Abstract
Background
The esophageal intraluminal baseline impedance may be used to evaluate the status of mucosa integrity. Esophageal acid exposure decreases the baseline impedance. We aimed to compare baseline impedance in patients with various reflux events and with different acid-related parameters, and investigate the relationships between epithelial histopathologic abnormalities and baseline impedance.
Methods
A total of 229 GERD patients and 34 controls underwent 24-h multichannel intraluminal impedance and pH monitoring (MII–pH monitoring), gastroendoscopy, and completed a GERD questionnaire (GerdQ). We quantified epithelial intercellular spaces (ICSs) and expression of tight junction (TJ) proteins by histologic techniques.
Results
Mean baseline values in reflux esophagitis (RE) (1752 ± 1018 Ω) and non-erosive reflux disease (NERD) (2640 ± 1143 Ω) were significantly lower than in controls (3360 ± 1258 Ω; p < 0.001 and p = 0.001, respectively). Among NERD subgroups, mean baselines in the acid reflux group (2510 ± 1239 Ω) and mixed acid/weakly acidic reflux group (2393 ± 1009 Ω) were much lower than in controls (3360 ± 1258 Ω; p = 0.020 and p < 0.001, respectively). The mean baseline in severe RE patients was significantly lower than in mild RE patients (LA-C/D vs. LA-A/B: 970 ± 505 Ω vs. 1921 ± 1024 Ω, p < 0.001). There was a significant negative correlation between baseline value and acid exposure time (AET) (r = −0.41, p < 0.001), and a weak but significant correlation (r = −0.20, p = 0.007) between baseline value and weakly AET. Negative correlations were observed between ICS and the baseline impedance (r = −0.637, p < 0.001) and claudin-1 and the baseline impedance (r = −0.648, p < 0.001).
Conclusions
Patients with dominant acid reflux events and with longer AET have low baseline impedance. Baseline values are correlated with esophageal mucosal histopathologic changes such as dilated ICS and TJ alteration.
Similar content being viewed by others
Introduction
Twenty-four-hour multichannel intraluminal impedance and pH monitoring (MII–pH monitoring) is currently used for detection of reflux episodes in GERD patients. However, when there are no episodes of reflux or swallowing, the esophageal wall comes directly into contact with the MII–pH sensor catheter. As a result, the impedance value reflects the intrinsic electrical conductivity of the esophageal wall, and this is the so-called esophageal baseline impedance value.
Farre et al. [1] performed acid perfusion experiments and showed that the baseline impedance drops to and maintains a low value after acid perfusion. Kessing et al. [2] studied acid exposure in GERD patients and found that patients with pathologic acid exposure time (AET) and patients off proton pump inhibitor (PPI) therapy showed lower baseline impedance values than control subjects.
Acid exposure correlates with macroscopic and microscopic lesions in esophageal mucosa [3–6]. Bioimpedance spectroscopy can distinguish squamous epithelium from columnar epithelium in Barrett’s esophagus, which means mucosal structural change such as epithelial metaplasia can be identified by impedance baseline change [7]. Farre et al. [1] also demonstrated that impedance baseline measurements can be used to evaluate changes in the integrity of the esophageal mucosa after acid perfusion injury, and showed that baseline impedance is correlated with transepithelial resistance (TER), which reflects impaired mucosal structure. At the same time, they showed that the baseline impedance in GERD patients was lower than in healthy subjects, and found that different subtypes of GERD were associated with different low baseline levels. Taken together, these findings suggest that difference in baseline values in GERD patients may be related to the severity of mucosal structural abnormalities. Dilated intercellular space (DIS) in the epithelium is generally considered to be a structural marker of GERD, and may be regarded as an early injury to the integrity of the esophageal mucosa [8]. DIS occurs in association with a decrease in TER [9]. However, there is no direct evidence showing correlation between esophageal epithelial intercellular space (ICS) and baseline impedance.
