Abstract
Purpose
We reviewed the literature regarding the specific methods and strategies for implementing simulation-based training into the modern surgical residency curriculum. Residency programs are still struggling with how best to implement it into their curricula from a practical viewpoint.
Methods
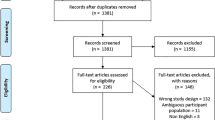
A systematic review was performed using Ovid MEDLINE, EMBASE, PubMed, PsycINFO, Web of Science, and other resources for studies involving the use of simulation for technical skills training in the surgical residency curriculum. Studies were selected based on the integration of simulation into the curriculum and/or a description of the details of implementation and the resources required.
Results
In total, 2533 unique citations were retrieved based on this search, and 31 articles met the inclusion criteria. Most simulators were focused on laparoscopic procedures, and training occurred most often in a skills lab. The assessment of skills consisted mostly of speed of task completion. Only 4 studies addressed issues of cost, and 6 programs mentioned human resources without any mention of skills center personnel or administrative support.
Conclusions
All of the studies described the nature of the simulation training, but very few commented on how it was actually implemented and what was needed from organizational, administrative and logistical perspectives.

Similar content being viewed by others
References
Sturm LP, Windsor JA, Cosman PH, Cregan P, Hewett PJ, Maddern GJ. A systematic review of skills transfer after surgical simulation training. Ann Surg. 2008;248:166–79.
Seymour NE. VR to OR: a review of the evidence that virtual reality simulation improves operating room performance. World J Surg. 2008;32:182–8.
Gurusamy K, Aggarwal K, Palanivelu L, Davidson B. Systematic review of randomized controlled trials on the effectiveness of virtual reality training for laparoscopic surgery. Br J Surg. 2008;95:1088–97.
ACGME Program Requirements for Graduate Medical Education in General Surgery. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/440_general_surgery_07012015.pdf. Accessed 21 August 2016.
Hamilton EC, Scott DJ, Kapoor A, Nwariaku F, Bergen PC, Rege RV, et al. Improving operative performance using a laparoscopic hernia simulator. Am J Surg. 2001;182:725–8.
Powers TW, Murayama KM, Toyama M, Murphy S, Denham Iii EW, Derossis AM, et al. Housestaff performance is improved by participation in a laparoscopic skills curriculum. Am J Surg. 2002;184:626–30.
Neumann M, Hahn C, Horbach T, Schneider I, Meining A, Heldwein W, et al. Score card endoscopy: a multicenter study to evaluate learning curves in 1-week courses using the Erlangen Endo-Trainer. Endoscopy. 2003;35:515–20.
Dayal R, Faries PL, Lin SC, Bernheim J, Hollenbeck S, DeRubertis B, et al. Computer simulation as a component of catheter-based training. J Vasc Surg. 2004;40:1112–7.
Clark JA, Volchok JA, Hazey JW, Sadighi PJ, Fanelli RD. Initial experience using an endoscopic simulator to train surgical residents in flexible endoscopy in a community medical center residency program. Curr Surg. 2005;62:59–63.
Schijven MP, Jakimowicz JJ, Broeders IAMJ, Tseng LNL. The Eindhoven laparoscopic cholecystectomy training course—Improving operating room performance using virtual reality training: results from the first E.A.E.S. accredited virtual reality trainings curriculum. Surg Endosc. 2005;19:1220–6.
Seymour NE. Integrating simulation into a busy residency program. Min Inv Ther All Tech. 2005;14:280–6.
Griffin S, Kumar A, Burgess N, Donaldson P. Development of laparoscopic suturing skills: a prospective trial. J Endourol. 2006;20:144–8.
Levine RL, Kives S, Cathey G, Blinchevsky A, Acland R, Thompson C, et al. The use of lightly embalmed (fresh tissue) cadavers for resident laparoscopic training. J Min Invas Gynec. 2006;13:451–6.
Chang L, Petros J, Hess DT, Rotondi C, Babineau TJ. Integrating simulation into a surgical residency program: is voluntary participation effective? Surg Endosc. 2007;21:418–21.
Passman MA, Fleser PS, Dattilo JB, Guzman RJ, Naslund TC. Should simulator-based endovascular training be integrated into general surgery residency programs? Am J Surg. 2007;194:212–9.
Fann JI, Caffarelli AD, Georgette G, Howard SK, Gaba DM, Youngblood P, et al. Improvement in coronary anastomosis with cardiac surgery simulation. J Thorac Cardiovasc Surg. 2008;136:1486–91.
Goova MT, Hollett LA, Tesfay ST, Gala RB, Puzziferri N, Kehdy FJ, et al. Implementation, construct validity, and benefit of a proficiency-based knot-tying and suturing curriculum. J Surg Educ. 2008;65:309–15.
Jensen AR, Milner R, Achildi O, Gaughan J, Wilhite DB, Grewal H. Effective instruction of vascular anastomosis in the surgical skills laboratory. Am J Surg. 2008;195:189–94.
Jensen AR, Wright AS, McIntyre LK, Levy AE, Foy HM, Anastakis DJ, et al. Laboratory-based instruction for skin closure and bowel anastomosis for surgical residents. Arch Surg. 2008;143:852–8.
Kirby TO, Numnum TM, Kilgore LC, Straughn JM. A prospective evaluation of a simulator-based laparoscopic training program for gynecology residents. J Am Coll Surg. 2008;206:343–8.
Sickle KRV, Ritter EM, Baghai M, Goldenberg AE, Huang I-P, Gallagher AG, et al. Prospective, randomized, double-blind trial of curriculum-based training for intracorporeal suturing and knot tying. J Am Coll Surg. 2008;207:560–8.
