Abstract
Purpose
This prospective randomized study compared the coracoid and retroclavicular approaches to ultrasound-guided infraclavicular brachial plexus block (IBPB) in terms of needle tip and shaft visibility and quality of block. We hypothesized that the retroclavicular approach would increase needle tip and shaft visibility and decrease the number of needle passes compared to the coracoid approach.
Methods
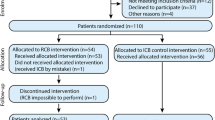
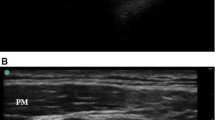
A total of 100 adult patients who received IBPB block for upper limb surgery were randomized into two groups: a coracoid approach group (group C) and a retroclavicular approach group (group R). In group C, the needle was inserted 2 cm medial and 2 cm inferior to the coracoid process and directed from ventral to dorsal. In group R, the needle insertion point was posterior to the clavicle and the needle was advanced from cephalad to caudal. All ultrasound images were digitally stored for analysis. The primary aim of the present study was to compare needle tip and shaft visibility between the coracoid approach and retroclavicular approach in patients undergoing upper limb surgery. The secondary aim was to investigate differences between the two groups in the number of needle passes, sensory and motor block success rates, surgical success rate, block performance time, block performance-related pain, patient satisfaction, use of supplemental local anesthetic and analgesic, and complications.
Results
Needle tip visibility and needle shaft visibility were significantly better in group R (p = 0.040, p = 0.032, respectively). Block performance time and anesthesia-related time were significantly shorter in group R (p = 0.022, p = 0.038, respectively). Number of needle passes was significantly lower in group R (p = 0.044). Paresthesia during block performance was significantly higher in group C (p = 0.045). There were no statistically significant differences between the two groups in terms of sensory or motor block success, surgical success, block-related pain, and patient satisfaction.
Conclusion
The retroclavicular approach is associated with better needle tip and shaft visibility, reduced performance time and anesthesia-related time, less paresthesia during block performance, and fewer needle passes than the coracoid approach.
Trıal registry number
Clinicaltrials.gov (no. NCT02673086).




Similar content being viewed by others
References
Raj PP, Montgomery SJ, Nettles D, Jenkins MT. Infraclavicular brachial plexus block—a new approach. Anesth Analg. 1973;52:897–904.
Desroches J. The infraclavicular brachial plexus block by the coracoid approach is clinically effective: an observational study of 150 patients. Can J Anaesth. 2003;50:253–7.
Gürkan Y, Hoşten T, Solak M, Toker K. Lateral sagittal infraclavicular block: clinical experience in 380 patients. Acta Anaesthesiol Scand. 2008;52:262–6.
Mosaffa F, Gharaei B, Rafeeyan M, Gachkar L. Comparing vertical and coracoid approaches for infraclavicular block in orthopedic surgery of the forearm and hand. J Clin Anesth. 2012;24:196–200.
Wilson JL, Brown DL, Wong GY, Ehman RL, Cahill DR. Infraclavicular brachial plexus block: parasagittal anatomy important to the coracoid technique. Anesth Analg. 1998;87:870–3.
Bocquet JD, N’takpe N, Draganescu C, Ridarch A, Jullien YR. The coracoid block: demonstration of a simple approach using the pectoralis minor as landmark. Can J Anaesth. 2005;52:1040–6.
Neal JM, Gerancher JC, Hebl JR, Ilfeld BM, McCartney CJ, Franco CD, Hogan QH. Upper extremity regional anesthesia: essentials of our current understanding, 2008. Reg Anesth Pain Med. 2009;34:134–70.
Macfarlane A, Anderson K. Infraclavicular brachial plexus block. Continuing education in anaesthesia. Crit Care Pain. 2009;9:139–43.
Charbonneau J, Fréchette Y, Sansoucy Y, Echave P. The ultrasound-guided retroclavicular block: a prospective feasibility study. Reg Anesth Pain Med. 2015;40:605–9.
Hebbard P, Royse C. Ultrasound guided posterior approach to the infraclavicular brachial plexus. Anaesthesia. 2007;62:539.
Taboada M, Rodriquez J, Amor M. Is ultrasound guidance superior to conventional nerve stimulation for coracoid infraclavicular brachial plexus block? Reg Anesth Pain Med. 2009;34:357–60.
Yazer MS, Finlayson RJ, Tran DQ. A randomized comparison between infraclavicular block and targeted intracluster injection supraclavicular block. Reg Anesth Pain Med. 2015;40:11–5.
Jandzinski DI, Carson N, Davis D, Rubens DJ, Voci SL, Gottlieb RH. Treated needles: do they facilitate sonographically guided biopsies? J Ultrasound Med. 2003;22:1233–7.
Schwemmer U, Geppert T, Steinfeldt T, Wunder C. Improvement of sonographic visualization of cannula needle tips by alignment of the needle lumen: in vitro investigation of established needle tip forms. Anaesthesist (in press).
Soeding P, Eizenberg N. Review article: anatomical considerations for ultrasound guidance for regional anesthesia of the neck and upper limb. Can J Anaesth. 2009;56:518–33.
Frederiksen BS, Koscielniak-Nielsen ZJ, Jacobsen RB, Rasmussen H, Hesselbjerg L. Procedural pain of an ultrasound-guided brachial plexus block: a comparison of axillary and infraclavicular approaches. Acta Anaesthesiol Scand. 2010;54:408–13.
Tran DQ, Russo G, Muñoz L, Zaouter C, Finlayson RJ. A prospective, randomized comparison between ultrasound-guided supraclavicular, infraclavicular, and axillary brachial plexus blocks. Reg Anesth Pain Med. 2009;34:366–71.
Wang FY, Wu SH, Lu IC, Hsu HT, Soo LY, Tang CS, Chu KS. Ultrasonographic examination to search out the optimal upper arm position for coracoid approach to infraclavicular brachial plexus block—a volunteer study. Acta Anaesthesiol Taiwan. 2007;45:15–20.
Ruíz A, Sala X, Bargalló X, Hurtado P, Arguis MJ, Carrera A. The influence of arm abduction on the anatomic relations of infraclavicular brachial plexus: an ultrasound study. Anesth Analg. 2009;108:364–6.
Pianezza A, Salces y Nedeo A, Chaynes P, Bickler PE, Minville V. The emergence level of the musculocutaneous nerve from the brachial plexus: implications for infraclavicular nerve blocks. Anesth Analg. 2012;114:1131–3.
Sutton EM, Bullock WM, Gadsden J. The retroclavicular brachial plexus block: additional advantages. Reg Anesth Pain Med. 2015;40:733–4.
Author information
Authors and Affiliations
Contributions
N.K.O. and A.S.K. conceived and performed the study, analyzed the data, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors of this manuscript have any conflict of interest to declare.
Funding
Departmental resources were used for the study.
About this article
Cite this article
Kavrut Ozturk, N., Kavakli, A.S. Comparison of the coracoid and retroclavicular approaches for ultrasound-guided infraclavicular brachial plexus block. J Anesth 31, 572–578 (2017). https://doi.org/10.1007/s00540-017-2359-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2359-6