Some studies have considered DIS as a manifestation of acid-induced damage to the intercellular junctional complex [3, 10]. Tight junctions (TJ) are a part of this complex, and are crucial for epithelial barrier functions. Some TJ proteins not only seal off the paracellular pathway, but also form paracellular ion channels and act as transporters [11]. In vitro cell culture experiments have shown that both acid and acidic bile salts decrease TER and increase permeability of esophageal epithelium in a dose-dependent manner in part by modulating the amount of claudin-1 and claudin-4 [12, 13]. Alterations in localization patterns of TJ proteins such as claudin-1, -3, and -4 have been reported in a chronic reflux esophagitis (RE) rat model [14, 15]. This raises the possibility TJ may also correlate with baseline impedance changes in GERD patients. No previous research has focused on the relation between TJ and in vivo mucosal electrical conductivity.
The aims of this study were (1) to evaluate whether baseline impedance values are related to various reflux events and different acid-related parameters in GERD patients and (2) to assess whether the baseline impedance is correlated with structural abnormalities such as DIS and TJ protein alteration.
Methods
Subjects
Consecutive patients newly referred to Peking University Third Hospital from June 2009 to Aug 2011 with typical GER symptoms according to the Montreal consensus for MII–pH monitoring were eligible for inclusion in this study. Patients were excluded if they were taking medication which could influence esophageal motor function or gastric acid secretion, or if they had history of peptic ulcer, gastrointestinal tumor or surgery, or primary or secondary severe esophageal motility disorders. Healthy volunteers with no digestive or systemic symptoms were recruited as controls. All subjects completed a GERD questionnaire (GerdQ) and underwent gastroendoscopy 1 week or less in advance of the MII–pH monitoring. Subjects were also excluded if at gastroendoscopy examination they were found to have abnormalities other than erosive esophagitis or chronic superficial gastritis. Only subjects who met the above criteria were included. The protocol for this study was approved by the Ethical Committee of Peking University Health Science Center. All subjects gave informed written consent before commencement of the study.
MII–pH monitoring and baseline value acquirement
All subjects underwent MII–pH monitoring using an ambulatory MII–pH monitoring system (Ohmega, MMS, Enschede, the Netherlands). The pH electrode was placed at 5 cm above the upper margin of the lower esophageal sphincter (LES), and six impedance values (z 1, z 2, z 3, z 4, z 5, and z 6) were recorded at six sites (3, 5, 7, 9, 15, and 17 cm above the LES, respectively). Baseline impedance values in each individual were selected in a manner blinded to the diagnostic results at three time points (around 10:30 am, 4:30 pm, and 00:30 am), avoiding values taken close to any period of swallowing or reflux. Each single baseline value represents the average value of three suitable baseline values around each time point. We analyzed variations in the baseline impedance over the six sites and variations throughout three time points during a 24-h interval (data shown in Supplementary Fig. 1). For the primary analysis, we selected baseline values from the second distal impedance channel (z 5, 5 cm above the LES), where there was a pH electrode to ensure that baseline values were taken only when pH > 6.
Study protocol
Diagnostic procedure
All subjects completed a GerdQ and those with scores higher than 8 were diagnosed as abnormal (GerdQ+) [16]. Subjects then underwent gastroendoscopy and the MII–pH monitoring. On the basis of the endoscopic results, GERD patients were subdivided into RE and non-erosive reflux disease (NERD). RE was defined as the presence of esophageal mucosal injury and was graded according to the criteria of the Los Angeles classification. Patients were considered to have NERD if there was an absence of visible esophageal mucosal injury during endoscopy, together with an abnormal esophageal AET (>4.2 %) and/or a positive symptom association probability (SAP, >95 %) to acid/nonacid reflux during MII–pH monitoring [17–19]. Asymptomatic healthy controls were identified by negative gastroendoscopic and MII–pH monitoring results.
Histopathological evaluation
A subset of subjects (n = 35, consecutively collected from Jan 2011 to Aug 2011) were biopsied and two biopsies were taken at 2 cm above the Z-line during gastroendoscopy, avoiding biopsy of any obvious erosive lesion. Biopsies were stained with hematoxylin and eosin (H&E). Expression and localization of claudin-1, claudin-3, and occludin in the esophageal epithelium were evaluated with immunohistochemistry (IHC) (for details, see Supplementary Methods). Tissue sections or whole biopsies that were not well prepared were excluded from further evaluation. Morphological analysis was performed in a manner blinded to other results in this study.
Data analysis
Gastroesophageal reflux parameters
Esophageal AET and weakly acid exposure time (WAET) in MII–pH monitoring were calculated using original data recorded by the MMS software package.
