Abstract
Rotator cuff tear is one of the most common shoulder diseases. It is interesting that some rotator cuff tears are symptomatic, whereas others are asymptomatic. Pain is the most common symptom of patients with a tear. Even in patients with an asymptomatic tear, it may become symptomatic with an increase in tear size. Physical examination is extremely important to evaluate the presence, location, and extent of a tear. It also helps us to understand the mechanism of pain. Conservative treatment often works. Patients with well-preserved function of the supraspinatus and infraspinatus are the best candidates for conservative treatment. After a successful conservative treatment, the symptom once disappeared may come back again. This recurrence of symptoms is related to tear expansion. Those with high risk of tear expansion and those with less functional rotator cuff muscles are less likely to respond to conservative treatment. They may need a surgical treatment.
Similar content being viewed by others
Prevalence of rotator cuff tears
Rotator cuff tear is a common disease. According to general population surveys, the prevalence of rotator cuff tear is 25 % in those older than 50 years of age [1] and 20 % in those older than 20 years of age [2]. The interesting thing is that only 1/3 of the tears cause pain and 2/3 are without pain. Only 20 % of those who have shoulder pain come to the clinic, whereas the rest go to bone setters or chiropractors, buy pain killers, or just leave it alone [3]. This means that only 1/15 of those with rotator cuff tears come to see us at the clinic. In other words, when we see one patient at our clinic with a symptomatic rotator cuff tear, there are 4 more patients with a symptomatic tear and 10 more patients with an asymptomatic tear in the background.
Symptoms of rotator cuff tears
We evaluated the symptoms of patients with rotator cuff tears when they first come to see us [4]. There were 157 patients who visited us: 138 patients (87.9 %) came to us because of pain; 17 (10.8 %) came to us because of pain and muscle weakness less than manual muscle testing (MMT) grade 3 (fair); 2 patients (1.3 %) came to us because of muscle weakness less than MMT grade 3 without pain. Almost 99 % of patients with rotator cuff tears come to the clinic because of pain. In other words, controlling pain is the key element of treatment. What causes pain in shoulders with rotator cuff tears? We often experience that an injection of local anesthetics into the subacromial bursa decreases shoulder pain and increases shoulder strength [5]. Koike et al. [6] reported that the uptake of radioisotopes on bone scintigraphy increased in shoulders with a symptomatic tear compared to the contralateral intact shoulders. Inflammation seems to be one of the major causes of pain in shoulders with a rotator cuff tear. In fact, oral medication of anti-inflammatory non-steroidal drugs (NSAIDs) or intra-articular injection of corticosteroid is known to be effective in reducing the pain. Although the conservative treatment does not promote the healing of a tear, it is effective in most of the cases because the major symptom is pain, which is often controllable by the conservative treatment.
Physical examination
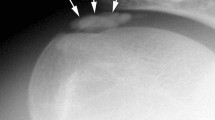
Physical examination starts with inspection. It is easy to detect muscle atrophy of the infraspinatus viewing from the back of the patient because the infraspinatus is located just under the skin, whereas the supraspinatus is covered by the trapezius (Fig. 1). Atrophy of the shoulder muscles is a common finding in patients with rotator cuff tears. The position of the scapula is also important. If the parascapular muscles do not function well, the scapula is protracted and located away from the spinous processes. Next, the scapular motion on the thorax is examined from the back of the patient. The scapula rotates upward and downward during arm elevation/depression. This smooth movement of the scapula on the thorax may have deteriorated because of subacromial impingement, and as a result, the medial boarder of the scapula may be prominent during arm depression in order to avoid the passing of the rotator cuff tendon underneath the acromion (Fig. 2). Palpation of the cuff tendon defect is a very useful examination. Codman [7] described this palpation technique in his textbook “The Shoulder.” The tip of the finger is placed just anterior to the acromion to palpate the defect of the cuff tendon (Fig. 3). A tendon defect may be felt just anterior to the acromion with the shoulder in extension, and it disappears under the acromion with the shoulder in flexion. According to Wolf and Agrawal [8], the sensitivity and specificity of this palpating of the cuff tendon defect for the diagnosis of full-thickness rotator cuff tears were 96 and 97 %, respectively, which were equivalent to the sensitivity and specificity of magnetic resonance imaging (MRI) or ultrasonography.
