Abstract
Purpose
To clarify the feasibility and utility of reduced port surgery (RPS) for achalasia.
Methods
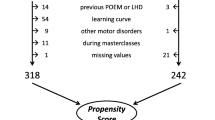
Between September 2005 and June 2013, 359 patients with esophageal achalasia, excluding cases of reoperation, underwent laparoscopic Heller myotomy and Dor fundoplication (LHD) according to our clinical pathway. Three-hundred and twenty-seven patients underwent LHD with five incisions (conventional approach), while the other 32 patients underwent RPS, including eight via SILS. The clinical data were collected in a prospective fashion and retrospectively reviewed. We selected 24 patients matched for gender, age and morphologic type with patients in the RPS group from among the 327 patients (C group). The surgical outcomes were compared between the C and RPS groups.
Results
There were no significant differences between the two groups in the duration of symptoms, dysphagia score, chest pain score, shape of the distal esophagus and esophageal clearance. The operative time was significantly longer in the RPS group than in the C group (p < 0.001). There were no significant differences between the two groups in the length of postoperative hospital stay or rates of bleeding, mucosal injury of the esophagus and/or stomach and postoperative complications. The symptom scores significantly improved after surgery in both groups (p < 0.001). Furthermore, there were no significant differences between the C group and RPS group in terms of the postoperative symptom scores or satisfaction scores after surgery.
Conclusions
The surgical outcomes of RPS for achalasia are comparable to those obtained with the conventional method.



Similar content being viewed by others
References
Miyazaki Y, Nakajia K, Sumikawa M, Yamasaki M, Takahashi T, Miyata H, et al. Magnetic resonance imaging for simultaneous morphological and functional evaluation of esophageal motility disorders. Surg Today. 2014;44:668–76.
Tsiaoussis J, Athanasakis E, Pechlivanides G, Tzortzinis A, Gouvas N, Mantides A, et al. Long-term functional results after laparoscopic surgery for esophageal achalasia. Am J Surg. 2007;193:26–31.
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, et al. Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg. 2008;248:986–93.
Mattioli S, Ruffato A, Lugaresi M, Pilotti V, Aramini B, D’Ovidio F. Long-term results of the Heller-Dor operation with intraoperative manometry for the treatment of esophageal achalasia. J Thorac Cardiovasc Surg. 2010;140:962–9.
Katada N, Sakuramoto S, Yamashita K, Hosoda K, Shibata T, Moriya H, et al. Comparison of the Heller-Toupet procedure with the Heller-Dor procedure in patients who underwent laparoscopic surgery for achalasia. Surg Today. 2014;44:732–9.
Qiu J, Yuan H, Chen S, He Z, Han P, Wu H. Single-Port versus conventional multiport laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials and nonrandomized studies. J Laparoendosc Adv Surg Tech A. 2013;23:815–31.
Cai YL, Xiong XZ, Wu SJ, Cheng Y, Lu J, Zhang J, et al. Single-incision laparoscopic appendectomy vs conventional laparoscopic appendectomy: systematic review and meta-analysis. World J Gastroenterol. 2013;19:5165–73.
Fan Y, Wu SD, Kong J, Su Y, Tian Y, Yu H. Feasibility and safety of single-incision laparoscopic splenectomy: a systematic review. J Surg Res. 2014;186:354–62.
Takata A, Nakajima K, Kurokawa Y, Takahashi T, Yamasaki M, Miyata H, et al. Single-incision laparoscopic partial gastrectomy for gastric submucosal tumors without compromising transumbilical stapling. Asian J Endosc Surg. 2014;7:25–30.
Mittermair R. Transumbilical single-incision laparoscopic sleeve gastrectomy: short-term results and technical considerations. J Minim Access Surg. 2013;9:104–8.
Kwag SJ, Kim JG, Oh ST, Kang WK. Single incision vs conventional laparoscopic anterior resection for sigmoid colon cancer: a case-matched study. Am J Surg. 2013;206:320–5.
Omura N, Kashiwagi H, Ishibashi Y, Yano F, Tsuboi K, Kawasaki N, et al. Laparoscopic Heller myotomy and Dor fundoplication for the treatment of achalasia: assessment in relation to morphologic type. Surg Endosc. 2006;20:210–3.
Kostic SV, Rice TW, Baker ME, DeCamp MM, Murthy SC, Rybicki LA, et al. Timed barium esophagogram: a simple physiologic assessment for achalasia. J Thorac Cardiovasc Surg. 2000;120:935–46.
Omura N, Kashiwagi H, Yano F, Tsuboi K, Ishibashi Y, Hoshino M, et al. Effect of laparoscopic esophagomyotomy on chest pain associated with achalasia and prediction of therapeutic outcomes. Surg Endosc. 2011;25:1048–53.
Burpee SE, Mamazza J, Schlachta CM, Bendavid Y, Klein L, Moloo H, et al. Objective analysis of gastroesophageal reflux after laparoscopic heller myotomy: an anti-reflux procedure is required. Surg Endosc. 2005;19:9–14.
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanström LL. Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg. 2005;140:827–34.
Rossetti G, Brusciano L, Amato G, Maffettone V, Napolitano V, Russo G, et al. A total fundoplication is not an obstacle to esophageal emptying after heller myotomy for achalasia: results of a long-term follow up. Ann Surg. 2005;241:614–21.
Shimi S, Nathanson LK, Cuschieri A. Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb. 1991;36:152–4.
Yamada H, Yano T. Single incision laparoscopic approach for esophageal achalasia: a case report. Int J Surg Case Rep. 2013;4:1–4.
Yano F, Omura N, Tsuboi K, Hoshino M, Yamamoto SR, Kashiwagi H, et al. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surg Today. 2012;42:299–302.
Kobayashi M, Mizuno M, Sasaki A, Arisue A, Akiyama S, Wakabayashi G. Single-port laparoscopic Heller myotomy and Dor fundoplication: initial experience with a new approach for the treatment of pediatric achalasia. J Pediatr Surg. 2011;46:2200–3.
Nakajima J, Sasaki A, Obuchi T, Baba S, Umemura A, Wakabayashi G. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surg Today. 2011;41:1543–7.
Barry L, Ross S, Dahal S, Morton C, Okpaleke C, Rosas M, et al. Laparoendoscopic single-site Heller myotomy with anterior fundoplication for achalasia. Surg Endosc. 2011;25:1766–74.
Conflict of interest
Nobuo Omura and the other co-authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Omura, N., Yano, F., Tsuboi, K. et al. Short-term surgical outcomes of reduced port surgery for esophageal achalasia. Surg Today 45, 1139–1143 (2015). https://doi.org/10.1007/s00595-014-1109-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-1109-8