NERD patients were divided into four subgroups designated as the acid reflux group, weakly acidic reflux group, weakly alkaline reflux group, and mixed acid/weakly acidic reflux group, according to the dominant positive reflux events identified by MII–pH monitoring. These groups were defined as at least 35 acid reflux events, at least 18 weakly acidic reflux events, and at least 7 weakly alkaline reflux events or mixed positive events [20]. Healthy controls were excluded from the study if they reached the defined number for any of these reflux event categories.
ICS measurement under light microscopy
ICS was quantitatively measured on H&E sections under light microscopy (LM), in a manner similar to that previously described [21, 22]. The ICS morphological characteristics and measuring process were compared under LM and transmission electron microscopy (TEM). Each specimen was examined and photographed under the immersion objective (×100) using a Nikon E600 microscope. Ten random fields in the prickle layer of the squamous epithelium were captured so that each field contained a whole cell. Image-Pro Plus software (IPP, version 6.0, Media Cybernetics, CA, USA) was used to randomly draw 10 lines delineated through the ICS around each cell, thus measuring 100 ICS for each individual, and the mean ICS was then calculated.
Evaluation of protein expression by Image-Pro Plus
The expression of three TJ proteins on IHC sections was measured semi-quantitatively with IPP software, using the method introduced by Xavier et al. [23, 24]. Briefly, five images per individual at 1600 × 1200 pixel resolution under ×200 were captured. All images were captured under the same manual exposure settings with the auto-white turned off. The selected measurement parameter was integrated optical density (IOD). The optical density was calibrated systematically and the area of interest was extracted through the HSI mode with the following settings: hue, 0–30; saturation, 0–255; and intensity, 0–255. Then the image was converted to a grayscale-8 image, and its IOD was counted. The mean IOD for each image, which represented expression of a certain protein, was calculated by IOD/tissue area, and mean IOD for each individual was the mean value of the mean IODs in five images from the same individual.
Statistical analysis
All baseline values are expressed as mean ± SD as they were normally distributed. Other data are presented as median and interquartile range. The variation of baselines over the entire length of the esophagus and throughout the 24-h test period was analyzed by repeated measurement. One-way ANOVA was used to compare baselines among GERD subtypes and controls, and among NERD subtypes and controls, followed by LSD post hoc testing to determine differences between subgroups. Comparison of baselines for GerdQ± and LA classification were carried out by an independent samples Student’s t test. Pearson’s correlation statistics were used for correlation analysis of the histopathologic results and baselines as well as AET/WAET and baselines. Receiver operator characteristic (ROC) curves were used to evaluate optimum cutoff values for evaluation of the ability of baseline values to discriminate GERD patients. All test results with a p value less than 0.05 were considered statistically significant. Statistical analyses were completed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 229 (229 out of 561 MII–pH monitoring patients) consecutive first-visit GERD patients (106 males, mean age 51.4 years, range 18–80 years) and 34 healthy controls (14 males, mean age 43.0 years, range 27–58 years) who met the enrolment criteria and finished all required procedures were included in the final analysis. RE was identified in 79 patients and was classified as LA-A/B (mild) (65 patients) and LA-C/D (severe) (14 patients). A total of 150 patients were diagnosed as having NERD, and within the NERD subgroups, there were 14 patients in the acid reflux group, 79 in the weakly acidic reflux group, 7 in the weakly alkaline reflux group, and 47 patients in the mixed acid/weakly acidic reflux group. There were also 3 patients with all three kinds of positive reflux events and they were excluded from NERD subgroup analysis because this group was too small to establish statistical significance.
Detailed demographic data and MII–pH monitoring parameters for all subjects are summarized in Table 1.
