Abstract
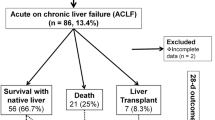
Liver transplantation has become a well-recognized transplant modality for children with end-stage liver disease. The first indicator to evaluate its efficiency is mortality rate. The aim of this study is to evaluate the complications and mortality of liver disease in children waiting for transplantation and understanding the risk factors that predict liver transplant waiting list death. This is a single-center prospective cohort study of all patient ≤18 years of age with chronic liver disease listed for liver transplantation. We analyzed medical records of 130 children for mortality risk factor. There were 52.3 % boys and 47.7 % girls with mean age of 8.6 ± 6.1 year (range, 3 months–18 year). The most common causes of cirrhosis were biliary atresia (21.5 %). The most common complication while awaiting transplantation was failure to thrive (76.2 %). Up to end of study, 20 patients (15.4 %) died without transplantation, 22 (16.9 %) of them transplanted, and 88 (67.7 %) of patients were alive while waiting for a liver transplantation. Mortality rate and transplantation ratio were 15.4 and 16.9 % with survival time waiting list 67.7 %. Factors which significantly associated with waiting list mortality included encephalopathy (p = 0.006), child score ≥10 (p = 0.036), model for end-stage liver disease (MELD) score ≥20 (p = 0.002), gastrointestinal bleeding (p = 0.004), Na (p = 0.046), and international normalized ratio (INR) (p = 0.018). A pediatric risk factor = (0.715 × Encephalopathy) + (0.152 × INR) − (0.022 × Na) was created. It had 90-day survival time 76.5 % for low risk group and 40.6 % for high risk group (p = 0.001) with ROC curve area 0.7 (95 % CI 0.599–0.796). The pediatric risk score such as MELD predicts the risk of liver transplantation waiting list mortality. Use of such scores in organ allocation in Iranian liver transplant unit may result in reduced waiting list mortality.



Similar content being viewed by others
References
Ben-Haim M, Carrniel M, Katz P, Shabtai E, Oren R, Nakache R (2006) Is the model of end-stage liver disease (MELD) valid in Israel? A critical analysis of liver transplant waiting list mortality. Indian Med Assoc J 8(9):605–9
Carey RG, Bucuvalas JC, Balistreri WF, Nick TG, Ryckman FR, Yazigi N (2010) Hyponatremia increases mortality in pediatric patients listed for liver transplantation. Pediatr Transplant 14(1):115–20
Dehghani SM, Gholami S, Bahador A, Nikeghbalian S, Salahi H, Imanieh MH et al (2007) Morbidity and mortality of children with chronic liver diseases who were listed for liver transplantation in Iran. Pediatr Transplant 11(1):21–3
Del Pino M, Cervio G, Dip M, Giannivelli S, Buamscha D, Ciocca M et al (2006) Mortality risk score in liver transplantation: changes over time in its predicting power. Pediatr Transplant 10(4):466–73
Fink MA, Berry SR, Gow PJ, Angus PW, Wang B-Z, Muralidharan V et al (2007) Risk factors for liver transplantation waiting list mortality. J Gastroenterol Hepatol 22(1):119–24
Gridelli B, Spada M, Riva S, Maggiore G (2008) Liver transplantation. In: Kleinman RE, Goulet OJ, Mieli-Vergani G, Sanderson I, Sherman P, Shneider B (eds) Walker's pediatric gastrointestinal disease, 5th edn. Hamilton, BC Decker Inc, USA, p 1149
McDiarmid SV, Anand R, Lindblad AS (2004) Studies of pediatric liver transplantation: 2002 update. An overview of demographics, indications, timing, and immunosuppressive practices in pediatric liver transplantation in the United States and Canada. Pediatr Transplant 8(3):284–94
Porrett PM, Baranov E, ter Horst M (2015) Serum hypoalbuminemia predicts late mortality on the liver transplant waiting list. Transplantation 99(1):158–63
Ryckman FC, Fisher RA, Pedersen SH, Balistreri WF (1992) Liver transplantation in children. Semin Pediatr Surg 1(2):162–72
Šumskienė J, Kupčinskas L, Pundzius J, Šumskas L (2005) Prognostic factors for short and longterm survival in patients selected for liver transplantation. Medicina 41(1):39–46
Acknowledgments
The present article was extracted from the thesis written by Naghi Dara and was financially supported by Shiraz University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dara, N., Dehghani, S.M., Safarpour, A. et al. Liver function, paraclinical tests, and mortality risk factors in pediatric liver transplant candidates. Comp Clin Pathol 25, 189–195 (2016). https://doi.org/10.1007/s00580-015-2168-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-015-2168-y