Abstract
Background
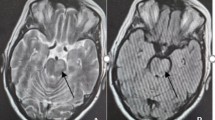
Simultaneous appearance of sphenoid sinus aspergilloma and pituitary adenoma is a very rare finding.
Methods
Retrospective analysis of patients with sellar and sphenoid sinus mass lesions who underwent trans-sphenoidal surgery was performed. Demographic data, medical history, predisposing factors, clinical picture, neurological status and radiological findings were reviewed. All patients underwent a trans-sphenoidal microsurgical treatment, and acquired specimens underwent both histopathological and microbiological analysis.
Results
Sphenoid sinus aspergilloma was encountered in seven patients. Three patients had an isolated sphenoid sinus aspergilloma and four patients with pituitary macroadenoma had a sphenoid aspergilloma as an incidental finding.
Conclusions
Sphenoid sinus aspergilloma can be found during trans-sphenoidal surgery for pituitary adenomas. Sphenoid sinus extirpation followed by adenomectomy is the treatment of choice unless invasive aspergilloma is encountered requiring additional antifungal therapy.



Similar content being viewed by others
References
Ahmeti H, Balschun K, Mehdorn H, Stark A (2014) Unusual coincidence of a pituitary adenoma and an aspergilloma of the sphenoid sinus. J Neurooncol 119(2):447–448
Azarpira N, Esfandiari M, Bagheri MH, Rakei S, Salari S (2008) Cerebral aspergillosis presenting as a mass lesion. Braz J Infect Dis 12:349–351
Azarpira N, Anbardar M, Taghipour M (2014) Coexistance of pituitary adenoma with sphenoid sinus fungus ball. Neurosurg Q 24:50–52
Blitzer A, Lawson W (1993) Fungal infections of the nose and paranasal sinuses: part I. Otolaryngol Clin North Am 26:1007–1103
Boutarbouch M, Arkha Y, El Ouahabi A, Derraz S, El Khamlichi A (2009) Sphenoid sinus aspergillosis simulating pituitary tumor in immunocompetent patient. J Clin Neurosci 16:840–841
Bowman J, Panizza N, Gandhi M (2007) Sphenoid sinus fungal balls. Ann Otol Rhinol Laryngol 116:514–519
Brandwein M (1993) Histopathology of sinonasal fungal disease. Otolaryngol Clin North Am 26:949–981
Bridenstine M, Kerr JM, Lillehei KO, Kleinschmidt-Demasters BK (2013) Cushing’s disease due to mixed pituitary adenomagangliocytoma of the posterior pituitary gland presenting with Aspergillus sp. sinus infection. Clin Neuropathol 32:377–383
Castelnuovo P, Pagella F, Semino L (2005) Endoscopic treatment of the isolated sphenoid sinus lesion. Eur Arch Otorhinolaryngol 262:142–147
Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A (2005) Intracranial fungal granuloma: analysis of 40 patients and review of the literature. Surg Neurol 63:254–260
Ferguson BJ (2000) Definitions of fungal rhinosinusitis. Otolaryngol Clin North Am 33:227–235
Friedman A, Batra PS, Fakhri S, Ctardi MJ, Lanza DC (2005) Isolated sphenoid sinus disease: etiology and management. Otolaryngol Head Neck Surg 133:544–550
Furtado SV, Venkatesh PK, Ghosal N, Hegde AS (2011) Invasive sphenocavernous aspergilloma complicating an operated case of acromegaly. Skull Base Rep 1(1):33–38
Garcia-Reija MF, Crespo-Pinilla JL, Labayru-Echeverria C (2002) Invasive maxillary aspergilossis: report of a case and review of the literature. Med Oral 7:200–205
Gilain L, Aidan D, Coste A, Peynegre R (1994) Functional endoscopic sinus surgery for isolated sphenoid sinus disease. Head Neck 16:433–437
Gondim J, Quidute AR, Maciel M, Carneiro A, Tavares C, Fontenele E, Montenegro R (2003) Cushing’s disease and sphenoidal aspergilloma. Acta Radiol 44:685–687
Hao L, Jing C, Bowen C, Min H, Chao Y (2008) Aspergillus sellar abscess: case report and review of the literature. Neurol India 56:186–188
Iplikcioglu AC, Bek S, Bikmaz K, Ceylan D, Gokduman CA (2004) Aspergillus pituitary abscess. Acta Neurochir (Wien) 146:521–524
Jung JH, Cho GS, Chung YS, Lee BJ (2013) Clinical characteristics and outcome in patients with isolated sphenoid sinus aspergilloma. Auris Nasus Larynx 40:189–193
Karci B, Burhanoglu D, Erdem T (2001) Fungal infections of the paranasal sinuses. Rev Laryngol Otol Rhinol 122:315
Klossek JM, Peloquin L, Fourcroy PJ, Ferrie JC, Fontanel JP (1996) Aspergillomas of the sphenoid sinus: a series of ten cases treated by endoscopic sinus surgery. Rhinology 34:179–183
Lee LA, Huang CC, Lee TJ (2004) Prolonged visual distrubance secondary to isolated sphenoid sinus disease. Laryngoscope 114:986–990
Lee TJ, Huang SF, Chang PH (2009) Characteristics of isolated sphenoid sinsu aspergilloma: report of twelve cases and literature review. Ann Otol Rhinol Laryngol 118:211–217
Martin TJ, Smith TL, Smith MM, Loerhl TA (2002) Evaluation and surgical management of isolated sphenoid sinus disease. Arch Otorynol Head Neck Surg 133:1413–1419
Pagella F, Matti E, De Bernardi F (2007) Paranasal sinus fungus ball: diagnosis and management. Mycoses 50:451–456
