Abstract
Background
There are two modified TLIF, including MIS-TLIF and TLIF through Wiltse approach (W-TLIF). Although both of the two minimally invasive surgical procedures can be effective in the treatment for lumbar degenerative diseases, no comparative analysis has been made so far regarding their clinical outcomes.
Objective
To compare the clinical outcomes of MIS-TLIF and W-TLIF for the treatment for single-segment degenerative lumbar diseases.
Methods
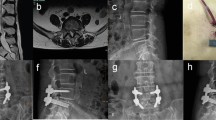
Ninety-seven patients with single-segment degenerative lumbar disorders were included in this study. Forty-seven underwent MIS-TLIF surgery (group A). For group B, fifty patients underwent W-TLIF. The Japanese Orthopedic Association (JOA) score, the visual analog scale (VAS) of low back pain (LBP) and leg pain, MRI score and atrophy rate of CSA, interbody fusion rate were assessed during the postoperative follow-up.
Results
Incision length, blood loss, operative time, CPK, and postoperative incision pain VAS were better in group A (P < 0.05). The seconds of intraoperative fluoroscopy in groups A and B were 76 ± 9 and 7 ± 2, respectively (P < 0.05). In group B, The blood loss and CPK at L5-S1 were significantly higher than those at L4-5. Postoperative JOA scores, VAS of leg pain, and fusion rate were statistically the same between the two groups. VAS of LBP, MRI score, and atrophy rate of CSA was better in group A than in group B (P < 0.05).
Conclusion
Both methods are effective in the treatment for lumbar degenerative disease. MIS-TLIF has less blood loss, shorter surgical incision, and less lower postoperative back pain, while W-TLIF is less expensive for hospital stay with lower exposure to X-rays.


Similar content being viewed by others
References
Bogduk N (1981) The lumbar mamillo-accessory ligament its anatomical and its neurosurgical significance. Spine 6:162–167
Panjabi M (1992) The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord 5:383–389
Kim K, Isu T, Sugawara A et al (2008) Comparison of the effect of 3 different approaches to the lumbar spinal canal on postoperative paraspinal muscle damage. Surg Neurol 69:109–113
Kotil K, Tunckale T, Tatar Z et al (2007) Serum creatine phosphokinase activity and histological changes in the multifidus muscle: a prospective randomized controlled comparative study of discectomy with or without retraction. J Neurosurg Spine 6:121–125
Mixter WJ (1937) Rupture of the lumbar intervertebral disk: an etiologic factor for so-called “sciatic” pain. Ann Surg 106:777–787
Sapega AA, Heppenstall RB, Change B et al (1985) Optimizing tourniquet application and release times in extremity surgery. J Bone Joint Surg Am 67:303–314
Watkins MB (1959) Posterolateral bone grafting for fusion of the lumbar and lumbosacral spine. J Bone Joint Surg Am 41:388–396
Wiltse LL, Bateman JG, Hutchinson RH et al (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 50:919–926
Wiltse LL, Spencer CW (1988) New uses and refinements of the paraspinal approach to the lumbar spine. Spine 13:696–706
Harms J, Rolinger H (1982) A one-stage procedure in operative treatment of spondylolisthesis: dorsal traction-reposition and anterior fusion. Z Orthop Ihre Grenzgeb 120:343–347
Foley KT, Lefkowitz MA (2002) Advances in minimally invasive spine surgery. Clin Neurosurg 49:499–517
Foley KT, Holly LT, Schwender JD (2003) Minimally invasive lumbar fusion. Spine 28:S26–S35
Lee KH, Yue WM, Yeo W et al (2012) Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 21:2265–2270
Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR (2014) Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res 472(6):1727–1737
Zheng Y, Liu X, Yuan S (2011) The clinical results of minimally invasive transforaminal lumbar interbody fusion through the Wiltse approach for the treatment of lumbar spondylolisthesis. Chin J Orthop 31:921–926
Liu X, Wang Y, Wu X, Zheng Y, Long Jia, Li J, Li J, Wei B (2010) Impact of surgical approaches on the lumbar multifidus muscle: an experimental study using sheep as models. J Neurosurg Spine 12(5):570–576
Fujiwara A, Kobayashi N, Saiki K et al (2003) Association of the Japanese orthopaedic association score with the oswestry disability index, Roland–Morris disability questionnaire, and short-form 36. Spine 28:1601–1607
Brantigan JW, Steffee AD, Lewis ML et al (2001) Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine 25:1437–1446
Wang MY, Cummock MD, Yu Y et al (2010) An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J Neurosurg Spine 12:694–699
Acknowledgments
This study was funded by the Natural Science Foundation of China. (Grant Number 81277024).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have not received research grants from any Company.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and National Research Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Tian, Y., Liu, X. Clinical outcomes of two minimally invasive transforaminal lumbar interbody fusion (TLIF) for lumbar degenerative diseases. Eur J Orthop Surg Traumatol 26, 745–751 (2016). https://doi.org/10.1007/s00590-016-1755-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1755-1