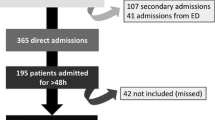
We retrospectively analysed 6,227 trauma patients and classified them according to injury severity score (ISS). The minor trauma group (ISS ≤15) contained 5,637 patients and the major trauma group (ISS >15) contained 590 patients.
Results
In the minor trauma group, VTE incidence was 1.17 %: 0.67 % were diagnosed with deep vein thrombosis (DVT) and 0.5 % with pulmonary embolism (PE). The readmission rate in the following 3-month period was 11 %, of which 2.8 % were subsequently rediagnosed with VTE. The 30-day mortality rate was 2.2 %. Seven patients died from PE following their initial admission and treatment, and another patient died from PE within three months after discharge. In the major trauma group, the VTE incidence was 6.8 %: 5.1 % with diagnosed with DVT and 1.7 % with PE. The readmission rate during the following three-month period was 6.6 %, of which 5 % were readmitted because of VTE and two cases were readmitted because of DVT. The overall 30-day mortality rate was 9.7 %, but no patients were formally diagnosed with a fatal case of PE.
Conclusion
This study found that major trauma patients have an approximate six-fold increased risk of developing VTE during admission compared with minor trauma patients (relative risk: 5.79; 95 % confidence interval: 3.94–8.49). Our findings support the use of extended prophylaxis to treat minor trauma patients.







Similar content being viewed by others
References
Rogers FB, Cipolle MD, Velmahos G, Rozycki G, Luchette FA. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002;53(1):142–64.
Meissner MH, Chandler WL, Elliott JS. Venous thromboembolism in trauma: a local manifestation of systemic hypercoagulability? J Trauma. 2003;54(2):224–31.
Khorana AA. The NCCN clinical practice guidelines on venous thromboembolic disease: strategies for improving VTE prophylaxis in hospitalized cancer patients. Oncologist. 2007;12(11):1361–70.
Rosendaal FR. Venous thrombosis: a multicausal disease. Lancet. 1999;353(9159):1167–73.
Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Forcier A. The prevalence of risk factors for venous thromboembolism among hospital patients. Arch Intern Med. 1992;152(8):1660–4.
Stannard JP, Lopez-Ben RR, Volgas DA, Anderson ER, Busbee M, Karr DK, McGwin GR Jr, Alonso JE. Prophylaxis against deep-vein thrombosis following trauma: a prospective, randomized comparison of mechanical and pharmacologic prophylaxis. J Bone Jt Surg Am. 2006;88(2):261–6.
Gearhart MM, Luchette FA, Proctor MC, Lutomski DM, Witsken C, James L, Davis K, Johannigman JA, Hurst JM, Frame SB. The risk assessment profile score identifies trauma patients at risk for deep vein thrombosis. Surgery. 2000;128:631–40.
Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331(24):1601–6.
Health N, Council MR. Clinical practice guideline for the prevention of venous thromboembolism in patients admitted to Australian hospitals. Canberra. 2009.
Kock HJ, Schmit-Neuerburg KP, Hanke J, Rudofsky G, Hirche H. Thromboprophylaxis with low-molecular-weight heparin in outpatients with plaster-cast immobilisation of the leg. Lancet. 1995;346(8973):459–61.
Cothren CC, Smith WR, Moore EE, Morgan SJ. Utility of once-daily dose of low-molecular-weight heparin to prevent venous thromboembolism in multisystem trauma patients. World J Surg. 2007;31(1):98–104.
Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, Granger C, Ohman EM, Dalen JE. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest. 2001;119(1 Suppl):64S–94S.
Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen, Colwell CW, Ray JG. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(Suppl 3):338S–400S.
Green D, Lee MY, Lim AC, Chmiel JS, Vetter M, Pang T, Chen D, Fenton L, Yarkony GM, Meyer PR Jr. Prevention of thromboembolism after spinal cord injury using low-molecular-weight heparin. Ann Intern Med. 1990;113(8):571–4.