Burkhart HM, Riley JB, Hendrickson SE, Glenn GF, Lynch JJ, Arnold JJ, et al. The successful application of simulation-based training in thoracic surgery residency. J Thorac Cardiovasc Surg. 2010;139:707–12.
Edelman DA, Mattos MA, Bouwman DL. FLS skill retention (Learning) in first year surgery residents. J Surg Res. 2010;163:24–8.
Fann JI, Calhoon JH, Carpenter AJ, Merrill WH, Brown JW, Poston RS, et al. Simulation in coronary artery anastomosis early in cardiothoracic surgical residency training: the Boot Camp experience. J Thorac Cardiovasc Surg. 2010;139:1275–81.
Nguyen PH, Acker CE, Heniford BT, Stefanidis D. What is the cost associated with the implementation of the FLS program into a general surgery residency? Surg Endosc. 2010;24:3216–20.
Olson TP, Becker YT, McDonald R, Gould J. A simulation-based curriculum can be used to teach open intestinal anastomosis. J Surg Res. 2010;172:53–8.
Rodriguez-Sanjuan JC, Manuel-Palazuelos C, Fernandez-Diez MJ, Gutierrez-Cabezas JM, Alonso-Martin J, Redondo-Figuero C, et al. Assessment of resident training in laparoscopic surgery based on a digestive system anastomosis model in the laboratory. Cirug Espan. 2010;87:20–5.
Joyce DL, Dhillon TS, Caffarelli AD, Joyce DD, Tsirigotis DN, Burdon TA, et al. Simulation and skills training in mitral valve surgery. J Thorac Cardiovasc Surg. 2011;141:107–12.
Kobayashi SA, Jamshidi R, O’Sullivan P, Palmer B, Hirose S, Stewart L, et al. Bringing the skills laboratory home: an affordable webcam-based personal trainer for developing laparoscopic skills. J Surg Educ. 2011;68:105–9.
Panait L, Hogle NJ, Fowler DL, Bell RL, Roberts KE, Duffy AJ. Completion of a novel, virtual-reality-based, advanced laparoscopic curriculum improves advanced laparoscopic skills in senior residents. J Surg Educ. 2011;68:121–5.
Zimmerman H, Latifi R, Dehdashti B, Ong E, Jie T, Galvani C, et al. Intensive laparoscopic training course for surgical residents: program description, initial results, and requirements. Surg Endosc. 2011;25:3636–41.
Varas J, Mejı´a R, Riquelme A, Maluenda F, Buckel E, Salinas J, Martı´nez J, Aggarwal R, Jarufe N, Boza C. Significant transfer of surgical skills obtained with an advanced laparoscopic training program to a laparoscopic jejunojejunostomy in a live porcine model: feasibility of learning advanced laparoscopy in a general surgery residency. Surg Endosc. 2012;26:3486–94.
Palter VN, Grantcharov TP. Development and validation of a comprehensive curriculum to teach an advanced minimally invasive procedure: a randomized controlled trial. Ann Surg. 2012;256:25–32.
Rinewalt D, Du H, Velasco JM. Evaluation of a novel laparoscopic simulation laboratory curriculum. Surgery. 2012;152:550–6.
Teitelbaum EN, Soper NJ, Santos BF, Rooney DM, Patel P, Nagle AP, Hungness ES. A simulator-based resident curriculum for laparoscopic common bile duct exploration. Surgery. 2014;156:880–93.
Martin J, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84:273–8.
Hopmans CJ, den Hoed PT, van der Laan L, van der Harst E, van der Elst M, Mannaerts GH, et al. Assessment of surgery residents’ operative skills in the operating theater using a modified Objective Structured Assessment of Technical Skills (OSATS): a prospective multicenter study. Surgery. 2014;156:1078–88.
General Surgery Training Requirements. The AMERICAN BOARD of SURGERY. http://www.absurgery.org/default.jsp?certgsqe_training. Accessed 21 August 2016.
Hammond L, Ketchum J, Schwartz B. Accreditation council on graduate medical education technical skills competency compliance: urologic surgical skills. J Am Coll Surg. 2005;201:454–7.
Stefanidis D, Acker C, Swiderski D, Heniford B, Greene F. Challenges during the implementation of a laparoscopic skills curriculum in a busy general surgery residency program. J Surg Educ. 2008;65:4–7.
Vassiliou MC, Feldman LS. Objective assessment, selection, and certification in surgery. Surg Oncol. 2011;20:140–5.
Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondre K, Stanbridge D, et al. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg. 2005;190:107–13.
Kurashima Y, Feldman LS, Al-Sabah S, Kaneva PA, Fried GM, Vassiliou MC. A tool for training and evaluation of laparoscopic inguinal hernia repair: the Global Operative Assessment Of Laparoscopic Skills-Groin Hernia (GOALS-GH). Am J Surg. 2011;201:54–61.
Vaillancourt M, Ghaderi I, Kaneva PA, Vassiliou MC, Kolozsvari N, George I, et al. GOALS-incisional hernia: a valid assessment of simulated laparoscopic incisional hernia repair. Surg Innov. 2011;18:48–54.
Cox T, Seymour N, Stefanidis D. Moving the needle: simulation’s impact on patient outcomes. Surg Clin N Am. 2015;95:827–38.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kurashima, Y., Hirano, S. Systematic review of the implementation of simulation training in surgical residency curriculum. Surg Today 47, 777–782 (2017). https://doi.org/10.1007/s00595-016-1455-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1455-9