Abstract
Background
Upper cervical nerve sheath tumors (NST) arising mainly from C2 root and to lesser extent from C1 root are not uncommon, they constitute approximately 5-12% of spinal nerve sheath tumors and 18-30% of all cervical nerve sheath tumors, unique in presentation and their relationship to neighbouring structures owing to the discrete anatomy at the upper cervical-craniovertebral region, and have atendency for growth reaching large-sized tumors before manifesting clinically due to the capacious spinal canal at this region; accordingly the surgical approaches to such tumors are modified. The aim of this paper is to discuss the surgical strategies for upper cervical nerve sheath tumors.
Methods
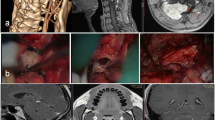
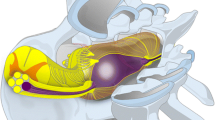
Eleven patients (8 male and 3 females), age range 28–63 years, with C2 root nerve sheath tumors were operated upon based on their anatomical relations to the spinal cord. The magnetic resonance imaging findings were utilized to determine the surgical approach. The tumors had extra- and intradural components in 10 patients, while in one the tumor was purely intradural. The operative approaches included varied from extreme lateral transcondylar approach(n = 1) to laminectomy, whether complete(n = 3) a or hemilaminectomy(n = 7), with partial facetectomy(n = 7), and with suboccipital craniectomy(n = 2).
Results
The clinical picture ranged from spasticity (n = 8, 72,72 %), tingling and numbness below neck (n = 6, 54,54 %), weakness (n = 6, 54,54 %), posterior column involvement (n = 4, 26,36 %), and neck pain (n = 4, 36,36 %). The duration of symptoms ranged from 1 to 54 months, total excision was performed in 7 patients; while in 3 patients an extraspinal component, and in 1 patient a small intradural component, were left in situ. Eight patients showed improvement of myelopathy; 2 patients maintained their grades. One poor-grade patient was deteriorated.
Conclusion
The surgical approaches for the C2 root nerve sheath tumors should be tailored according to the relationship to the spinal cord, determined by magnetic resonance imaging.

Similar content being viewed by others
References
McCormick PC, Post KD, Stein BM (1990) Intradural extramedullary tumors in adults. Neurosurg Clin N Am 1(3):591–608
Bucci MN, McGillicuddy JE, Taren JA, Hoff JT (1990) Management of anteriorly located C1–C2 neurofibromata. Surg Neurol 33:15–18
George B, Lot G (1995) Neurinomas of the first two cervical nerve roots: a series of 42 cases. J Neurosurg 82:917–923
Welling B, Park YK, Al-Mefty O (1988) Primary extramedullary tumors of the craniovertebral junction. In: Dickman CA, Spetzler RF, Sonntag VK (eds) Surgery of the craniovertebral junction, 1st edn. Theime, New York, pp 240–242
McCormick PC, Stein BM (1994) Spinal cord tumors in adults. In: Youmans JR (ed) Neurological Surgery, Vol. 4, 4th edn. WB Saunders Company, Philadelphia, pp. 302–323
Bartolomei JC, Crockard A (2001) Bilateral posterolateral approach to mirror-image C-2 neurofibromas. Report of four cases. J Neurosurg 94:292–298
Klekamp J, Samii M (1998) Surgery of spinal nerve sheath tumors with special reference to neurofibromatosis. Neurosurgery 42:279–290
Smith DA, Schmeidek HH (1980) Tumors of the nerve sheath involving the spine. In: Sundaresan N, Schmeidek HH, Schiller A, Rosenthal DM (eds) Tumors of the spine: diagnosis and clinical management, 1st edn. WB Saunders Company, Philadelphia, pp. 226–227
Yasuoka S, Okazaki H, Daube JR, MacCarty CS (1978) Foramen magnum tumors. Analysis of 57 cases of benign extramedullary tumors. J Neurosurg 49:828–838
Zdeblick TA, Zou D, Warden KE (1992) Cervical stability after foraminotomy. A biomechanical in vitro analysis. J Bone Joint Surg (Am) 74:22–27
Banerji D, Behari S, Jain VK, Pandey T, Chhabra DK (1999) Extreme lateral transcondylar approach to the skull base. Neurol India 47:22–31
Pritz MB (1991) Evaluation and treatment of intradural tumors located anterior to the cervicomedullary junction by a lateral suboccipital approach. Acta Neurochir (Wein) 113:74–81
Sen CN, Sekhar LN (1990) An extreme lateral approach to intradural lesions of the cervical spine and foramen magnum. Neurosurgery 27:197–204
