Abstract
Background
The “resect and discard” strategy is beneficial for cost savings on screening and surveillance colonoscopy, but it has the risk to discard lesions with advanced histology or small invasive cancer (small advanced lesion; SALs). The aim of this study was to prove the principle of new “resect and discard” strategy with consideration for SALs using magnifying narrow-band imaging (M-NBI).
Methods
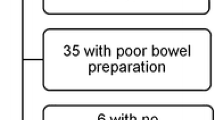
Patients undergoing colonoscopy at a tertiary center were involved in this prospective trial. For each detected polyp <10 mm, optical diagnosis (OD) and virtual management (“leave in situ”, “discard” or “send for pathology”) were independently made using non-magnifying NBI (N-NBI) and M-NBI, and next surveillance interval were predicted. Histological and optical diagnosis results of all polyps were compared.
Results
While the management could be decided in 82 % of polyps smaller than 10 mm, 24/31 (77 %) SALs including two small invasive cancers were not discarded based on OD using M-NBI. The sensitivity [90 % confidence interval (CI)] of M-NBI for SALs was 0.77 (0.61–0.89). The risk for discarding SALs using N-NBI was significantly higher than that using M-NBI (53 vs. 23 %, p = 0.02). The diagnostic accuracy (95 % CI) of M-NBI in distinguishing neoplastic from non-neoplastic lesions [0.88 (0.86–0.90)] was significantly better than that of N-NBI [0.84 (0.82–0.87)] (p = 0.005).
Conclusions
The results of our study indicated that our “resect and discard” strategy using M-NBI could work to reduce the risk for discarding SALs including small invasive cancer (UMIN-CTR, UMIN000003740).


Similar content being viewed by others
References
Ignjatovic A, East JE, Suzuki N, et al. Optical diagnosis of small colorectal polyps at routine colonoscopy (Detect InSpect ChAracterise Resect and Discard; DISCARD trial): a prospective cohort study. Lancet Oncol. 2009;10:1171–8.
Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol. 2010; 8: 865–9, 869. e1–3.
Loberg M, Kalager M, Holme O, et al. Long-term colorectal-cancer mortality after adenoma removal. N Engl J Med. 2014;371:799–807.
Hasaan C, Quintero E, Eumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2013;45:842–64.
Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on colorectal cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–95.
Hotta K, Imai K, Yamaguchi Y, et al. Diminutive submucosally invasive cancers of the colon and rectum. Endoscopy. 2015;18(Suppl 1):E2–3. doi:10.1055/s-0034-1377400.
Katagiri A, Fu KI, Sano Y, et al. Narrow-band imaging with magnifying colonoscopy as diagnostic tool for predicting histology of early colorectal neoplasia. Aliment Pharmacol Ther. 2008;27:1269–74.
Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy. 2004;36:1094–8.
Takeuchi Y, Hanafusa M, Kanzaki H, et al. Proposal of a new ‘resect and discard’ strategy using magnifying narrow-band imaging: pilot study of diagnostic accuracy. Dig Endosc. 2014;26(Suppl 2):90–7.
Standards for the reporting of diagnostic accuracy studies (STARD) statement. http://www.stard-statement.org/. Accessed 20 Feb 2013.
Takeuchi Y, Inoue T, Hanaoka N, et al. Autofluorescence imaging with a transparent hood for detection of colorectal neoplasms: a prospective, randomized trial. Gastorointest Endosc. 2010;72:1006–13.
Participants in the Paris Workshop. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon—November 30 to December 1, 2002. Gastrointest Endosc. 2003;58(Suppl):S3–43.
Dixon MF. Gastrointestinal epithelial neoplasia: Vienna revisited. Gut. 2002;51:130–1.
East JE, Suzuki N, Saunders BP. Comparison of magnified pit pattern interpretation with narrow-band imaging versus chromoendoscopy for diminutive colonic polyps: a pilot study. Gastrointest Endosc. 2007;66:310–6.
Hirata M, Tanaka S, Oka S, et al. Magnifying endoscopy with narrow-band imaging for diagnosis of colorectal tumors. Gastrointest Endosc. 2007;65:988–95.
Sano Y, Ikematsu H, Fu KI, et al. Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Gastrointest Endosc. 2009;69:278–83.
Kudo S, Hirota S, Nakajima T, et al. Colorectal tumours and pit pattern. J Clin Pathol. 1994;47:880–5.
Lambert R, Kudo SE, Vieth M, et al. Pragmatic classification of superficial neoplastic colorectal lesions. Gastrointest Endosc. 2009;70:1182–99.
