Abstract
Purpose
We investigated associations between treatment decision making (TDM) and global health-related-quality-of-life (gHRQoL) among prostate cancer (PCa) survivors.
Methods
Postal questionnaires were sent to 6559 PCa survivors 2–18 years post-diagnosis, identified through population-based cancer registries in Ireland. The Control Preference Scale was used to investigate respondents’ ‘actual’ and ‘preferred’ role in TDM. The TDM experience was considered ‘congruent’ when actual and preferred roles matched and ‘incongruent’ otherwise. The EORTC QLQ-C30 was used to measure gHRQoL. Multivariate linear regression was employed to investigate associations between (i) actual role in TDM, (ii) congruence in TDM, and gHRQoL.
Results
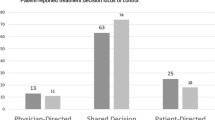
The response rate was 54% (n = 3348). The percentages of men whose actual role in TDM was active, shared or passive were 36, 33 and 31%, respectively. Congruence between actual and preferred roles in TDM was 58%. Actual role in TDM was not associated with gHRQoL. In multivariate analysis, after adjusting for socio-demographic and clinical factors, survivors whose TDM experience was incongruent had significantly lower gHRQoL than those who had a congruent experience (− 2.25 95%CI − 4.09, − 0.42; p = 0.008). This effect was most pronounced among survivors who had more involvement in the TDM than they preferred (− 2.69 95%CI − 4.74, − 0.63; p = 0.010).
Conclusions
Less than 6 in 10 PCa survivors experienced congruence between their actual and preferred roles in TDM. Having an incongruent TDM experience was associated with lower gHRQoL among survivors. These findings suggest that involving patients in TDM to the degree to which they want to be involved may help improve PCa survivors’ gHRQoL.
Similar content being viewed by others
References
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E (2012) Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin 62(4):220–241. https://doi.org/10.3322/caac.21149
Sooriakumaran P, Nyberg T, Akre O, Haendler L, Heus I, Olsson M, Carlsson S, Roobol MJ, Steineck G, Wiklund P (2014) Comparative effectiveness of radical prostatectomy and radiotherapy in prostate cancer: observational study of mortality outcomes. BMJ 348:g1502. https://doi.org/10.1136/bmj.g1502
Bill-Axelson A, Holmberg L, Garmo H, Rider JR, Taari K, Busch C, Nordling S, Häggman M, Andersson SO, Spångberg A, Andrén O, Palmgren J, Steineck G, Adami HO, Johansson JE (2014) Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med 370(10):932–942. https://doi.org/10.1056/NEJMoa1311593
Wilt TJ, Brawer MK, Jones KM, Barry MJ, Aronson WJ, Fox S, Gingrich JR, Wei JT, Gilhooly P, Grob BM, Nsouli I, Iyer P, Cartagena R, Snider G, Roehrborn C, Sharifi R, Blank W, Pandya P, Andriole GL, Culkin D, Wheeler T, Prostate Cancer Intervention versus Observation Trial (PIVOT) Study Group (2012) Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med 367(3):203–213. https://doi.org/10.1056/NEJMoa1113162
Gomella LG, Johannes J, Trabulsi EJ (2009) Current prostate cancer treatments: effect on quality of life. Urology 73(5 Suppl):S28–S35. https://doi.org/10.1016/j.urology.2009.03.003.
Gavin AT, Drummond FJ, Donnelly C, O'Leary E, Sharp L, Kinnear HR (2015) Patient-reported 'ever had' and 'current' long-term physical symptoms after prostate cancer treatments. BJU Int 116(3):397–406. https://doi.org/10.1111/bju.13036
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, for the ProtecT Study Group et al (2016) 10-year outcomes after monitoring, surgery or radiotherapy for localised prostate cancer. NEJM 375(15):1416–1424
Drummond FJ (2016) Are we sleeping on the job? Insomnia among men with prostate cancer. AMOR 2(2):74. 10.18282/amor.v2.i2.94.