Behari S, Banerji D, Trivedi P, Jain VK, Chhabra DK (2002) Anterior retropharyngeal approach to the upper cervical spine. Neurol India 49:342–349
Nittner K (1976) Spinal meningioma, neurinomas and neurofibromas and hourglass tumors. In: Vinken PJ, Bruyn GW (eds) Handbook of clinical neurology, Vol. 20. North Holland/America Elsevier, New York, pp. 177–322
Levy WJ, Latchaw J, Hahn JF, Sawhny B, Bay J, Dohn DF (1986) Spinal neurofibromas: a report of 66 cases and a comparison with meningiomas. Neurosurg 18(3):331–334
Guidetti B, Spallone A (1988) Benign extramedullary tumors of the foramen magnum. In: Symon L (ed) Advances and technical standards in neurosurgery, Vol. 16. Springer, Wein, pp. 84–120
Lot G, George B (1997) Cervical neuromas with extradural components: surgical management in a series of 57 patients. Neurosurgery 41:813–822
Freeman TB, Cahill DW (1996) Tumors of the meninges, cauda equine, and spinal nerves. In: Menezes AH, Sonntag VKH (eds) Principles of spinal surgery, Vol. 2. McGraw-Hill, New York, pp. 1371–1386
Jinnai T, Hoshimaru M, Koyama T, Yasargil MG, Hedley-Whyte ET, Brotchi J (2005) Clinical characteristics of spinal nerve sheath tumors: analysis of 149 cases. Neurosurg 56(3):510–515
Soulié A (1901) Nerfs rachidiens. In: Poirier P, Charpy A (eds) Traite d’anatomie humaine. Masson & Cie, Paris
Goel A, Muzumdar D, Nadkarni T, Desai K, Dange K, Chagla A (2008) Retrospective analysis of peripheral nerve sheath tumors of the second cervical nerve root in 60 surgically treated patients. J Neurosurg Spine 8(2):129–134
Jee WH, Oh SN, McCauley T, Ryu KN, Suh JS, Lee JH, Park JM, Chun KA, Sung MS, Kim K, Lee YS, Kang YK, Ok IY, Kim JM (2004) Extraaxial neurofibroma, versus neurilemmomas: discimination with MRI. AJR 183:629–633
Tubbs RS, Salter G, Grabb PA, Oakes WJ (2001) The denticulate ligament: anatomy and functional significance. J Neurosurg 94:271–275
Cusick JF, Yoganandan N, Pintar F (1988) Biomechanics of cervical spine facetectomy and fixation techniques. Spine 13:808–812
McCormick PC (1996) Surgical management of dumb-bell tumors of the cervical spine. Neurosurgery 38:294–300
Verbiest JH (1986) A lateral approach to the cervical spine-technique and indications. J Neurosurg 28:191–203
Crockard HA, Transoral BR (1985) transclival removal of a schwannoma anterior to the craniocervical junction. J Neurosurg 62:293–295
Crockard HA, Sen CN (1991) Transoral approach for the management of intradural lesions at the cervicovertebral junction – a review of 7 cases. Neurosurgery 28:88–98
Jain VK, Behari S, Banerji D, Bhargava V, Chhabra DK (1999) Transoral decompression for craniovertebral anomalies: perioperative management dilemmas. Neurol India 47:188–195
Celli P (2002) Treatment of relevant nerve roots involved in nerve sheath tumors: removal or preservation? Neurosurgery 51:684–692
Schultheiss R, Gullotta G (1993) Resection of relevant nerve roots in surgery of spinal neurinomas without persisting neurological deficit. Acta Neurochir (Wien) 122:91–96
Kim P, Ebersold MJ, Onofrio BM, Quast LM (1989) Surgery of spinal nerve schwannoma: risk of neurological deficit after resection of involved root. J Neurosurg 71:810–814
Seppala MT, Haltia MJJ, Sankila RJ, Jaaskelainen JE, Heiskanen O (1995) Long term outcome after removal of spinal neurofibroma. J Neurosurg 82:572–577
Seppala MT, Haltia MJJ, Sankila RJ, Jaaskelainen JE, Heiskanen O (1995) Long term outcome after removal of spinal schwannomas. A clinicopathological study of 187 cases. J Neurosurg 83:621–626
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Abbreviations used in this paper: NST=nerve sheath tumors; C1=atlas vertebra; C2=axis vertebra; MRI=magnetic resonance imaging; CVJ=craniovertebral junction; CSF=cerebrospinal fluid; NF-1= neurofibromatosis type 1; roots of C5, D1, D6, L1, S1, and S5=roots of 5th cervical, 1st dorsal, 6th dorsal, first lumbar, first sacral and 5th sacral spinal segment.
Rights and permissions
About this article
Cite this article
El-Sissy, M.H., Mahmoud, M. C2 root nerve sheath tumors management. Acta Neurochir 155, 779–784 (2013). https://doi.org/10.1007/s00701-013-1659-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1659-3