Abstract
Background
Dexmedetomidine is a useful anesthetic adjuvant for general anesthesia. We determined whether preoperative dexmedetomidine administration could reduce the half maximal effective concentration (EC50) of propofol for successful i-gel insertion without muscle relaxants.
Methods
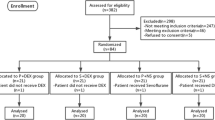
Thirty-seven patients were randomly allocated to one of two groups. In the dexmedetomidine group (n = 19), dexmedetomidine (1 µg/kg) was loaded for 10 min preoperatively. In the control group (n = 20), the same volume of 0.9 % normal saline was administered in the same manner. The EC50 of propofol for successful i-gel insertion was determined using Dixon’s up-and-down method. The EC50 of propofol was calculated as the midpoint concentration after at least six crossover points had been obtained. For successful i-gel insertion, all of the following four factors were required—(1) no major movement of the body within 1 min of insertion, (2) no significant resistance to mouth opening, (3) cough ≤2, and (4) visible square wave capnogram without air leakage at a peak airway pressure of <10 cmH2O. Mean blood pressure (MBP) and heart rate (HR) were monitored during the peri-insertion period of i-gel.
Results
The EC50 of propofol for successful i-gel insertion was 3.18 μg/mL in the dexmedetomidine group and 6.75 μg/mL in the control group (p < 0.001). The incidence of hypotension (MBP <80 % of the baseline) during the peri-insertion period of i-gel was higher in the control group (p = 0.001), whereas the incidence of bradycardia (HR <80 % of the baseline) was higher in the dexmedetomidine group (p = 0.001).
Conclusions
Preoperative dexmedetomidine reduced the EC50 of propofol for successful i-gel insertion without muscle relaxants.



Similar content being viewed by others
References
Haske D, Schempf B, Gaier G, Niederberger C. Performance of the i-gel during pre-hospital cardiopulmonary resuscitation. Resuscitation. 2013;84:1229–32.
Donaldson W, Michalek P. The use of an i-gel supraglottic airway for the airway management of a patient with subglottic stenosis: a case report. Minerva Anestesiol. 2010;76:369–72.
Emmerich M, Tiesmeier J. The i-gel supraglottic airway: a useful tool in case of difficult fiberoptic intubation. Minerva Anestesiol. 2012;78:1169–70.
Kim YL, Seo DM, Shim KS, Kim EJ, Lee JH, Lee SG, Ban JS. Successful tracheal intubation using fiberoptic bronchoscope via an i-gel supraglottic airway in a pediatric patient with Goldenhar syndrome − a case report. Korean J Anesthesiol. 2013;65:61–5.
Kosucu M, Eroglu A, Besir A, Cansu A. Using Proseal LMA and i-gel for difficult airway management in patient with diffuse tracheal stenosis and pulmonary artery sling. Bratisl Lek Listy. 2013;114:418–20.
Ruetzler K, Gruber C, Nabecker S, Wohlfarth P, Priemayr A, Frass M, Kimberger O, Sessler DI, Roessler B. Hands-off time during insertion of six airway devices during cardiopulmonary resuscitation: a randomised manikin trial. Resuscitation. 2011;82:1060–3.
Barker P, Langton JA, Wilson IG, Smith G. Movements of the vocal cords on induction of anaesthesia with thiopentone or propofol. Br J Anaesth. 1992;69:23–5.
Brown GW, Patel N, Ellis FR. Comparison of propofol and thiopentone for laryngeal mask insertion. Anaesthesia. 1991;46:771–2.
Higuchi H, Adachi Y, Arimura S, Nitahara K, Satoh T. Oral clonidine premedication reduces the EC50 of propofol concentration for laryngeal mask airway insertion in male patients. Acta Anaesthesiol Scand. 2002;46:372–7.
Kodaka M, Okamoto Y, Koyama K, Miyao H. Predicted values of propofol EC50 and sevoflurane concentration for insertion of laryngeal mask Classic and ProSeal. Br J Anaesth. 2004;92:242–5.
Farag E, Argalious M, Abd-Elsayed A, Ebrahim Z, Doyle DJ. The use of dexmedetomidine in anesthesia and intensive care: a review. Curr Pharm Des. 2012;18:6257–65.
Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth. 2011;55:352–7.
Kunisawa T, Ueno M, Kurosawa A, Nagashima M, Hayashi D, Sasakawa T, Suzuki A, Takahata O, Iwasaki H. Dexmedetomidine can stabilize hemodynamics and spare anesthetics before cardiopulmonary bypass. J Anesth. 2011;25:818–22.
Lee JH, Kim H, Kim HT, Kim MH, Cho K, Lim SH, Lee KM, Kim YJ, Shin CM. Comparison of dexmedetomidine and remifentanil for attenuation of hemodynamic responses to laryngoscopy and tracheal intubation. Korean J Anesthesiol. 2012;63:124–9.
Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S. Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation: perioperative haemodynamics and anaesthetic requirements. Drugs R D. 2006;7:43–52.
Scher CS, Gitlin MC. Dexmedetomidine and low-dose ketamine provide adequate sedation for awake fibreoptic intubation. Can J Anaesth. 2003;50:607–10.
Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, Youngs EJ. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502–16.
Park HJ, Lee JR, Kim CS, Kim SD, Kim HS. Remifentanil halves the EC50 of propofol for successful insertion of the laryngeal mask airway and laryngeal tube in pediatric patients. Anesth Analg. 2007;105:57–61.
Wharton NM, Gibbison B, Gabbott DA, Haslam GM, Muchatuta N, Cook TM. i-gel insertion by novices in manikins and patients. Anaesthesia. 2008;63:991–5.
Dixon WJ. Staircase bioassay: the up-and-down method. Neurosci Biobehav Rev. 1991;15:47–50.