During active or passive arm elevation, patients may feel shoulder pain because of subacromial impingement. It is called “painful arc” if the pain appears during active arm elevation or depression. The pain appears between 90° and 120° during arm elevation, and it appears between 90° and 30° during arm depression. On the other hand, if the pain appears during passive arm motion, it is called a positive “impingement sign.” Two types of impingement sign are well known: the Neer [9] (Fig. 4) and the Hawkins and Kennedy [10] (Fig. 5). Modifications of these signs are also possible (Figs. 6, 7).
For the purpose of identifying which tendon is ruptured, various location-specific physical examinations have been reported. A tear of the supraspinatus tendon can be detected by the empty-can test (Fig. 8) [11] or full-can test (Fig. 9) [12]. The accuracy of the tests was the greatest when muscle weakness was interpreted as indicating a torn supraspinatus tendon in both the full-can test (75 % accurate) and the empty-can test (70 % accurate) [13].
The major external rotators of the shoulder are the infraspinatus and teres minor. Measuring the isometric strength of external rotation with the arm at the side is commonly performed to detect a tear of the infraspinatus [14]. A patient cannot keep the arm in external rotation at the side when a tear involves the major portion of the infraspinatus tendon. As a result, the forearm drops to the neutral rotation position, and this is called the “dropping sign,” described by Neer [15] (Fig. 10). Hertel et al. [16] introduced an external rotation lag sign, which is similar to the “dropping sign.” If a tear is more extensive and involves the teres minor, the external rotation strength decreases with the arm in abduction, which leads to a positive hornblower’s sign (Fig. 11) [17]. Walch et al. [17] reported that the hornblower’s sign had a sensitivity of 100 % and a specificity of 93 % for the presence of stage 3 or stage 4 fatty degeneration of teres minor on the CT scan. On the other hand, the dropping sign had a 100 % sensitivity and specificity for the presence of stage 3 or stage 4 fatty degeneration of the infraspinatus.
Dropping sign or external rotation lag sign. The patient is asked to keep the arm in external rotation. On the intact side (a), the patient can keep the arm in external rotation position when the examiner lets the arm go. On the involved side (b), the patient cannot keep the arm in external rotation, and the arm comes back to the neutral rotation after the examiner lets the arm go
With a tear of the subscapularis, the internal rotation strength theoretically decreases, but because of the other internal rotators such as the teres major, latissimus dorsi, and pectoralis major, it is difficult to evaluate a decrease in the internal rotation strength with the arm in neutral rotation using the manual muscle test. The lift-off test to detect a subscapularis tear was introduced by Gerber and Krushell [18] (Fig. 12). Placing the hand behind the back at the lumbar level, the shoulder is almost in full internal rotation, and the only internal rotator that functions in this position is the subscapularis. The patient is instructed to raise the hand off the back, performing a further internal rotation of the shoulder. Inability to hold the hand off the back is indicative of subscapularis tearing. In cases with limited motion of internal rotation, the belly press test is recommended (Fig. 13) [19].
Belly-press test. With the intact subscapularis, a patient can press the belly with the hand, wrist, and elbow straight (a). If the subscapularis is torn, the patient cannot keep the hand, wrist, and elbow straight to press the belly (b). Due to weakness, the patient flexes the wrist and brings the elbow backward in order to press the belly
Conservative treatment
For the purpose of eliminating pain, we use oral NSAID medication, steroids or hyaluronic acid injections into the glenohumeral joint or subacromial bursa depending upon the site of the tear. Physical therapy such as heat, stretching, passive and active range of motion exercises, and muscle strengthening exercises are prescribed. Evaluation of any abnormal movement of the scapulothoracic motion is also important. If there is any dyskinesis of the scapulothoracic motion (scapular protraction), it needs to be corrected by physical therapy.
