Abstract
Background
The exacerbation of disease in patients with ulcerative colitis (UC) can greatly affect quality of life and can impose economic burdens. In Japan, a large nationwide registry for the medical reimbursement of UC patients has existed since 1975. We aimed to examine factors associated with UC exacerbation among patients newly diagnosed with mild UC using electronic data from the registry.
Methods
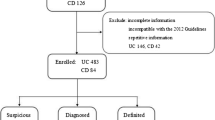
We retrospectively reviewed the clinical data of patients (n = 8120) newly diagnosed with mild UC between 2003 and 2011, and examined the association of patient background, medications, clinical symptoms and laboratory data, and pathological findings with exacerbation of UC, using the Cox proportional hazards model.
Results
The incidence of UC exacerbation was 94.6 per 1000 person-years (mean follow-up of 2.1 years). We found that male sex, age <17 years, an extensive lesion (left-sided colitis or pancolitis), overweight or obesity, hematochezia (mild or moderate-to-severe), mushy stools, frequency of bowel movements, and crypt architectural distortion were positively associated with UC exacerbation. On the other hand, age >40 years, high hemoglobin concentration, and high serum albumin levels were inversely associated with UC exacerbation among patients with mild UC in Japan.
Conclusion
Using data from the Japanese nationwide registry, we identified several factors, including body mass index and pathological findings, associated with disease exacerbation among patients with newly diagnosed mild UC. Our findings may lead to earlier recognition of exacerbation in patients with mild UC, thus enabling optimal care.

Similar content being viewed by others
Abbreviations
- UC:
-
Ulcerative colitis
- MHLW:
-
Ministry of Health, Labour and Welfare
- FH:
-
Family history
- Hb:
-
Hemoglobin
- BMI:
-
Body mass index
- 5-ASA:
-
5-Aminosalicylate
- CRP:
-
C-Reactive protein
- TP:
-
Total protein
- Alb:
-
Serum albumin
- ESR:
-
Erythrocyte sedimentation rate
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- SD:
-
Standard deviation
References
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105(3):501–23.
Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011;365(18):1713–25.
Cosnes J, Gower-Rousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140(6):1785–94.
Goh K, Xiao SD. Inflammatory bowel disease: a survey of the epidemiology in Asia. J Dig Dis. 2009;10(1):1–6.
Asakura K, Nishiwaki Y, Inoue N, et al. Prevalence of ulcerative colitis and Crohn’s disease in Japan. J Gastroenterol. 2009;44(7):659–65.
Morita N, Toki S, Hirohashi T, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30(Suppl 8):1–4.
Danese S, Sans M, Fiocchi C. Inflammatory bowel disease: the role of environmental factors. Autoimmun Rev. 2004;3(5):394–400.
Solberg IC, Lygren I, Jahnsen J, et al. Clinical course during the first 10 years of ulcerative colitis: results from a population-based inception cohort (IBSEN Study). Scand J Gastroenterol. 2009;44(4):431–40.
Hoie O, Wolters F, Riis L, et al. Ulcerative colitis: patient characteristics may predict 10-yr disease recurrence in a European-wide population-based cohort. Am J Gastroenterol. 2007;102(8):1692–701.
Romberg-Camps MJ, Dagnelie PC, Kester AD, et al. Influence of phenotype at diagnosis and of other potential prognostic factors on the course of inflammatory bowel disease. Am J Gastroenterol. 2009;104(2):371–83.
Futami S, Aoyama N, Honsako Y, et al. HLA-DRB1*1502 allele, subtype of DR15, is associated with susceptibility to ulcerative colitis and its progression. Dig Dis Sci. 1995;40(4):814–8.
Walker DG, Williams HR, Bancil AS, et al. Ethnicity differences in genetic susceptibility to ulcerative colitis: a comparison of Indian asians and white northern Europeans. Inflamm Bowel Dis. 2013;19(13):2888–94.
Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2(4947):1041–8.
Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol Journal canadien de gastroenterologie. 2005;19(Suppl A):5A–36A.
Lasson A, Simren M, Stotzer PO, et al. Fecal calprotectin levels predict the clinical course in patients with new onset of ulcerative colitis. Inflamm Bowel Dis. 2013;19(3):576–81.
Bitton A, Peppercorn MA, Antonioli DA, et al. Clinical, biological, and histologic parameters as predictors of relapse in ulcerative colitis. Gastroenterology. 2001;120(1):13–20.
Wibmer AG, Kroesen AJ, Grone J, et al. Predictors of permanent ileostomy after restorative proctocolectomy. Br J Surg. 2010;97(10):1561–6.
Canedo JA, Pinto RA, McLemore EC, et al. Restorative proctectomy with ileal pouch-anal anastomosis in obese patients. Dis Colon Rectum. 2010;53(7):1030–4.
Teixeira LG, Leonel AJ, Aguilar EC, et al. The combination of high-fat diet-induced obesity and chronic ulcerative colitis reciprocally exacerbates adipose tissue and colon inflammation. Lipids Health Dis. 2011;10:204.
Harper JW, Sinanan MN, Zisman TL. Increased body mass index is associated with earlier time to loss of response to infliximab in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(10):2118–24.
Azad S, Sood N, Sood A. Biological and histological parameters as predictors of relapse in ulcerative colitis: a prospective study. Saudi J Gastroenterol. 2011;17(3):194–8.
Kuwahara E, Asakura K, Nishiwaki Y, et al. Effects of family history on inflammatory bowel disease characteristics in Japanese patients. J Gastroenterol. 2012;47(9):961–8.
Lau A, Chande N, Ponich T, et al. Predictive factors associated with immunosuppressive agent use in ulcerative colitis: a case-control study. Aliment Pharmacol Ther. 2008;28(5):606–13.
Rutgeerts P, Vermeire S, Van Assche G. Mucosal healing in inflammatory bowel disease: impossible ideal or therapeutic target? Gut. 2007;56(4):453–5.
Acknowledgments
The members of this Japanese IBD research group were organized by the Ministry of Health, Labour and Welfare of Japan. This work was supported in part by Health and Labour Sciences Research Grants for research on intractable diseases from the Japanese Ministry of Health, Labour and Welfare. We would like to express our gratitude to a number of physicians and surgeons in Japan who were involved in UC treatment and who prepared the registration forms.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
YS has received lecture honoraria from Mitsubishi Tanabe Pharma Corporation, ZERIA Pharmaceutical Co., Ltd., and AbbVie GK. TM has received research grants from Eisai Co., Ltd., Mitsubishi Tanabe Pharma Corporation., AJINOMOTO PHARMACEUTICALS Co., Ltd., ZERIA Pharmaceutical Co., Ltd., Kyorin Pharmaceutical Co., Ltd., and JIMRO Co., Ltd., and has received lecture fees from Eisai Co., Ltd. MN has received lecture honoraria from Mitsubishi Tanabe Pharma Corporation, Eisai Co., and AbbVie GK. All remaining authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kuwahara, E., Murakami, Y., Nakamura, T. et al. Factors associated with exacerbation of newly diagnosed mild ulcerative colitis based on a nationwide registry in Japan. J Gastroenterol 52, 185–193 (2017). https://doi.org/10.1007/s00535-016-1209-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1209-x