Knudson MM, Morabito D, Paiement GD, Shackleford S. Use of low molecular weight heparin in preventing thromboembolism in trauma patients. J Trauma. 1996;41(3):446–59.
Tsiridis E, George M, Hamilton-Baillie D, Gamie Z, Upadhyay N, Giannoudis P. The efficacy and safety of enoxaparin following acetabular and pelvic fractures. 2009;91-B(SUPP_I):25.
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW, American College of chest P. Prevention of venous thromboembolism: American college of chest physicians evidence-based clinical practice guidelines (8th Edition). Chest. 2008;133(Suppl 6):381S–453S.
Network SIG. Prophylaxis of venous thromboembolism. 2002.
Anderson FA Jr, White K, Hip, Knee Registry I. Prolonged prophylaxis in orthopedic surgery: insights from the United States. Semin Thromb Hemost. 2002;28(Suppl 3):43–6.
Eriksson BI, Lassen MR. Investigators PEiH-FSP. Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery: a multicenter, randomized, placebo-controlled, double-blind study. Arch Intern Med. 2003;163(11):1337–42.
Kolb G, Bodamer I, Galster H, Seidlmayer C, Grambach K, Koudela K, Eisele RR, Becker C, Paal V, Spannagel U, Brom J, Weidinger G, Long-term Thromboprophylaxis Study G. Reduction of venous thromboembolism following prolonged prophylaxis with the low molecular weight heparin Certoparin after endoprothetic joint replacement or osteosynthesis of the lower limb in elderly patients. Thromb Haemost. 2003;90(6):1100–5.
Thaler HW, Roller RE, Greiner N, Sim E, Korninger C. Thromboprophylaxis with 60 mg enoxaparin is safe in hip trauma surgery. J Trauma. 2001;51(3):518–21.
Bergqvist D, Jonsson B. Cost-effectiveness of prolonged administration of a low molecular weight heparin for the prevention of deep venous thrombosis following total hip replacement. Value Health J Int Soc Pharmacoeconomics Outcome Res. 1999;2(4):288–94.
Haentjens P, De Groote K, Annemans L. Prolonged enoxaparin therapy to prevent venous thromboembolism after primary hip or knee replacement. A cost-utility analysis. Arch Orthop Trauma Surg. 2004;124(8):507–17.
Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, Baigent C. Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis. Health Technol Assess. 2005;9(49):iii-iv, ix-x, 1-78.
Turpie AG, Bauer KA, Caprini JA, Comp PC, Gent M, Muntz JE, Apollo I. Fondaparinux combined with intermittent pneumatic compression vs. intermittent pneumatic compression alone for prevention of venous thromboembolism after abdominal surgery: a randomized, double-blind comparison. J thromb haemost. 2007;5(9):1854–61.
Kurtoglu M, Yanar H, Bilsel Y, Guloglu R, Kizilirmak S, Buyukkurt D, Granit V. Venous thromboembolism prophylaxis after head and spinal trauma: intermittent pneumatic compression devices versus low molecular weight heparin. World J Surg. 2004;28(8):807–11.
Ginzburg E, Cohn SM, Lopez J, Jackowski J, Brown M, Hameed SM, Miami Deep Vein Thrombosis Study G. Randomized clinical trial of intermittent pneumatic compression and low molecular weight heparin in trauma. Br J Surg. 2003;90(11):1338–44.
Shackford SR, Moser KM. Deep venous thrombosis and pulmonary embolism in trauma patients. J Intensive Care Med. 1988;3:87–98.
Acknowledgments
I would like to thank my colleague Dr. Hirofumi Haga for his contriubution in finalising this manuscript. I would also like to thank the research staff at Westmead Hospital for their contribution.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Chu, CC., Haga, H. Venous thromboembolism associated with lower limb fractures after trauma: dilemma and management. J Orthop Sci 20, 364–372 (2015). https://doi.org/10.1007/s00776-014-0690-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0690-4