How effective is conservative treatment? The success rate of conservative treatment ranges from 33 % [20] to 82 % [21] in the literature. In our first study [21], we retrospectively reviewed 62 shoulders of 54 patients with full-thickness tears who were followed up without surgery. The follow-up period averaged 3.4 years. According to modified criteria of Wolfgang, 51 shoulders in 45 patients (82 %) were rated as satisfactory (excellent or good). The patients with satisfactory results and unsatisfactory results among those observed more than 5 years were compared. The only significant differences in the initial findings between the two groups were the active abduction angle and the abduction strength: the patients with satisfactory results retained a good range of motion and strength, whereas those with unsatisfactory results had a limited range and muscle weakness on initial examination. Conservative treatment affords satisfactory results when given to the patients with well-preserved motion and strength. The limitation of this study was that all surgical cases were excluded. In order to evaluate the efficacy of conservative treatment, those who failed to respond to conservative treatment and eventually underwent surgical treatment should be included as failure cases of conservative treatment. In our next study [22], we prospectively treated 107 shoulders of 105 consecutive patients with full-thickness tears of the rotator cuff. We performed conservative treatment for 6 months. If the shoulder symptoms disappeared or became mild enough, the treatment was discontinued. If the shoulder symptoms remained but the patients did not want to undergo surgery, conservative treatment was continued. If the patients were not happy with their shoulder because of remaining symptoms after 6 months of conservative treatment, they underwent surgical treatment with informed consent. The average age of the patients was 64 years (range 44–80 years). Three patients underwent surgical treatment. These three patients were evaluated as failure cases of conservative treatment. At the time of follow-up, one patient was dead as the result of a cause other than the shoulder and one patient was missing. In total, we followed 102 shoulders of 100 patients with an average follow-up period of 32 (12–48) months. At the time of follow-up, 50 % of them were totally pain free, and 40 % had mild pain not requiring pain killers. Regarding activities of daily living, 75 % of the patients said they felt no limitations in daily activities. In total, 75/100 (75 %) had good or excellent results according to the Shoulder Rating Score of the Japanese Orthopaedic Association. Adding three surgical cases as failure cases, the success rate was 73 % (75/103).
Kuhn et al. [23] reported a multicenter prospective cohort study. As of May 2010, 396 patients with full thickness rotator cuff tears have been enrolled. They began a physical therapy program with or without an intraarticular injection depending upon the severity of symptoms. They returned for evaluation at 6 and 12 weeks. At those visits, they could choose one of three outcomes: (1) cured (no follow-up scheduled), (2) improved (continued therapy with scheduled reassessment in 6 weeks), or (3) not better (arthroscopic cuff repair scheduled). Patients were contacted by telephone at 1 and 2 years. Overall, 10 % of the patients chose surgery after 6 weeks and another 10 % chose surgery within 2 years. This made the success rate of conservative treatment 90 % at 6 weeks and 80 % at 2 years.
Considering these studies, conservative treatment is thought to be effective in 73–80 % of cases with full-thickness tears of the rotator cuff. A systematic review has shown that exercise has statistically and clinically significant effects on pain reduction and improving function, but not on the range of motion or strength [24].
When we perform conservative treatment, we should pay attention to two things: (1) the responsiveness of patients to conservative treatment and (2) recurrence of symptoms. We know that conservative treatment is effective in 73–80 % of patients. If we know who will respond well to conservative treatment and who will not before initiating the treatment, it would be beneficial for both the doctors and patients because we would not have to waste non-responders' time. Also, the present symptom might go away after conservative treatment, but could recur in the future. If the symptoms disappear after the initial treatment but come back repeatedly, the patient will not be happy. If we knew who had a good chance of recurrence, we could advise surgery for them.
