Abstract
Background
Pain caused by intravenous injection of the muscle relaxant rocuronium bromide is common in children and adolescents. The cause of this unwanted effect is still unclear, and different pretreatment drugs have been administered in attempts to alleviate this side effect, with varying degrees of success.
Purpose
This study used a 60-s venous occlusion technique to evaluate the effectiveness of pretreatment with lidocaine, fentanyl, or remifentanil in preventing pain-induced withdrawal caused by intravenous injection of rocuronium bromide during the induction of general anesthesia.
Method
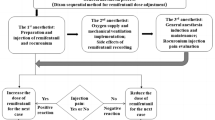
One hundred and one child and adolescent patients, ASA Ι–ΙΙ, requiring various surgical procedures under general anesthesia with muscle relaxation and mechanical ventilation, were enrolled. Patients were allocated randomly using computer-generated randomization into one of four pretreatment groups: a remifentanil group (1 µg/kg, n = 25), fentanyl group (1 µg/kg, n = 26), lidocaine 1 % group (0.5 mg/kg, n = 25), and normal saline group (n = 25). Drug doses were prepared in normal saline to a total volume of 5 ml. Venous occlusion was applied 10 cm above the venous access site. Pretreatment drugs were injected and retained for 60 s at the site of injection by an anesthetist blinded to group allocation. After release of the tourniquet, rocuronium (0.5 mg/kg) was then injected over 5 s, and withdrawal was recorded by another anesthetist blinded to group allocation. Descriptive statistics, analysis of variance, and a chi-squared test were used to statistically analyze the results as appropriate.
Results
Compared to normal saline, all other pretreatment groups scored a significantly lower mean of withdrawal response (P < 0.001). Lidocaine was superior to both remifentanil (P < 0.05) and fentanyl (P < 0.05) in suppressing the withdrawal response to rocuronium injection. Remifentanil was superior to fentanyl in suppressing the withdrawal response caused by rocuronium injection (P < 0.001).
Conclusion
Using a venous occlusion technique for 60 s, lidocaine was found to be most effective in preventing the withdrawal effect caused by rocuronium injection in children and adolescents. Lidocaine was superior to remifentanil which, in turn, was more effective than fentanyl.
Similar content being viewed by others
References
Dalgleish DJ. Drugs which cause pain on intravenous injection. Anaesthesia. 2000;55:828–9.
Steegers MA, Robertson EN. Pain on injection of rocuronium bromide. Anesth Analg. 1996;83:203.
Borgeat A, Kwiatkowski D. Spontaneous movement associated with rocuronium. Is pain on injection the cause? Br J Anaesth. 1997;79:382–3.
Shevchenko Y, Jocson JC, McRae VA, Stayer SA, Schwartz RE, Rehman M, Choudhry DK. The use of lidocaine for preventing the withdrawal associated with the injection of rocuronium in children and adolescents. Anesth Analg. 1999;88:746–8.
Oh AY, Seo KS, Goo EK, Park YO, Kim SJ, Kim JH. Prevention of withdrawal movement associated with injection of rocuronium in children: comparison of remifentanil, alfentanil and fentanyl. Acta Anaesthesiol Scand. 2007;51:1190–3.
Cheong KF, Wong WH. Pain on injection of rocuronium: influence of two doses of lidocaine pretreatment. Br J Anaesth. 2000;84:106–7.
Memiş D, Turan A, Karamanlioğlu B, Süt N, Pamukçu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol, and fentanyl. Anesth Analg. 2002;94:1517–20.
Shin YH, Choi SJ, Jeong HY, Kim MH. Evaluation of dose effect of magnesium sulfate on rocuronium injection pain and hemodynamic changes by laryngoscopy and endotracheal intubation. Korean J Anesthesiol. 2011;60:329–33.
Abduşoğlu MN, Özkoçak I, Yurtlu BS, Hancı V, Okyay RD, Ayoğlu H. A subhypnotic dose of ketamine reduces pain associated with injection of propofol and rocuronium. Eur J Anaesthesiol. 2011;28:229–30.
Jeon Y, Ha JH, Lee JE, Lee HC, Ryu T, Kwak KH. Rocuronium induced withdrawal movement: influence of ketorolac or a combination of lidocaine and ketorolac pretreatment. Korean J Anesthesiol. 2013;64:25–8.
Kim JY, Kim JY, Kim YB, Kwak HJ. Pretreatment with remifentanil to prevent withdrawal after rocuronium in children. Br J Anaesth. 2007;98:120–3.
Lui JT, Huang SJ, Yang CY, Hsu JC, Lui PW. Rocuronium induced generalized spontaneous movement caused pulmonary aspiration. Chong Gung Med J. 2002;25:617–20.
Solomowitz BH. Intravenous cannulation: a different approach. Anesth Prog. 1993;40:20–2.
Kelment W, Arndt JO. Pain on i.v injection of some anesthetic agents is evoked by the unphysiological osmolarity or pH of their formulations. Br J Anaesth. 1991;66:189–95.
Ahmad N, Choy CY, Aris EA, Balan S. Preventing the withdrawal response associated with rocuronium injection: a comparison of fentanyl with lidocaine. Anesth Analg. 2005;100:987–90.
Massad IM, Abu Ali HM, Abu Halaweh SA, Badran IZ. Venous occlusion with lidocaine for preventing propofol induced pain: a prospective double blind randomized study. Saudi Med J. 2006;27:997–1000.
Lesniak A, Lipkowski AW. Opioid peptides in peripheral pain control. Acta Neurobiol Exp. 2011;71:129–38.
Blunk JA, Seifert F, Schmelz M, Reeh PW, Koppert W. Injection pain of rocuronium and vecuronium is evoked by direct activation of nociceptive nerve endings. Eur J Anaesthesiol. 2003;20:245–53.
Jaffe RA, Rowe MA. A comparison of the local anesthetic effects of meperidine, fentanyl, and sufentanil on dorsal root axons. Anesth Analg. 1996;83:776–81.
Gissen AJ, Gugino LD, Datta S, Miller J, Covino BG. Effects of fentanyl and sufentanil on peripheral mammalian nerves. Anesth Analg. 1987;66:1272–6.
Sari M, Lyilikci L, Bayindir S, Ellidokuz H, Gunerli A. Comparison of the effectiveness of pretreatment by fentanyl and remifentanil on rocuronium induced injection pain. Saudi Med J. 2008;29:374–8.
Chaudhary K, Gupta P, Gogia AR. A prospective, randomized, double-blind study to compare the efficacy of lidocaine + metoclopramide and lidocaine + ketamine combinations in preventing pain on propofol injection. J Anesth. 2013;27:402–6.
Hagenouw RR, Bridenbaugh PO, van Egmond J, Stuebing R. Tourniquet pain: a volunteer study. Anesth Analg. 1986;65:1175–80.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Abu-Halaweh, S.A., Aloweidi, A.K., Qudaisat, I.Y. et al. Pretreatment with remifentanil, fentanyl, or lidocaine to prevent withdrawal after rocuronium using venous occlusion technique in children and adolescents: a prospective randomized placebo-controlled double-blind study. J Anesth 28, 886–890 (2014). https://doi.org/10.1007/s00540-014-1836-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1836-4