Cairns S, Scholefield JH. Guidelines for colorectal cancer screening in high risk groups. Gut. 2002;51(Suppl 5):V1–2.
Rex DK, Kahi C, O’Brien M, et al. The American Society for Gastrointestinal Endoscopy PIVI on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73:419–22.
Arkin AC, Wachtel MS. How many patients are necessary to assess test performance. JAMA. 1990;263:275–8.
East JE, Suzuki N, Bassett P, et al. Narrow-band imaging with magnification for the characterization of small and diminutive colonic polyps: pit pattern and vascular pattern intensity. Endoscopy. 2008;40:811–7.
Gschwantler M, Kriwanek S, Langner E, et al. High-grade dysplasia and invasive carcinoma in colorectal adenomas: a multivariate analysis of the impact of adenoma and patient characteristics. Eur J Gastroenterol Hepatol. 2002;14:183–8.
Butterly LF, Chase MP, Pohl H, et al. Prevalence of clinically important histology in small adenomas. Clin Gastroenterol Hepatol. 2006;4:343–8.
Acknowledgments
This study was supported by a grant-in-aid from the Osaka Foundation for the Prevention of Cancer and Cardiovascular Diseases.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2015_1048_MOESM1_ESM.tif
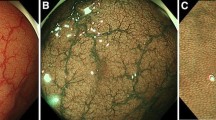
Supplementary material 1 S1a. Endoscopic and microscopic images of hyperplastic polyp. Non-magnifying narrow-band imaging (NBI) image of the lesion: The lesion shows weaker vascular pattern intensity. (TIFF 465 kb)
535_2015_1048_MOESM2_ESM.tif
Supplementary material 2 S1b. Endoscopic and microscopic images of hyperplastic polyp. Magnifying NBI image of the lesion: Microvascular architecture is arranged in a regular honeycomb pattern that was faintly visible or invisible. (TIFF 515 kb)
535_2015_1048_MOESM3_ESM.tif
Supplementary material 3 S1c. Endoscopic and microscopic images of hyperplastic polyp. Microscopic findings of the lesion: The histopathological diagnosis is hyperplastic polyps. (TIFF 4512 kb)
535_2015_1048_MOESM4_ESM.tif
Supplementary material 4 S2a. Endoscopic and microscopic images of low-grade adenoma. Non-magnifying narrow-band imaging (NBI) image of the lesion: The lesion shows stronger vascular pattern intensity. (TIFF 392 kb)
535_2015_1048_MOESM5_ESM.tif
Supplementary material 5 S2b. Endoscopic and microscopic images of low-grade adenoma. Magnifying NBI image of the lesion: Microvascular architecture is arranged in round to oval honeycomb-like pattern. (TIFF 418 kb)
535_2015_1048_MOESM6_ESM.tif
Supplementary material 6 S2c. Endoscopic and microscopic images of low-grade adenoma. Microscopic findings of the lesion: The histopathological diagnosis is low-grade adenoma. (TIFF 7319 kb)
535_2015_1048_MOESM7_ESM.tif
Supplementary material 7 S3a. Endoscopic and microscopic images of tubulovillous polyp. Non-magnifying narrow-band imaging (NBI) image of the lesion: The lesion shows stronger vascular pattern intensity, and the surface of the lesion seems not smooth. (TIFF 471 kb)
535_2015_1048_MOESM8_ESM.tif
Supplementary material 8 S3b. Endoscopic and microscopic images of tubulovillous polyp. Magnifying NBI image of the lesion: Microsurface pattern of the lesion shows blanched groove and villous pattern, resemble to Kudo Type IV pit pattern. (TIFF 493 kb)
535_2015_1048_MOESM9_ESM.tif
Supplementary material 9 S3c. Endoscopic and microscopic images of tubulovillous polyp. Microscopic findings of the lesion: The histopathological diagnosis is tubulovillous adenoma.(TIFF 6151 kb)
535_2015_1048_MOESM10_ESM.tif
Supplementary material 10 S4a. Endoscopic and microscopic images of small invasive cancer. Non-magnifying narrow-band imaging (NBI)image of the lesion: The lesion shows stronger vascular pattern intensity, and the surface of the lesion seems irregular. (TIFF 373 kb)
535_2015_1048_MOESM11_ESM.tif
Supplementary material 11 S4b. Endoscopic and microscopic images of small invasive cancer. Magnifying NBI image of the lesion: Microvascular architecture that was not arranged regularly in a honeycomb-like pattern and exhibited irregular size, complex branching, disruption and irregular winding. (TIFF 406 kb)
535_2015_1048_MOESM12_ESM.tif