Responders and non-responders
We performed a study to determine the physical and MRI findings characteristic of responders on the initial examination by comparing those who responded well and those who responded poorly to conservative treatment [25]. This study included 123 shoulders of 118 patients with full-thickness rotator cuff tears diagnosed by MRI. All patients were treated conservatively for at least 3 months. Clinical symptoms improved in 65 shoulders of 62 patients with conservative treatment (responders), but remained unchanged or aggravated in 58 shoulders of 56 patients who eventually underwent surgical repair (non-responders). The following parameters showed significant differences: (1) impingement sign (positive in 30.7 % in the responders and 79.3 % in the non-responders); (2) active external rotation angle on physical examination (52.2° in the responders and 35.0° in the non-responders); (3) integrity of the intramuscular tendon of the supraspinatus on MRI (58.4 % in the responders and 24.1 % in the non-responders showed an intact intramuscular tendon); (4) presence of supraspinatus muscle atrophy on MRI (occupancy ratio was 78.0 % in the responders and 69.8 % in the non-responders). The success rate of conservative treatment was 92 % in patients with all of these four factors and 5.2 % in those with none of these factors. These four factors seem to be useful in separating responders from non-responders before initiating treatment.
Recurrence of symptoms
Symptoms may come back again after the shoulder has become symptom free. Some asymptomatic tears become symptomatic. Yamaguchi et al. [26] followed up 58 patients with asymptomatic tears using ultrasonography. After an average of 2.8 years, 51 % of them became symptomatic. They found that there was a strong association between symptom appearances and tear size expansion. Mall et al. [27] prospectively monitored 195 patients with asymptomatic tears for pain development. With pain development, the size of a full-thickness tear increased significantly, with 18 % of the full-thickness tears showing an increase of more than 5 mm, and 40 % of the partial-thickness tears progressed to a full-thickness tear. They concluded that pain development in shoulders with an asymptomatic tear was associated with an increase in tear size. Safran et al. [28] evaluated 61 full-thickness tears equal to or larger than 5 mm in 51 patients using ultrasonography. At an average follow-up period of 29 months, 49 % of the tears increased in size. There was a significant correlation between the existence of pain and increase in tear size. These reports tell us that the remnant or recurrent pain is related to an increase in tear size.
What are the risk factors for tear propagation? According to Safran et al. [28], there were no correlations between the change in tear size and age of the patients, sex, existence of a prior trauma, initial size of the tear, and bilateral tears. On the other hand, Maman et al. [29] reported that factors that were associated with progression of a rotator cuff tear were an age of more than 60 years, a full-thickness tear, and fatty infiltration of the rotator cuff muscles. We evaluated the relationship between the tear size and the degree of labor in 195 patients with rotator cuff tears (unpublished data). The tear size was significantly greater in heavy laborers (8.2 ± 1.7 cm2) than in medium (4.9 ± 1.1 cm2) or sedentary laborers (4.2 ± 1.5 cm2) (p = 0.0020). Vigorous use of the shoulder or traumatic event on the shoulder seems to be related to tear expansion. Smoking is known to be related to tear size: the greater the smoking index, the larger the tear [30, 31]. These factors need to be taken into consideration when performing conservative treatment. Further studies to clarify the risk factors of tear expansion need to be undertaken.
References
Minagawa H, Itoi E, Abe H, Fukuta M, Yamamoto N, Seki N, Kikuchi K. Epidemiology of rotator cuff tears. J Jpn Orthop Assoc. 2006;80:S217 (in Japanese).
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. J Should Elbow Surg. 2010;19:116–20.
Kobayashi M, Itoi E, Minagawa H, Yamamoto N, Tuoheti Y, Saito H, Seki N, Aizawa T, Abe H. Prevalence of the shoulder pain in the middle-aged and the elderly and their choices for the treatment. Katakansetsu 2004;29:179 (in Japanese).
Itoi E, Minagawa H, Yamamoto N, Seki N, Abe H. Are pain location and physical examinations useful in locating a tear site of the rotator cuff? Am J Sports Med. 2006;34:256–64.