Choi SC. Interval estimation of the LD50 based on an up-and-down experiment. Biometrics. 1990;46:485–92.
Jung H, Choi SC. Sequential method of estimating the LD50 using a modified up-and-down rule. J Biopharm Stat. 1994;4:19–30.
Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a precis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007;107:144–52.
Casati A, Fanelli G, Casaletti E, Cedrati V, Veglia F, Torri G. The target plasma concentration of propofol required to place laryngeal mask versus cuffed oropharyngeal airway. Anesth Analg. 1999;88:917–20.
Taylor IN, Kenny GN. Requirements for target-controlled infusion of propofol to insert the laryngeal mask airway. Anaesthesia. 1998;53:222–6.
Richebe P, Rivalan B, Baudouin L, Sesay M, Sztark F, Cros AM, Maurette P. Comparison of the anaesthetic requirement with target-controlled infusion of propofol to insert the laryngeal tube vs. the laryngeal mask. Eur J Anaesthesiol. 2005;22:858–63.
Guler G, Akin A, Tosun Z, Eskitascoglu E, Mizrak A, Boyaci A. Single-dose dexmedetomidine attenuates airway and circulatory reflexes during extubation. Acta Anaesthesiol Scand. 2005;49:1088–91.
Aksu R, Akin A, Bicer C, Esmaoglu A, Tosun Z, Boyaci A. Comparison of the effects of dexmedetomidine versus fentanyl on airway reflexes and hemodynamic responses to tracheal extubation during rhinoplasty: a double-blind, randomized, controlled study. Curr Ther Res Clin Exp. 2009;70:209–20.
Goyagi T, Tanaka M, Nishikawa T. Oral clonidine premedication reduces propofol requirement for laryngeal mask airway insertion. Can J Anaesth. 2000;47:627–30.
Dhungana Y, Bhattarai BK, Bhadani UK, Biswas BK, Tripathi M. Prevention of hypotension during propofol induction: a comparison of preloading with 3.5% polymers of degraded gelatin (Haemaccel) and intravenous ephedrine. Nepal Med Coll J. 2008;10:16–9.
Kamibayashi T, Maze M. Clinical uses of alpha2 -adrenergic agonists. Anesthesiology. 2000;93:1345–9.
Gupta A, Kaur S, Attri JP, Saini N. Comparative evaluation of ketamine-propofol, fentanyl-propofol and butorphanol-propofol on haemodynamics and laryngeal mask airway insertion conditions. J Anaesthesiol Clin Pharmacol. 2011;27:74–8.
Bailey PL, Streisand JB, East KA, East TD, Isern S, Hansen TW, Posthuma EF, Rozendaal FW, Pace NL, Stanley TH. Differences in magnitude and duration of opioid-induced respiratory depression and analgesia with fentanyl and sufentanil. Anesth Analg. 1990;70:8–15.
Dahan A, Aarts L, Smith TW. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226–38.
Christian CM 2nd, Waller JL, Moldenhauer CC. Postoperative rigidity following fentanyl anesthesia. Anesthesiology. 1983;58:275–7.
Grant SA, Breslin DS, MacLeod DB, Gleason D, Martin G. Dexmedetomidine infusion for sedation during fiberoptic intubation: a report of three cases. J Clin Anesth. 2004;16:124–6.
Snapir A, Posti J, Kentala E, Koskenvuo J, Sundell J, Tuunanen H, Hakala K, Scheinin H, Knuuti J, Scheinin M. Effects of low and high plasma concentrations of dexmedetomidine on myocardial perfusion and cardiac function in healthy male subjects. Anesthesiology. 2006;105:902–10 quiz 1069–70.
Hong JY, Kim WO, Yoon Y, Choi Y, Kim SH, Kil HK. Effects of intravenous dexmedetomidine on low-dose bupivacaine spinal anaesthesia in elderly patients. Acta Anaesthesiol Scand. 2012;56:382–7.
Kunisawa T, Nagata O, Nagashima M, Mitamura S, Ueno M, Suzuki A, Takahata O, Iwasaki H. Dexmedetomidine suppresses the decrease in blood pressure during anesthetic induction and blunts the cardiovascular response to tracheal intubation. J Clin Anesth. 2009;21:194–9.
Basar H, Akpinar S, Doganci N, Buyukkocak U, Kaymak C, Sert O, Apan A. The effects of preanesthetic, single-dose dexmedetomidine on induction, hemodynamic, and cardiovascular parameters. J Clin Anesth. 2008;20:431–6.
Shin HW, Yoo HN, Kim DH, Lee H, Shin HJ, Lee HW. Preanesthetic dexmedetomidine 1 microg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesia. Korean J Anesthesiol. 2013;65:114–20.
Menda F, Koner O, Sayin M, Ture H, Imer P, Aykac B. Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth. 2010;13:16–21.
Reddy SV, Balaji D, Ahmed SN. Dexmedetomidine versus esmolol to attenuate the hemodynamic response to laryngoscopy and tracheal intubation: a randomized double-blind clinical study. Int J Appl Basic Med Res. 2014;4:95–100.
Theiler L, Gutzmann M, Kleine-Brueggeney M, Urwyler N, Kaempfen B, Greif R. i-gel supraglottic airway in clinical practice: a prospective observational multicentre study. Br J Anaesth. 2012;109:990–5.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration Identifier: NCT02097407 (http://www.clinicaltrials.gov).
About this article
Cite this article
Jang, YE., Kim, YC., Yoon, HK. et al. A randomized controlled trial of the effect of preoperative dexmedetomidine on the half maximal effective concentration of propofol for successful i-gel insertion without muscle relaxants. J Anesth 29, 338–345 (2015). https://doi.org/10.1007/s00540-014-1949-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1949-9