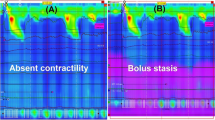
Acid-related GER parameters and baseline impedance
Mean baseline impedance values were significantly lower in RE and NERD patients than in healthy controls (1752 ± 1018 Ω vs. 3360 ± 1258 Ω, p < 0.001; 2640 ± 1143 Ω vs. 3360 ± 1258 Ω, p = 0.001) (Fig. 1a).
a Baselines in subgroups of GERD patients and controls. b Baselines in subgroups of NERD patients with different dominant reflux events and controls. c Correlation of acid exposure time (AET) and baseline impedance (r = −0.41, p < 0.001, n = 263). d Correlation of weakly acid exposure time (WAET) and baseline impedance (r = −0.20, p = 0.007, n = 263). Blue triangle delineates data distribution pattern. e Comparison of baseline in GerdQ (−) and GerdQ (+) individuals. f Comparison of baseline in mild RE patients (LA A/B, n = 65) and severe RE patients (LA C/D, n = 14). LA Los Angeles classification. Solid blue lines show mean values for each group. *p < 0.05, **p < 0.01
With regard to subgroups of NERD patients, mean baseline values were significantly lower in the acid reflux group (2510 ± 1239 Ω), weakly acidic reflux group (2801 ± 1156 Ω), and mixed acid/weakly acidic reflux group (2393 ± 1009 Ω) than those in healthy controls (3360 ± 1258 Ω; p = 0.020, p = 0.018, and p < 0.001, respectively) (Fig. 1b).
There was a significant negative correlation between baseline value and AET (r = −0.41, p < 0.001, n = 263) (Fig. 1c). A weak but significant correlation (r = −0.20, p = 0.007, n = 263) was also found between baseline value and WAET (Fig. 1d). The mean baseline in GerdQ (+) subjects (points ≥8, n = 133) was significantly lower than that in GerdQ (−) subjects (points <8, n = 126) (2200 ± 1153 Ω vs. 2709 ± 1244 Ω, p = 0.001) (Fig. 1e). In RE patients, the mean baseline in severe RE patients (LA-C/D, n = 14) was significantly lower than in mild RE patients (LA-A/B, n = 65) (970 ± 505 Ω vs. 1921 ± 1024 Ω, p < 0.001) (Fig. 1f).
Mucosal structural changes and baseline impedance
Photomicrographs of ICS measurement in RE patients and NERD patients are shown in Fig. 2a, b. A significant negative correlation was observed (r = −0.637, p < 0.001, n = 34) in comparing ICS and baseline impedance values (Fig. 2c). RE patients showed wider ICS [1.29 (1.10–1.46) μm, n = 6] than NERD patients [1.10 (0.95–1.21) μm, n = 16] and controls [1.01 (0.94–1.17) μm, n = 12; vs. RE, p = 0.027] (Fig. 2d). ICS measurements comparing LM and TEM are shown in Supplementary Fig. 2.
Photomicrographs of ICS measurement (H&E, immersion objective, ×100, bar 10 μm) showing relatively wide ICS a in RE group and narrow ICS b in NERD group. c Correlation of esophageal epithelial intercellular space (ICS) and impedance baselines (r = −0.637, p < 0.001, n = 34). d Median values for ICS in controls (n = 12), NERD (n = 16), and RE (n = 6) patients. *p < 0.05 versus controls
Claudin-1 and claudin-3 were found in abundance in the basal and prickle layers of the epithelium in a honeycomb-like pattern along cell borders (Fig. 3a, c). Occludin showed a dot-like or dense granule signal in the cytoplasm of the basal layer, and in the prickle layer but the latter was less intense (Fig. 3b). There was a significant negative correlation (r = −0.648, p < 0.001, n = 31) between the mean IOD of claudin-1 and baseline value, and a similar trend existed between occludin and baseline value but the latter was not significant (r = −0.317, p = 0.077, n = 32) (Fig. 3g, h). We also analyzed claudin-3 in the same manner but did not find any obvious correlation (Fig. 3i). Median IODs of claudin-1 in RE [0.14 (0.10–0.18), n = 6, p < 0.001] and NERD [0.08 (0.07–0.13), n = 13, p = 0.021] groups were significantly higher than in the controls [0.06 (0.04–0.07), n = 12] (Fig. 3j). The median IOD of occludin tended to be lower in the RE group and the median IODs of claudin-3 tended to be higher in the RE and NERD groups. However, none of these were significant (Fig. 3k, l).
