Abstract
Purpose
A significant minority of colorectal cancer (CRC) patients experience clinically meaningful distress that may warrant intervention. The goal of this systematic review was to assess the impact of psychosocial interventions on quality-of-life and psychosocial outcomes for CRC patients.
Methods
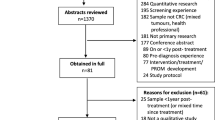
A systematic search of CINAHL, MEDLINE, PsycINFO, and PsycARTICLES was undertaken to obtain relevant randomized controlled trials (RCTs) published through October 2016.
Results
Fourteen RCTs of psychosocial interventions for CRC patients were identified. Only three of these RCTs showed significant intervention effects on multiple mental health outcomes. These interventions included written and verbal emotional expression, progressive muscle relaxation training, and a self-efficacy enhancing intervention. Eight of the 14 trials, testing a range of psychoeducational and supportive care interventions, produced little to no effects on study outcomes. An evaluation of RCT quality highlighted the need for greater rigor in study methods and reporting.
Conclusion
A limited evidence base supports the efficacy of psychosocial interventions for CRC patients. Large-scale trials are needed before drawing definitive conclusions regarding intervention impact.

Similar content being viewed by others
References
Dunn J, Ng SK, Holland J, Aitken J, Youl P, Baade PD, Chambers SK (2013) Trajectories of psychological distress after colorectal cancer. Psychooncology 22:1759–1765
Hou WK, Law CC, Yin J, Fu YT (2010) Resource loss, resource gain, and psychological resilience and dysfunction following cancer diagnosis: a growth mixture modeling approach. Health Psychol 29:484–495
Mosher CE, Winger JG, Given BA, Helft PR, O’Neil BH (2016) Mental health outcomes during colorectal cancer survivorship: a review of the literature. Psychooncology 25:1261–1270
Chambers SK, Meng X, Youl P, Aitken J, Dunn J, Baade P (2012) A five-year prospective study of quality of life after colorectal cancer. Qual Life Res 21:1551–1564
Arndt V, Merx H, Stegmaier C, Ziegler H, Brenner H (2004) Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: a population-based study. J Clin Oncol 22:4829–4836
Hou WK, Law CC, Fu YT (2010) Does change in positive affect mediate and/or moderate the impact of symptom distress on psychological adjustment after cancer diagnosis? A prospective analysis. Psychol Health 25:417–431
Hou WK, Wan JH (2012) Perceived control mediates the prospective impact of relationship quality in the year after colorectal cancer diagnosis. Ann Behav Med 43:129–138
Simon AE, Thompson MR, Flashman K, Wardle J (2009) Disease stage and psychosocial outcomes in colorectal cancer. Color Dis 11:19–25
Smith-Gagen J, Cress RD, Drake CM, Romano PS, Yost KJ, Ayanian JZ (2010) Quality-of-life and surgical treatments for rectal cancer—a longitudinal analysis using the California Cancer Registry. Psychooncology 19:870–878
Steginga SK, Lynch BM, Hawkes A, Dunn J, Aitken J (2009) Antecedents of domain-specific quality of life after colorectal cancer. Psychooncology 18:216–220
Sharma A, Sharp DM, Walker LG, Monson JR (2007) Predictors of early postoperative quality of life after elective resection for colorectal cancer. Ann Surg Oncol 14:3435–3442
Lynch BM, Steginga SK, Hawkes AL, Pakenham KI, Dunn J (2008) Describing and predicting psychological distress after colorectal cancer. Cancer 112:1363–1370
Emmertsen KJ, Laurberg S (2013) Impact of bowel dysfunction on quality of life after sphincter-preserving resection for rectal cancer. Br J Surg 100:1377–1387
Occhipinti S, Chambers SK, Lepore S, Aitken J, Dunn J (2015) A longitudinal study of post-traumatic growth and psychological distress in colorectal cancer survivors. PLoS One 10:e0139119
Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R (2013) Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol 31:782–793
Hart SL, Hoyt MA, Diefenbach M, Anderson DR, Kilbourn KM, Craft LL, Steel JL, Cuijpers P, Mohr DC, Berendsen M, Spring B, Stanton AL (2012) Meta-analysis of efficacy of interventions for elevated depressive symptoms in adults diagnosed with cancer. J Natl Cancer Inst 104:990–1004
Schneider S, Moyer A, Knapp-Oliver S, Sohl S, Cannella D, Targhetta V (2010) Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Behav Med 33:1–14
American Cancer Society (2017) Cancer facts and figures 2017. American Cancer Society, Atlanta
Rozmovits L, Ziebland S (2004) Expressions of loss of adulthood in the narratives of people with colorectal cancer. Qual Health Res 14:187–203
Traa MJ, De Vries J, Roukema JA, Den Oudsten BL (2011) Sexual (dys)function and the quality of sexual life in patients with colorectal cancer: a systematic review. Ann Oncol 23:19–27
Hoon LS, Chi Sally CW, Hong-Gu H (2013) Effect of psychosocial interventions on outcomes of patients with colorectal cancer: a review of the literature. Eur J Oncol Nurs 17:883–891
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Cramer H, Lauche R, Klose P, Dobos G, Langhorst J (2014) A systematic review and meta-analysis of exercise interventions for colorectal cancer patients. Eur J Cancer Care (Engl) 23:3–14
Kassianos AP, Raats MM, Gage H, Peacock M (2015) Quality of life and dietary changes among cancer patients: a systematic review. Qual Life Res 24:705–719
Hawkes AL, Chambers SK, Pakenham KI, Patrao TA, Baade PD, Lynch BM, Aitken JF, Meng X, Courneya KS (2013) Effects of a telephone-delivered multiple health behavior change intervention (CanChange) on health and behavioral outcomes in survivors of colorectal cancer: a randomized controlled trial. J Clin Oncol 31:2313–2321
Demark-Wahnefried W, Morey MC, Sloane R, Snyder DC, Miller PE, Hartman TJ, Cohen HJ (2012) Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. J Clin Oncol 30:2354–2361
Hawkes AL, Pakenham KI, Chambers SK, Patrao TA, Courneya KS (2014) Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: a randomized controlled trial. Ann Behav Med 48:359–370
Winger JG, Mosher CE, Rand KL, Morey MC, Snyder DC, Demark-Wahnefried W (2014) Diet and exercise intervention adherence and health-related outcomes among older long-term breast, prostate, and colorectal cancer survivors. Ann Behav Med 48:235–245
Centre for Evidence-Based Physiotherapy (2009) PEDro scale. Centre for Evidence-Based Physiotherapy. http://www.pedro.org.au/. Accessed 2 Nov 2016
Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, Ogedegbe G, Orwig D, Ernst D, Czajkowski S (2004) Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 23:443–451
Newell SA, Sanson-Fisher RW, Savolainen NJ (2002) Systematic review of psychological therapies for cancer patients: overview and recommendations for future research. J Natl Cancer Inst 94:558–584
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) When does it make sense to perform a meta-analysis? In: Introduction to meta-analysis. Wiley, Chichester, UK, p 357–364
Beaver K, Campbell M, Williamson S, