Abstract
Purpose
Gastroesophageal reflux disease (GERD) is reported as one of the symptoms of adult spinal deformity (ASD). Little is known about the mid- to long-term improvement in GERD symptoms after ASD surgery. Therefore, this retrospective study from prospectively collected database aimed to investigate GERD symptoms in patients for a minimum of 2 years after ASD corrective surgery.
Methods
Records from 230 patients (mean age: 64 years) who underwent ASD surgery were examined using the frequency scale for the symptoms of GERD (FSSG) questionnaires for the diagnosis of GERD. FSSG scores and radiographic parameters were investigated preoperatively and postoperatively at 6 months and 1, 2, and 5 years.
Results
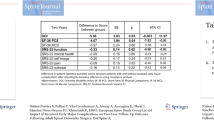
In total, 90 (39%) patients were preoperatively diagnosed with GERD defined by FSSG score ≥ 8 points. Radiographic results showed that the corrective surgeries improved local and global alignments. In the GERD patients, preoperative FSSG scores (16.1 ± 7.3 points) significantly improved to 7.7 ± 7.4 points within 6 months postoperatively (p < 0.001), and postoperative FSSG scores maintained at 1 year (9.9 ± 8.2 points, p = 0.061), 2 years (9.7 ± 8.2 points, p = 0.086), and 5 years (9.4 ± 8.0 points, p = 0.177). Among the GERD group, 62 patients (69%; improvement cases) showed improvement in GERD symptoms defined by FSSG score < 8 points within 6 months postoperatively.
Conclusions
Among ASD patients, 39% were diagnosed with GERD. In 69% of these patients, GERD symptoms improved within 6 months of corrective surgery and maintained up to 5 years postoperatively.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.





Similar content being viewed by others
References
Dreimann M, Hoffmann M, Kossow K, Hitzl W, Meier O, Koller H (2014) Scoliosis and chest cage deformity measures predicting impairments in pulmonary function: a cross-sectional study of 492 patients with scoliosis to improve the early identification of patients at risk. Spine (Phila Pa 1976) 39:2024–2033. https://doi.org/10.1097/brs.0000000000000601
Imagama S, Hasegawa Y, Wakao N, Hirano K, Hamajima N, Ishiguro N (2012) Influence of lumbar kyphosis and back muscle strength on the symptoms of gastroesophageal reflux disease in middle-aged and elderly people. Eur Spine J 21:2149–2157. https://doi.org/10.1007/s00586-012-2207-1
Hosogane N, Watanabe K, Yagi M, Kaneko S, Toyama Y, Matsumoto M (2017) Scoliosis is a risk factor for gastroesophageal reflux disease in adult spinal deformity. Clin Spine Surg 30:E480–E484. https://doi.org/10.1097/BSD.0000000000000263
Matsuzaki H, Makiyama K, Hoshino M, Oshima T (2016) High prevalence of laryngopharyngeal reflux disease in patients with lumbar kyphosis. J Voice 30:773–775. https://doi.org/10.1016/j.jvoice.2015.11.013
Melli MS, Alizadeh M (2007) Abnormal spinal curvature as a risk factor for pelvic organ prolapse. Pak J Biol Sci 10:4218–4223. https://doi.org/10.3923/pjbs.2007.4218.4223
Miyakoshi N, Kasukawa Y, Sasaki H, Kamo K, Shimada Y (2009) Impact of spinal kyphosis on gastroesophageal reflux disease symptoms in patients with osteoporosis. Osteoporos Int 20:1193–1198. https://doi.org/10.1007/s00198-008-0777-x
Quigley EM, Hungin AP (2005) Review article: quality-of-life issues in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 22(Suppl 1):41–47. https://doi.org/10.1111/j.1365-2036.2005.02608.x
Sugimoto M, Hasegawa T, Nishino M, Sahara S, Uotani T, Ichikawa H, Kagami T, Sugimoto K, Yamato Y, Togawa D, Kobayashi S, Hoshino H, Matsuyama Y, Furuta T (2016) Improvement of gastroesophageal reflux disease in Japanese patients with spinal kyphotic deformity who underwent surgical spinal correction. Dig Endosc 28:50–58. https://doi.org/10.1111/den.12543
Bridwell KH, Cats-Baril W, Harrast J, Berven S, Glassman S, Farcy JP, Horton WC, Lenke LG, Baldus C, Radake T (2005) The validity of the SRS-22 instrument in an adult spinal deformity population compared with the Oswestry and SF-12: a study of response distribution, concurrent validity, internal consistency, and reliability. Spine (Phila Pa 1976) 30:455–461. https://doi.org/10.1097/01.brs.0000153393.82368.6b
Gum JL, Bridwell KH, Lenke LG, Bumpass DB, Sugrue PA, Karikari IO, Carreon LY (2015) SRS22R appearance domain correlates most with patient satisfaction after adult deformity surgery to the sacrum at 5-year follow-up. Spine (Phila Pa 1976) 40:1297–1302. https://doi.org/10.1097/brs.0000000000000961
Smith JS, Shaffrey CI, Lafage V, Schwab F, Scheer JK, Protopsaltis T, Klineberg E, Gupta M, Hostin R, Fu KM, Mundis GM Jr, Kim HJ, Deviren V, Soroceanu A, Hart RA, Burton DC, Bess S, Ames CP, International Spine Study G (2015) Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine 23:349–359. https://doi.org/10.3171/2014.12.SPINE14777
Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K, Horikoshi T, Sugiyama T, Toki M, Ohwada T, Mori M (2004) Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol 39:888–891. https://doi.org/10.1007/s00535-004-1417-7
Kusano M, Ino K, Yamada T, Kawamura O, Toki M, Ohwada T, Kikuchi K, Shirota T, Kimura M, Miyazaki M, Nakamura K, Igarashi S, Tomizawa M, Tamura T, Sekiguchi T, Mori M (1999) Interobserver and intraobserver variation in endoscopic assessment of GERD using the “Los Angeles” classification. Gastrointest Endosc 49:700–704. https://doi.org/10.1016/s0016-5107(99)70285-3
Danjo A, Yamaguchi K, Fujimoto K, Saitoh T, Inamori M, Ando T, Shimatani T, Adachi K, Kinjo F, Kuribayashi S, Mitsufuji S, Fujiwara Y, Koyama S, Akiyama J, Takagi A, Manabe N, Miwa H, Shimoyama Y, Kusano M (2009) Comparison of endoscopic findings with symptom assessment systems (FSSG and QUEST) for gastroesophageal reflux disease in Japanese centres. J Gastroenterol Hepatol 24:633–638. https://doi.org/10.1111/j.1440-1746.2008.05747.x
Committee ASoP, Muthusamy VR, Lightdale JR, Acosta RD, Chandrasekhara V, Chathadi KV, Eloubeidi MA, Fanelli RD, Fonkalsrud L, Faulx AL, Khashab MA, Saltzman JR, Shaukat A, Wang A, Cash B, DeWitt JM (2015) The role of endoscopy in the management of GERD. Gastrointest Endosc 81:1305–1310. https://doi.org/10.1016/j.gie.2015.02.021
Pace F, Bollani S, Molteni P, Bianchi Porro G (2004) Natural history of gastro-oesophageal reflux disease without oesophagitis (NERD)—a reappraisal 10 years on. Dig Liver Dis 36:111–115. https://doi.org/10.1016/j.dld.2003.10.012
Nonaka T, Kessoku T, Ogawa Y, Yanagisawa S, Shiba T, Sakaguchi T, Atsukawa K, Takahashi H, Sekino Y, Iida H, Endo H, Sakamoto Y, Koide T, Takahashi H, Yoneda M, Maeda S, Nakajima A, Gotoh E, Inamori M (2013) Comparative Study of 2 Different Questionnaires in Japanese Patients: The Quality of Life and Utility Evaluation Survey Technology Questionnaire (QUEST) Versus the Frequency Scale for the Symptoms of Gastroesophageal Reflux Disease Questionnaire (FSSG). J Neurogastroenterol Motil 19:54–60. https://doi.org/10.5056/jnm.2013.19.1.54
Fujiwara Y, Arakawa T (2009) Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol 44:518–534. https://doi.org/10.1007/s00535-009-0047-5
Furukawa N, Iwakiri R, Koyama T, Okamoto K, Yoshida T, Kashiwagi Y, Ohyama T, Noda T, Sakata H, Fujimoto K (1999) Proportion of reflux esophagitis in 6010 Japanese adults: prospective evaluation by endoscopy. J Gastroenterol 34:441–444
Hampel H, Abraham NS, El-Serag HB (2005) Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med 143:199–211. https://doi.org/10.7326/0003-4819-143-3-200508020-00006
Ness-Jensen E, Lindam A, Lagergren J, Hveem K (2014) Tobacco smoking cessation and improved gastroesophageal reflux: a prospective population-based cohort study: the HUNT study. Am J Gastroenterol 109:171–177. https://doi.org/10.1038/ajg.2013.414
Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J (2003) Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA 290:66–72. https://doi.org/10.1001/jama.290.1.66
Yamaguchi T, Sugimoto T, Yamada H, Kanzawa M, Yano S, Yamauchi M, Chihara K (2002) The presence and severity of vertebral fractures is associated with the presence of esophageal hiatal hernia in postmenopausal women. Osteoporos Int 13:331–336. https://doi.org/10.1007/s001980200034
Khan M, Santana J, Donnellan C, Preston C, Moayyedi P (2007) Medical treatments in the short term management of reflux oesophagitis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd003244.pub2
Singh G, Triadafilopoulos G (2005) Appropriate choice of proton pump inhibitor therapy in the prevention and management of NSAID-related gastrointestinal damage. Int J Clin Pract 59:1210–1217. https://doi.org/10.1111/j.1368-5031.2005.00660.x
Acknowledgments
We appreciate the help of Yuki Mihara, Sho Kobayashi, and Daisuke Togawa for case collections or manuscript discussions. We would like to thank Editage (www.editage.jp) for English language editing. Dr. Matsuyama supervised the study. Dr. Hasegawa was responsible for the study’s conception and design. Dr. Hasegawa and Dr. Ushirozako acquired, analyzed, and interpreted data, drafted the article, and approved the final version on behalf of all authors. All authors have critically revised the article and reviewed the submitted version.
Funding
Dr. Oe and Yamato belong to a donation-funded laboratory called the “Division of Geriatric Musculoskeletal Health.” Donations to this laboratory have been received from Medtronic Sofamor Danek, Inc.; Japan Medical Dynamic Marketing, Inc.; and the Meitoku Medical Institution Jyuzen Memorial Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The other authors declare no conflicts of interest.
IRB approval
All study participants provided informed consent, and the study design was approved by the appropriate ethics review board of Hamamatsu University School of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hasegawa, T., Ushirozako, H., Yamato, Y. et al. Impact of adult spinal deformity corrective surgery in patients with the symptoms of gastroesophageal reflux disease: a 5-year follow-up report. Eur Spine J 29, 860–869 (2020). https://doi.org/10.1007/s00586-020-06300-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06300-2