Photomicrographs of immunohistochemical staining for TJ proteins claudin-1 (a), occludin (b), and claudin-3 (c) in RE group. Converted grayscale images (d–f) used to quantify respective IODs. Correlation between impedance baseline value and TJ proteins claudin-1 (g), occludin (h), and claudin-3 (i). Median values of mean IOD of claudin-1 (j), occludin (k), and claudin-3 (l) in controls, NERD, and RE patients. (×40, *p < 0.05 vs. controls, **p < 0.01 vs. controls)
Cutoff baseline values
Best cutoff values (2167 Ω) were determined and corresponding sensitivity, specificity, and areas under the ROC curves (AUCs) are given to show the ability of baselines to distinguish GERD patients (Fig. 4).
Discussion
In this study, we evaluated the influence of acid reflux on baseline impedance change, and investigated the relationship between esophageal epithelial histopathologic changes and baseline impedance.
Baseline impedance values in GERD patients were lower than in controls, and baselines in RE patients were even lower than in NERD patients. These results are in concordance with previous research [1]. The fundamental abnormality in GERD is exposure of the esophageal epithelium to reflux content, resulting in tissue injury and/or symptoms. Acid is the key element in reflux content in the production of esophagitis and/or microscopic alterations. On this basis, we speculate that low baseline values in GERD patients are the consequence of acid injury of esophageal mucosa. In addition, acid reflux is reported to increase across the spectrum of GERD [25], prompting out further speculation that RE patients have lower baseline values than NERD patients as they have severe acid exposure. This gave rise to exploration of the role of reflux acid in baseline changes.
All NERD patients were subgrouped according to their dominant reflux events. Patients in the acid reflux and weakly acidic reflux subgroups both had lower impedance baselines than controls, and not surprisingly, the subgroup with mixed positive events got the lowest baselines. These findings allow the conclusion that acid decreases baseline values. However, whether weakly acidic reflux also decreases baseline values needs to be further confirmed, as although the number of acid reflux events in the weakly acidic reflux subgroup did not reach a positive score (i.e., ≥35), the number was still higher than in the control group (16.5 ± 10.9 vs. 10.6 ± 12.1, p = 0.013). As such, low baseline values in the weakly acidic reflux subgroup may still be due to underlying acid reflux events. In order to make certain of the roles of acid and weakly acid in baseline impedance, we analyzed individual AET/WAET and baseline impedance value and found negative correlations in both. The scatter plots showed triangle-like distributions rather than linear distributions. A triangular distribution indicates that although individuals may have high or low baseline values when they have normal AET/WAET, they are very likely to show low baseline values when they have long AET/WAET. The r value for AET is higher than that for WAET, indicating that acid reflux affects impedance values more profoundly than weakly acid reflux does. However, weakly alkaline reflux appears to affect baselines much less than acid or weakly acidic reflux. One possible explanation is that the sample of seven individuals is relatively small for investigation. Alternatively, positive dominant weakly alkaline reflux alone is not sufficient to cause esophageal mucosal damage. The latter is supported by Farre’s study which showed that esophageal mucosa injury such as DIS can be evoked by exposure to bile acids in acid and weakly acidic conditions but not in neutral solutions [4].
GerdQ is a symptom-based six-item questionnaire that helps identify GERD patients. Baseline values in subjects with positive GerdQ were lower than in subjects with negative GerdQ. Another study done by our group found that GerdQ scores are positively correlated with acid reflux events in MII–pH monitoring [26], and Lacy et al. [27] also suggested that higher GerdQ scores are predictive of an abnormal pH study. Therefore, this symptom–baseline relation may still be interpreted as the consequence of abnormal acid exposure.