Parker KM, Nigholson JK, Cezayrli RC, Biggs PJ (1996) Aspergillosis of the sphenoid sinus: presentation as a pituitary mass and post-operative gallium-67 imaging. Surg Neurol 45:354–358
Petrick M, Honegger J, Daschner F, Feuerhake F, Zentner J (2003) Fungal graniloma of the sphenoid sinus and clivus in a patient presenting with cranial nerve III paresis: case report and review of the literature. Neurosurgery 52(4):955–959
Ramos-Gabatin A, Jordan RM (1981) Primary pituitary aspergillosis responding to transsphenoidal surgery and combined therapy with amphotericin-B and 5-fluorocytosine: case report. J Neurosurg 54:839–841
Sethi DS (1999) Isolated sphenoid lesions: diagnosis and management. Otolaryngol Head Neck Surg 120:730–736
Sharma BS, Khosla VK, Kak VK, Banarjee AK, Vasishtha RK, Prasad KS, Sharma SC, Mathuriya SN, Tewari MK, Pathak A (1997) Intracranial fungal granuloma. Surg Neurol 47(5):489–497
Shaw CL, McCleave M, Wormald PJ (2000) Unusual presentations of isolated sphenoid fungal sinusitis. J Laryngol Otol 114:385–388
Thery A, Espitalier F, Cassagnau E, Durand E, Malard O (2012) Clinical features and outcome of sphenoid sinus aspergillosis: a retrospective series of 15 cases. Eur Ann Otorhinolaryngol Head Neck Dis 129:179–184
Yamada K, Zoarski GH, Rothmann MI (2001) An intracranial aspergilloma with low signal on T2-weighted images corresponding to iron accumulation. Neuroradiology 43:459–461
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
This paper by Sajko et al. touches an important issue in pituitary surgery: not every space-occupying lesion (SOL) that appears to be a pituitary adenoma (PA) preoperatively turns out to be a PA postoperatively. The rate of unexpected histology in presumably endocrine inactive PA may be as high as 18 % [1]. Typically, endocrine inactive PA are tumours of an advanced age [2]. Interestingly, the patients with a suspected endocrine inactive PA who finally turned out to have an unexpected histology also seem to belong to the advanced age group [1]. Sajko et al. found aspergilloma in trans-sphenoidal surgery for presumed PA in basically 1.3 % of their total of about 1,000 cases. If one assumes a normal distribution of PA coming to trans-sphenoidal surgery at their institution, about 27 % would be endocrine inactive [2]. Since cases of intrasellar or parasellar aspergilloma are unlikely to present as endocrine active PA, it is probably safe to assume that the majority of the 13 patients with aspergilloma presented preoperatively as endocrine inactive PA. With this in mind, one may expect a 3–4 % rate of aspergilloma in all presumed endocrine inactive PA at the authors’ institution. This rate may even be higher in less developed regions. Just as the patients with endocrine inactive PA, the patients with intrasellar or parasellar aspergilloma were of an advanced age group. The authors found a preponderance for females, which was not the case for neoplastic unexpected histologies [1]. Diabetes mellitus or immunodeficiency was present in almost half of their patients with aspergilloma. Just as the authors conclude, awareness should be heightened especially in elderly female patients presenting with a SOL in the sphenoid sinus and the sellar region. The authors are not the first to report on aspergilloma in the sellar region [3], but they certainly are the first to present a systematic review of this non-neoplastic SOL mimicking PA in their own large neurosurgical patient cohort. It is of great importance to pituitary surgeons to be aware that not every SOL which preoperatively seems to be a PA is necessarily a PA and that it may not even be a neoplastic lesion. This awareness adds to the patients’ security, since some of those unexpected lesions may require alternative surgical strategies from the conventional PA surgery. This manuscript underscores the need to approach “pituitary” patients with an open mind.
Thomas Mindermann
Zurich, Switzerland
1. Mindermann T, Staub JJ, Probst A (1998) High rate of unexpected histology in presumed pituitary adenomas. Lancet 352(9138):1445
2. Mindermann T, Wilson CB (1994) Age-related and gender-related occurrence of pituitary adenomas. Clin Endocrinol 41:359–364
3. Petrick M, Honegger J, Daschner F, Feuerhake F, Zentner J (2003) Fungal granuloma of the sphenoid sinus and clivus in a patient presenting with cranial nerve III paresis: case report and review of the literature. Neurosurgery 52:958–959
Rights and permissions
About this article
Cite this article
Sajko, T., Gnjidić, Ž., Sesar, N. et al. Sphenoid sinus aspergilloma in trans-sphenoidal surgery for pituitary adenomas. Acta Neurochir 157, 1345–1351 (2015). https://doi.org/10.1007/s00701-015-2485-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2485-6