Abstract
Aims
Atherogenic Index of Plasma (AIP) has been proposed as a novel marker of plasma atherogenicity, but its longitudinal predictive value in type 2 diabetes mellitus (T2DM) remains unclear. We aimed to assess the associations of AIP and its longitudinal transition with T2DM among middle-aged and older Chinese.
Methods
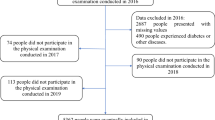
Data were extracted from four rounds of the China Health and Retirement Longitudinal Study (2011, 2013, 2015, and 2018). AIP was calculated as log10 (triglyceride/high-density lipoprotein cholesterol). Participants were classified into high and low AIP groups at baseline, and subsequently into four transition patterns during follow-up: maintained-high, maintained-low, high-to-low, and low-to-high AIP. Multivariable Cox frailty models were applied to explore the longitudinal transition patterns of AIP on the development of T2DM.
Results
A total of 8760 subjects without T2DM were selected in 2011, of which 981 developed T2DM until 2018. When compared with people with maintained-low AIP patterns, those with transition patterns of maintained-high AIP, high-to-low AIP, and low-to-high AIP were at around 1.5 times higher risk of T2DM (HRadj = 1.69, 1.32, and 1.47, respectively, all P < 0.05). However, the risk of T2DM did not decrease in the high-to-low AIP group as compared to the maintained-high AIP group.
Conclusions
Three longitudinal AIP transition patterns (maintained-high AIP, high-to-low AIP, and low-to-high AIP) were associated with the development of T2DM. Preventions are needed to combat T2DM at an early dyslipidemic stage.



Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available from [CHARLS Database] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of [CHARLS].
Code availability
Some codes generated during the study are available from the corresponding author by request.
References
The L (2017) Diabetes: a dynamic disease. Lancet (London, England) 389(10085):2163
Cho NH, Shaw JE, Karuranga S et al (2018) IDF diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281
Chen L, Magliano DJ, Zimmet PZ (2012) The worldwide epidemiology of type 2 diabetes mellitus–present and future perspectives. Nat Rev Endocrinol 8(4):228–236
ID Federation (2019) IDF diabetes Atlas
Chinese Diabetes Society (2021) Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2020 Edition). Chin J Diabetes Mellitus 13(04):315–409
Fletcher B, Gulanick M, Lamendola C (2002) Risk factors for type 2 diabetes mellitus. J Cardiovasc Nurs 16(2):17–23
Chehade JM, Gladysz M, Mooradian AD (2013) Dyslipidemia in type 2 diabetes: prevalence, pathophysiology, and management. Drugs 73(4):327–339
Shahwan MJ, Jairoun AA, Farajallah A, Shanabli S (2019) Prevalence of dyslipidemia and factors affecting lipid profile in patients with type 2 diabetes. Diabetes Metabolic Syndrome 13(4):2387–2392
Dobiásová M, Frohlich J (2000) The new atherogenic plasma index reflects the triglyceride and HDL-cholesterol ratio, the lipoprotein particle size and the cholesterol esterification rate: changes during lipanor therapy. Vnitrni lekarstvi 46(3):152–156
Cai G, Shi G, Xue S, Lu W (2017) The atherogenic index of plasma is a strong and independent predictor for coronary artery disease in the Chinese Han population. Medicine 96(37)
Zhu X, Yu L, Zhou H et al (2018) Atherogenic index of plasma is a novel and better biomarker associated with obesity: a population-based cross-sectional study in China. Lipids Health Dis 17(1):37
Song P, Xu L, Xu J et al (2018) Atherogenic Index of Plasma is associated with body fat level in type 2 diabetes mellitus patients. Curr Vasc Pharmacol 16(6):589–595
Zhu XW, Deng FY, Lei SF (2015) Meta-analysis of Atherogenic Index of Plasma and other lipid parameters in relation to risk of type 2 diabetes mellitus. Prim Care Diabetes 9(1):60–67
Guo XM (2013) Analysis on serum homocysteine: Atherogenic Index of Plasma and non-HDL-C in patients with type 2 diabetes mellitus complicated with cerebral infarction. J Clin Exp Med 12:1327–1328
Li Z, Liu F (2010) Correlation analysis of Atherogenic Index of Plasma and c-reactive protein in patients with abnormal glucose tolerance. J Pract Med Techn 17:347–348