Acid is the most important factor in the reflux content affecting baselines. Microscopic epithelial structural abnormalities are found to various degrees in GERD patients, and they are largely considered to be the consequence of acid injury. In this study, we have shown a negative correlation between ICS and baseline impedance, suggesting that a low baseline can reflect subtle structural changes in the epithelium. Acid perfusion in the esophagus can provoke DIS [3–5] and most patients achieve recovery from DIS after PPI therapy [28–30]. Animal studies have shown that DIS is an indicator of impaired epithelial barrier function, reflected by increased paracellular permeability and decreased TER [3, 9, 10]. Farre et al. [1] demonstrated that TER in a rabbit model had a strong negative correlation with DIS, and the baseline impedance in the rabbit showed a good positive correlation with TER. But there were no direct data in that study showing correlation between DIS and impedance baseline, and most of the results were based on animal experiments. However, we have demonstrated that human baseline impedance is negatively correlated with ICS. Moreover, it may be inferred from the study by Farre et al. that DIS, as they measured it, would negatively correlate with their impedance baseline as well, as the TER they measured was a convincing parameter which was related to both. Our findings are also consistent with those of Tobey et al. [31] using an Ussing chamber to explore the physicochemical basis for DIS. They found that DIS is a hydrostatic consequence following a significant fluid shift into the ICS. This process was initiated by acid damage, characterized by an H+-induced increase in epithelial permeability and followed by Cl− diffusion into the ICS, creating an osmotic force for water movement into the ICS. A plausible explanation as to why the baseline value decreases with DIS is that baseline reflects intrinsic conductivity of the esophageal epithelium, and as such when the ICS loads with more fluid or ions than usual, the esophageal baseline impedance will decrease. This is also in accordance with the observation that RE patients have wider DIS and lower baselines than NERD patients as DIS is initiated by H+ in ICS and RE patients suffer more acid reflux events.
In addition to DIS, we also found a negative correlation between TJ proteins and baseline impedance, which is further evidence of the relationship between subtle epithelial structural alteration and baseline impedance. We analyzed claudin-1, claudin-3, and occludin proteins, and found that only claudin-1 had a significant negative correlation with the baseline value. Claudin-1 increased significantly from controls to RE patients, which is consistent with the previous research [14]. Claudin-3 seemed to have the same trend of increase as claudin-1, probably because they were members of the same family. The r value of claudin-3 was less significant than that of claudin-1, and this may imply that claudin-3 is less sensitive to changes of baseline impedance than claudin-1 is. In our study, occludin had no significant change from controls to RE patients, and this was consistent with other research [32]. Occludin was less significantly correlated with baseline impedance compared with claudin-1 probably because occludin was mainly distributed along the basal layer less broadly than claudins were. Epithelial cells have diverse mechanisms to change the structure and permeability of the TJ under inflammation [15]. TJ relates to inflammation and paracellular barrier defects, which lead to increased ion permeability of the paracellular pathway [33]. Also, claudins are considered important candidates for forming charge-selective channels in the paracellular pathway, and expression of claudins can affect paracellular conductance [11, 34, 35]. As the claudins are related to paracellular ion channel formation and ion selection, and they can modulate paracellular conductance and show change which occurs together with change in TER and/or DIS, it is unsurprising that claudin-1 shows a relation to the baseline impedance which is functionally an electrical parameter of the esophageal epithelium.
On the basis of the aforementioned results, baseline values in GERD patients are clearly affected by acid and show change which is associated with acid-related structural abnormalities. This raises the possibility that it is the inflammatory response that links them. Upon exposure to HCl, esophageal epithelial cells may be involved in the initiation of esophageal inflammation [36, 37]. Distal esophageal acid perfusion has been shown to not only provoke subtle changes in the exposed mucosa but also in the more proximal non-exposed mucosa [5]. RE patients have low baseline impedance in all six impedance sites, not only in the site near the erosive lesion. These studies suggest that acid initiates an inflammatory response that may lead to extensive subclinical changes in the mucosa structure. In other words, we speculate that acid decreases baseline impedance by inflammation-related mucosa changes.
Baseline values have been demonstrated to be lower in GERD patients in this and several other studies, but no previous study has calculated optimal cutoff baseline values for GERD diagnosis, and we therefore obtained cutoff values by ROC analysis. Establishing these cutoff values may allow new interpretation of the MII–pH monitoring results other than their existing value in diagnosing reflux, and also allow rapid assessment of the probability or severity of GERD. Although we suggest 2167 Ω as a cutoff baseline value for distinguishing GERD, this value is a suboptimal discriminator as it is obtained with imbalanced numbers between GERD patients and controls, and with a large overlap of baseline values in NERD patients and controls. The cutoff baselines can be universally applied only after they are accurately established, which means they should be re-evaluated using enlarged samples by a multicenter study. Our study at least gives a start, and also a clue that the baseline cutoff has clinical value and is worth further evaluation.