Reyna VF, Nelson WL, Han PK, Pignone MP (2015) Decision making and cancer. Am Psychol 70(2):105–118. https://doi.org/10.1037/a0036834
Orom H, Penner LA, West BT, Downs TM, Rayford W, Underwood W (2009) Personality predicts prostate cancer treatment decision-making difficulty and satisfaction. Psycho-Oncology 18(3):290–299. https://doi.org/10.1002/pon.1385
Gwede CK, Pow-Sang J, Seigne J, Heysek R, Helal M, Shade K, Cantor A, Jacobsen PB (2005) Treatment decision-making strategies and influences in patients with localized prostate carcinoma. Cancer 104(7):1381–1390. https://doi.org/10.1002/cncr.21330
Kollmeier MA, Zelefsky MJ (2012) How to select the optimal therapy for early-stage prostate cancer. Crit Rev Oncol Hematol 84(Suppl 1):e6–e15. https://doi.org/10.1016/j.critrevonc.2012.12.002
Keyes M, Crook J, Morton G, Vigneault E, Usmani N, Morris WJ (2013) Treatment options for localized prostate cancer. Can Fam Physician 59(12):1269–1274
Jang TL, Bekelman JE, Liu Y, Bach PB, Basch EM, Elkin EB, Zelefsky MJ, Scardino PT, Begg CB, Schrag D (2010) Physician visits prior to treatment for clinically localized prostate cancer. Arch Intern Med 170(5):440–450. https://doi.org/10.1001/archinternmed.2010.1
Charles C, Gafni A, Whelan T (1997) Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 44(5):681–692. https://doi.org/10.1016/S0277-9536(96)00221-3
Emanuel EJ, Emanuel LL (1992) Four models of the physician-patient relationship. JAMA 267(16):2221–2226. https://doi.org/10.1001/jama.1992.03480160079038
Hubbard G, Kidd L, Donaghy E (2008) Preferences for involvement in treatment decision making of patients with cancer: a review of the literature. Eur J Oncol Nurs 12(4):299–318. https://doi.org/10.1016/j.ejon.2008.03.004
Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, Lakhani I, Salem B, Katz SJ (2005) Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Serv Res 40(3):745–767. https://doi.org/10.1111/j.1475-6773.2005.00383.x
Ashraf AA, Colakoglu S, Nguyen JT, Anastasopulos AJ, Ibrahim AM, Yueh JH, Lin SJ, Tobias AM, Lee BT (2013) Patient involvement in the decision-making process improves satisfaction and quality of life in post-mastectomy breast reconstruction. J Surg Res 184(1):665–670. https://doi.org/10.1016/j.jss.2013.04.057
Wong F, Stewart DE, Dancey J, Meana M, McAndrews MP, Bunston T, Cheung AM (2000) Men with prostate cancer: influence of psychological factors on informational needs and decision making. J Psychosom Res 49(1):13–19. https://doi.org/10.1016/S0022-3999(99)00109-9
Hack TF, Pickles T, Bultz BD, Ruether JD, Degner LF (2007) Impact of providing audiotapes of primary treatment consultations to men with prostate cancer: a multi-site, randomized, controlled trial. Psychooncology 16(6):543–552. https://doi.org/10.1002/pon.1094
Hack TF, Pickles T, Ruether JD, Weir L, Bultz BD, Mackey J, Degner LF (2010) Predictors of distress and quality of life in patients undergoing cancer therapy: impact of treatment type and decisional role. Psychooncology 19(6):606–616. https://doi.org/10.1002/pon.1590
Orom H, Biddle C, Underwood W 3rd, Nelson CJ, Homish DL (2016) What Is a "Good" Treatment Decision? Decisional Control, Knowledge, Treatment Decision Making, and Quality of Life in Men with Clinically Localized Prostate Cancer. Med Decis Mak 36(6):714–725. https://doi.org/10.1177/0272989X16635633
Davison BJ, Degner LF, Morgan TR (1995) Information and decision-making preferences of men with prostate cancer. Oncol Nurs Forum 22(9):1401–1408
Davison BJ, Parker PA, Goldenberg SL (2004) Patients' preferences for communicating a prostate cancer diagnosis and participating in medical decision-making. BJU Int 93(1):47–51. https://doi.org/10.1111/j.1464-410X.2004.04553.x
Davison BJ, Goldenberg SL (2003) Decisional regret and quality of life after participating in medical decision-making for early-stage prostate cancer. BJU Int 91(1):14–17. https://doi.org/10.1046/j.1464-410X.2003.04005.x
Drummond FJ, Kinnear H, Donnelly C, O'Leary E, O'Brien K, Burns RM, Gavin A, Sharp L (2015) Establishing a population-based patient-reported outcomes study (PROMs) using national cancer registries across two jurisdictions: the Prostate Cancer Treatment, your experience (PiCTure) study. BMJ Open 5(4):e006851. https://doi.org/10.1136/bmjopen-2014-006851
WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects. http://www.wma.net/en/30publications/10policies/b3
Degner LF, Sloan JA, Venkatesh P (1997) The Control Preferences Scale. Can J Nurs Res 29(3):21–43