Itoi E, Minagawa H, Sato T, Sato K, Tabata S. Isokinetic strength after tears of the supraspinatus tendon. J Bone Joint Surg Br. 1997;79:77–82.
Koike Y, Sano H, Kinjyo T, Imamura I, Masahiro O, Goto M, Ooyama M, Kita A, Itoi E. Shoulder surface temperature and bone scintigraphy findings in patients with rotator cuff tears. Ups J Med Sci. 2011;116:142–7.
Codman EA. Chapter V: Rupture of the supraspinatus tendon. In: The shoulder: rupture of the supraspinatus tendon and other lesions in and around the subacromial bursa. Boston: Thomas Todd Company; 1934. p. 123–77.
Wolf EM, Agrawal V. Transdeltoid palpation (the rent test) in the diagnosis of rotator cuff tears. J Should Elbow Surg. 2001;10:470–3.
Neer CS II. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54:41–50.
Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151–8.
Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med. 1982;10:336–9.
Kelly BT, Kadrmas WR, Speer KP. The manual muscle examination for rotator cuff strength: an electromyographic investigation. Am J Sports Med. 1996;24:581–8.
Itoi E, Kido T, Sano A, Urayama M, Sato K. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med. 1999;27:65–8.
Matsen FA III, Fehringer EV, Lippitt SB, Wirth MA, Rockwood CA Jr. Rotator cuff. In: Rockwood Jr CA, Matsen III FA, Wirth MA, Lippitt SB, editors. The shoulder. 4th ed. Philadelphia: Saunders/Elsevier; 2009. p. 771–889.
Neer CS. Anatomy of shoulder reconstruction. In: Neer CS, ed. Shoulder reconstruction. Philadelphia: W. B. Saunders Company; 1990. p. 1–39.
Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Should Elbow Surg. 1996;5:307–13.
Walch G, Boulahia A, Calderone S, Robinson AH. The ‘dropping’ and ‘hornblower’s’ signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80(4):624–8.
Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73:389–94.
Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78:1015–23.
Wolfgang GL. Surgical repair of tears of the rotator cuff of the shoulder. Factors influencing the result. J Bone Joint Surg Am. 1974;56:14–26.
Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop. 1992;275:165–73.
Minagawa H, Itoi E, Saito I. Conservative treatment of rotator cuff tears. Rheumatology 2001;25:494–500 (in Japanese).
Kuhn JE, Dunn WR, An AQ, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway GB, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Spencer Jr EE, Vidal AF, Wolf BR, Wright RW. Effectiveness of physical therapy in treating atraumatic full thickness rotator cuff tears. A multi-center prospective cohort study. In: 2011 Open meeting, American Shoulder and Elbow Surgeons, San Diego, 19 Feb 2011.
Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Should Elbow Surg. 2009;18:138–60.
Tanaka M, Itoi E, Sato K, Hamada J, Hitachi S, Tojo Y, Honda M, Tabata S. Factors related to successful outcome of conservative treatment for rotator cuff tears. Ups J Med Sci. 2010;115:193–200.
Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Should Elbow Surg. 2001;10:199–203.
Mall NA, Kim HM, Keener JD, Steger-May K, Teefey SA, Middleton WD, Stobbs G, Yamaguchi K. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92:2623–33.
Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710–4.
Maman E, Harris C, White L, Tomlinson G, Shashank M, Boynton E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91:1898–906.
Itoi E, Minagawa H, Konno N, Kobayashi T, Sato T, Sato K, Nishi T. Smoking habits in patients with rotator cuff tears. Katakansetsu 1996;20:209–12 (in Japanese).
Baumgarten KM, Gerlach D, Galatz LM, Teefey SA, Middleton WD, Ditsios K, Yamaguchi K. Cigarette smoking increases the risk for rotator cuff tears. Clin Orthop Relat Res. 2010;468:1534–41.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Itoi, E. Rotator cuff tear: physical examination and conservative treatment. J Orthop Sci 18, 197–204 (2013). https://doi.org/10.1007/s00776-012-0345-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-012-0345-2