The limitations of this study are as follows: (1) ICS measurement in our study was done under LM instead of with the acknowledged technique of transmission electron microscope (TEM). However, another study [25] in our department showed that DIS obtained using LM correlates well with DIS obtained using TEM. In addition, on the basis of our experience with ICS measurement under TEM, there seems no great difference in choosing ICS in the measurement process as long as sections are well prepared (see Supplementary Fig. 2). (2) Quantification of TJ protein expression was done with IHC using generally accepted methodology, because we did not have sufficient biopsy tissues. It would have been better if other quantification methods such as Western blot analysis had been used.
This study reports for the first time on the relationship between baseline impedance and esophageal mucosal histopathologic changes such as DIS and TJ alteration. In addition, we evaluate the effect of acid on baseline values in a manner different from previous studies. Baseline impedance values are lower in patients with severe-type GERD, with dominant acid reflux events, with longer AET, and with higher GerdQ scores; these could all be attributed to increased acid exposure. Since acid has been demonstrated to cause histopathological changes such as DIS and TJ alteration, we consider that acid decreases baseline values through inflammatory responses and consequent structural changes in mucosa, which result in altered electrical conductivity of the esophageal wall. The clinical significance of baseline impedance study lies in its capacity to reflect subtle mucosal abnormalities and its ability to assist diagnostic identification of mild GERD patients who fail to show a typical positive result of MII–pH monitoring in a single day’s monitoring.
In summary, we demonstrate that baseline impedance is related to esophageal mucosal histopathologic changes such as DIS and TJ alteration. Low baseline values may reflect subtle mucosal abnormalities. Acid reflux clearly decreases impedance baselines, which may be mediated by inflammation that induces characteristic histopathologic changes.
References
Farre R, et al. Evaluation of oesophageal mucosa integrity by the intraluminal impedance technique. Gut. 2011;60(7):885–92.
Kessing BF, et al. Esophageal acid exposure decreases intraluminal baseline impedance levels. Am J Gastroenterol. 2011;106(12):2093–7.
Tobey NA, et al. Dilated intercellular spaces and shunt permeability in nonerosive acid-damaged esophageal epithelium. Am J Gastroenterol. 2004;99(1):13–22.
Farre R, et al. Short exposure of oesophageal mucosa to bile acids, both in acidic and weakly acidic conditions, can impair mucosal integrity and provoke dilated intercellular spaces. Gut. 2008;57(10):1366–74.
Farre R, et al. Acid and weakly acidic solutions impair mucosal integrity of distal exposed and proximal non-exposed human oesophagus. Gut. 2010;59(2):164–9.
Jovov B, et al. Role of E-cadherin in the pathogenesis of gastroesophageal reflux disease. Am J Gastroenterol. 2011;106(6):1039–47.
Lundin P, et al. Bioimpedance spectroscopy: a new tool to assess early esophageal changes linked to gastroesophageal reflux disease? Dis Esophagus. 2011;24(7):462–9.
Orlando LA, Orlando RC. Dilated intercellular spaces as a marker of GERD. Curr Gastroenterol Rep. 2009;11(3):190–4.
van Malenstein H, Farre R, Sifrim D. Esophageal dilated intercellular spaces (DIS) and nonerosive reflux disease. 2008;103(4):1021–28.
Farre R, et al. Critical role of stress in increased oesophageal mucosa permeability and dilated intercellular spaces. Gut. 2007;56(9):1191–7.
Colegio OR, et al. Claudins create charge-selective channels in the paracellular pathway between epithelial cells. Am J Physiol Cell Physiol. 2002;283(1):C142–7.
Chen X, et al. Acidic bile salts modulate the squamous epithelial barrier function by modulating tight junction proteins. Am J Physiol Gastrointest Liver Physiol. 2011;301(2):G203–9.
Oshima T, et al. Acid modulates the squamous epithelial barrier function by modulating the localization of claudins in the superficial layers. Lab Invest. 2011;92(1):22–31.
Asaoka D, et al. Altered localization and expression of tight-junction proteins in a rat model with chronic acid reflux esophagitis. J Gastroenterol. 2005;40(8):781–90.
Oguro M, et al. Dissociation and dispersion of claudin-3 from the tight junction could be one of the most sensitive indicators of reflux esophagitis in a rat model of the disease. J Gastroenterol. 2011;46(5):629–38.