Singh JA, Sloan JA, Atherton PJ, Smith T, Hack TF, Huschka MM, Rummans TA, Clark MM, Diekmann B, Degner LF (2010) Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale. Am J Manag Care 16(9):688–696
Hawley ST, Lantz PM, Janz NK, Salem B, Morrow M, Schwartz K, Liu L, Katz SJ (2007) Factors associated with patient involvement in surgical treatment decision making for breast cancer. Patient Educ Couns 65(3):387–395. https://doi.org/10.1016/j.pec.2006.09.010
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376. https://doi.org/10.1093/jnci/85.5.365
Palmer NRA, Tooze JA, Turner AR, Xu J, Avis NE (2013) African American prostate cancer survivors’ treatment decision-making and quality of life. Patient Educ Couns 90(1):61–68. https://doi.org/10.1016/j.pec.2012.08.007
Folkman S (1997) Positive psychological states and coping with severe stress. Soc Sci Med 45(8):1207–1221. https://doi.org/10.1016/S0277-9536(97)00040-3
Diefenbach MA, Mohamed NE (2007) Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Investig 25(6):449–457. https://doi.org/10.1080/07357900701359460
Burns RM, Sharp L, Sullivan FJ, Deady SE, Drummond FJ, O Neill C (2014) Factors driving inequality in prostate cancer survival: a population based study. PLoS One 9(9):e106456. https://doi.org/10.1371/journal.pone.0106456
Drummond FJ, Kinnear H, O'Leary E, Donnelly GA, Sharp L (2015) Long-term health-related quality of life of prostate cancer survivors varies by primary treatment. Results from the PiCTure (Prostate Cancer Treatment, your experience) study. J Cancer Surviv 9(2):361–372. https://doi.org/10.1007/s11764-014-0419-6
Rimer BK, Briss PA, Zeller PK, Chan EC, Woolf SH (2004) Informed decision making: what is its role in cancer screening? Cancer 101(5 Suppl):1214–1228. https://doi.org/10.1002/cncr.20512
Street RL Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL (2005) Patient participation in medical consultations: why some patients are more involved than others. Med Care 43(10):960–969. https://doi.org/10.1097/01.mlr.0000178172.40344.70
Holmes-Rovner M, Montgomery JS, Rovner DR, Scherer LD, Whitfield J, Kahn VC, Merkle EC, Ubel PA, Fagerlin A (2015) Informed decision making: assessment of the quality of physician communication about prostate cancer diagnosis and treatment. Med Decis Mak 35(8):999–1009. https://doi.org/10.1177/0272989X15597226
Elkin EB, Kim SH, Casper ES, Kissane DW, Schrag D (2007) Desire for information and involvement in treatment decisions: elderly cancer patients' preferences and their physicians' perceptions. J Clin Oncol 25(33):5275–5280. https://doi.org/10.1200/JCO.2007.11.1922
Wilson TD, Gilbert DT (2003) Affective forecasting. Adv Exp Soc Psychol 35:345–411. https://doi.org/10.1016/S0065-2601(03)01006-2
Lin GA, Aaronson DS, Knight SJ, Carroll PR, Dudley RA (2009) Patient decision aids for prostate cancer treatment: a systematic review of the literature. CA Cancer J Clin 59(6):379–390. https://doi.org/10.3322/caac.20039
Adsul P, Wray R, Spradling K, Darwish O, Weaver N, Siddiqui S (2015) Systematic review of decision aids for newly diagnosed patients with prostate cancer making treatment decisions. J Urol 194(5):1247–1252. https://doi.org/10.1016/j.juro.2015.05.093
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L (2017) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 4:CD001431. https://doi.org/10.1002/14651858.CD001431.pub5
Acknowledgements
This work was supported by Health Research Board in the Republic of Ireland (RoI) and by Prostate Cancer UK and Research & Development office of Public health Agency in Northern Ireland. Additional funding was provided by the National Cancer Control Programme (RoI). The authors would like to thank the healthcare professionals who helped to screen the men for eligibility and those who cooperated in obtaining ethical approval. We would like to thank the Men Against Cancer support group, all those who commented on the survey during development and those who pre-tested it. Finally, we would like to thank the men who completed the survey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Supplementary Table 1
(ODT 17.2 kb)
Rights and permissions
About this article
Cite this article
Drummond, F.J., Gavin, A.T. & Sharp, L. Incongruence in treatment decision making is associated with lower health-related quality of life among prostate cancer survivors: results from the PiCTure study. Support Care Cancer 26, 1645–1654 (2018). https://doi.org/10.1007/s00520-017-3994-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3994-z