Lv XF, Zheng SH (2010) Atherogenic Index of Plasma is associated with early vascular endothelium-dependent vasodilatation function in patients with type 2 diabetes. Chin J Misdiagnosis 10:2269–2271
Manohar SM, Vaikasuvu SR, Deepthi K, Sachan A, Narasimha SR (2013) An association of hyperglycemia with plasma malondialdehyde and atherogenic lipid risk factors in newly diagnosed Type 2 diabetic patients. J Res Med Sci 18(2):89
Wu JM, Xu GY, Wu KG (2011) Atherogenic Index of Plasma and dorsalis pedis artery atherosclerosis. Clin Med China 27:273–276
Zhang RS, Qu W, Lin YL (2010) Clinical significance of determination of blood non-HDL-C, bilirubin levels and atherogenic Index of Plasma (AIP) in patients with DM2. J Radioimmunol 23:424–429
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G (2014) Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol 43(1):61–68
Zhao Y, Strauss J, Yang G et al (2013) China health and retirement longitudinal study–2011–2012 national baseline users’ guide. National School of Development, Peking University, Beijing, pp 1–56
Biggeri M, Nannini M, Putoto G (2018) Assessing the feasibility of community health insurance in Uganda: a mixed-methods exploratory analysis. Soc Sci Med 200:145–155
Song P, Wang H, Xia W, Chang X, Wang M, An L (2018) Prevalence and correlates of hyperuricemia in the middle-aged and older adults in China. Sci Rep 8(1):1–9
Chen C, Lu FC (2004) The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci 17(Suppl):1–36
Zhou B (2002) Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 23(1):5–10
James PA, Oparil S, Carter BL et al (2014) 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311(5):507–520
Steiner G, Vranic M (1982) Hyperinsulinemia and hypertriglyceridemia, a vicious cycle with atherogenic potential. Int J Obes 6:117–124
Li N, Fu J, Koonen DP, Kuivenhoven JA, Snieder H, Hofker MH (2014) Are hypertriglyceridemia and low HDL causal factors in the development of insulin resistance? Atherosclerosis 233(1):130–138
Goodpaster BH, Kelley DE (2002) Skeletal muscle triglyceride: marker or mediator of obesity-induced insulin resistance in type 2 diabetes mellitus? Current Diabet Report 2(3):216–222
Yang L, Shao J, Bian Y et al (2016) Prevalence of type 2 diabetes mellitus among inland residents in China (2000–2014): a meta-analysis. J Diabet Invest 7(6):845–852
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 394(10204):1145–1158
Bragg F, Holmes MV, Iona A et al (2017) Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 317(3):280–289
Wang M, Gong WW, Pan J et al (2020) Incidence and time trends of type 2 diabetes mellitus among adults in Zhejiang province, China, 2007–2017. J Diabet Res 2020
Collaboration NRF (2019) Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 569(7755):260–264
Acknowledgements
All authors thank the China Health and Retirement Longitudinal Study (CHARLS) for providing data. We are grateful to those who designed, conducted, and participated in this study.
Funding
This study has received no funding.
Author information
Authors and Affiliations
Contributions
PS and YZ designed the study. QY and ZR managed and analyzed the data. QY and GB prepared the first draft. SZ and SL reviewed and edited the manuscript, with comments from HW, PS, and YZ. All authors were involved in revising the paper and gave final approval of the submitted versions.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethical approval for all the CHARLS waves was granted from the Institutional Review Board at Peking University. The IRB approval number for the main household survey, including anthropometrics, is IRB00001052-11015; the IRB approval number for biomarker collection was IRB00001052-11014.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Eye Complications of Diabetes. Managed by Giuseppe Querques.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yi, Q., Ren, Z., Bai, G. et al. The longitudinal effect of the atherogenic index of plasma on type 2 diabetes in middle-aged and older Chinese. Acta Diabetol 59, 269–279 (2022). https://doi.org/10.1007/s00592-021-01801-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01801-y