Jones R, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30(10):1030–8.
Vakil N, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900–20 (quiz 1943).
Savarino E, et al. Functional heartburn has more in common with functional dyspepsia than with non-erosive reflux disease. Gut. 2009;58(9):1185–91.
Savarino E, et al. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: study using combined impedance-pH off therapy. Am J Gastroenterol. 2010;105(5):1053–61.
Zerbib F, et al. Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian-French cohort of healthy subjects. Aliment Pharmacol Ther. 2005;22(10):1011–21.
Cui R, et al. The feasibility of light microscopic measurements of intercellular spaces in squamous epithelium in the lower-esophagus of GERD patients. Dis Esophagus. 2011;24(1):1–5.
Ribolsi M, et al. Intercellular space diameters of the oesophageal epithelium in NERD patients: head to head comparison between light and electron microscopy analysis. Dig Liver Dis. 2009;41(1):9–14.
Xavier LL, et al. A simple and fast densitometric method for the analysis of tyrosine hydroxylase immunoreactivity in the substantia nigra pars compacta and in the ventral tegmental area. Brain Res Brain Res Protoc. 2005;16(1–3):58–64.
Wang CJ, et al. Survivin expression quantified by Image Pro-Plus compared with visual assessment. Appl Immunohistochem Mol Morphol. 2009;17(6):530–5.
Richter JE. Role of the gastric refluxate in gastroesophageal reflux disease: acid, weak acid and bile. Am J Med Sci. 2009;338(2):89–95.
Wang K, et al. Diagnostic values of GerdQ, 24-h ambulatory oesophageal pH and impedance-pH monitoring in Barrett’s esophagus, reflux esophagitis and non-erosive reflux disease. Zhonghua Yi Xue Za Zhi. 2011;91(18):1228–32.
Lacy BE, Chehade R, Crowell MD. A prospective study to compare a symptom-based reflux disease questionnaire to 48-h wireless ph monitoring for the identification of gastroesophageal reflux (revised 2-26-11). Am J Gastroenterol. 2011;106(9):1604–11.
Calabrese C, et al. Reversibility of GERD ultrastructural alterations and relief of symptoms after omeprazole treatment. Am J Gastroenterol. 2005;100(3):537–42.
Calabrese C, et al. Effect of omeprazole on symptoms and ultrastructural esophageal damage in acid bile reflux. World J Gastroenterol. 2005;11(12):1876–80.
Xue Y, Zhou LY, Lin SR. Dilated intercellular spaces in gastroesophageal reflux disease patients and the changes of intercellular spaces after omeprazole treatment. Chin Med J (Engl). 2008;121(14):1297–301.
Tobey NA, et al. Physicochemical basis for dilated intercellular spaces in non-erosive acid-damaged rabbit esophageal epithelium. Dis Esophagus. 2008;21(8):757–64.
Orlando RC, et al. Esophageal disease: updated information on inflammation. Ann N Y Acad Sci. 2011;1232:369–75.
Krug SM, Fromm M, Gunzel D. Two-path impedance spectroscopy for measuring paracellular and transcellular epithelial resistance. Biophys J. 2009;97(8):2202–11.
Van Itallie C, Rahner C, Anderson JM. Regulated expression of claudin-4 decreases paracellular conductance through a selective decrease in sodium permeability. J Clin Invest. 2001;107(10):1319–27.
Tamura A, et al. Loss of claudin-15, but not claudin-2, causes Na+ deficiency and glucose malabsorption in mouse small intestine. Gastroenterology. 2011;140(3):913–23.
Harnett KM, et al. Viewpoints on acid-induced inflammatory mediators in esophageal mucosa. J Neurogastroenterol Motil. 2010;16(4):374–88.
Souza RF, et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology. 2009;137(5):1776–84.
Acknowledgments
We thank Professor Michael McNutt for reviewing and editing this manuscript. This study was supported by the Natural Science Funding of Beijing (SZR08-3-03).
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Zhong, C., Duan, L., Wang, K. et al. Esophageal intraluminal baseline impedance is associated with severity of acid reflux and epithelial structural abnormalities in patients with gastroesophageal reflux disease. J Gastroenterol 48, 601–610 (2013). https://doi.org/10.1007/s00535-012-0689-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-012-0689-6