Supplementary material 12 S4c. Endoscopic and microscopic images of small invasive cancer. Microscopic findings of the lesion: The histopathological diagnosis was submucosal (SM) invasive cancer. The depth of invasion is SM 3000 μm. (TIFF 5961 kb)
535_2015_1048_MOESM13_ESM.tiff
Supplementary material 13 S5. Relationship between predicted polyp types and polyp managements. Detected polyps were characterized for their histopathological findings according to non-magnifying narrow-band imaging (NBI) and magnifying NBI. In the case of diminutive non-neoplastic lesions located in the recto-sigmoid colon suspected, “leave in situ” is the management. In the case of low-grade adenoma predicted, “resect and discard” without formal histopathology is the management. Non-neoplastic polyps in the rest of the colon (right-sided colon or descending colon), or advanced lesions including invasive cancer determined, or polyps where there were difficulties in predicting type, were considered as requiring formal histopathology, and “resect and send” these lesions for formal histopathology. “Leave in situ” or “resect and discard” means they decided to omit the formal histopathology with a high confidence. (TIFF 6737 kb)
535_2015_1048_MOESM14_ESM.tiff
Supplementary material 14 S6. Flow diagram of the prediction of polyp type (optical diagnosis), decision on polyp management and the results of formal histopathology (reference standard) using non-magnifying narrow-band imaging (N-NBI). pts: patients; LGA: low-grade adenoma; leave: leave it in situ; discard: resect and discard; send: resect and send. (TIFF 10835 kb)
535_2015_1048_MOESM15_ESM.tif
Supplementary material 15 S7 a. Endoscopic images of the lesions diagnosed as neoplastic lesion according to non-magnifying narrow-band imaging (N-NBI) image, but non-neoplastic lesion according to magnifying NBI (M-NBI) image. N-NBI image of the lesion. The participated endoscopist diagnosed this lesion as neoplastic lesion. (TIFF 540 kb)
535_2015_1048_MOESM16_ESM.tif
Supplementary material 16 S7b. Endoscopic images of the lesions diagnosed as neoplastic lesion according to non-magnifying narrow-band imaging (N-NBI) image, but non-neoplastic lesion according to magnifying NBI (M-NBI) image. M-NBI image of the lesion. Microvascular architecture was arranged in a regular honeycomb pattern that was faintly visible. The endoscopist changed the diagnosis to non-neoplastic lesion. (TIFF 520 kb)
535_2015_1048_MOESM17_ESM.tif
Supplementary material 17 S7c. Endoscopic images of the lesions diagnosed as neoplastic lesion according to non-magnifying narrow-band imaging (N-NBI) image, but non-neoplastic lesion according to magnifying NBI (M-NBI) image. Pathological specimen disclosed normal colonic mucosa with inflammation. (TIFF 5597 kb)
535_2015_1048_MOESM18_ESM.tif
Supplementary material 18 S8a. Endoscopic images of the lesions diagnosed as non-neoplastic lesion according to non-magnifying narrow-band imaging (N-NBI), but neoplastic lesion according to magnifying NBI (M-NBI) image. N-NBI image of the lesion. The participated endoscopist diagnosed this lesion as non-neoplastic lesion. (TIFF 513 kb)
535_2015_1048_MOESM19_ESM.tif
Supplementary material 19 S8b. Endoscopic images of the lesions diagnosed as non-neoplastic lesion according to non-magnifying narrow-band imaging (N-NBI), but neoplastic lesion according to magnifying NBI (M-NBI) image. M-NBI image of the lesion. Microvascular architecture was arranged in round to oval honeycomb-like pattern. The endoscopist changed the diagnosis to neoplastic lesion. (TIFF 489 kb)
535_2015_1048_MOESM20_ESM.tif
Supplementary material 20 S8c. Endoscopic images of the lesions diagnosed as non-neoplastic lesion according to non-magnifying narrow-band imaging (N-NBI), but neoplastic lesion according to magnifying NBI (M-NBI) image. Pathological specimen disclosed low-grade adenoma. (TIFF 6252 kb)
Rights and permissions
About this article
Cite this article
Takeuchi, Y., Hanafusa, M., Kanzaki, H. et al. An alternative option for “resect and discard” strategy, using magnifying narrow-band imaging: a prospective “proof-of-principle” study. J Gastroenterol 50, 1017–1026 (2015). https://doi.org/10.1007/s00535-015-1048-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-015-1048-1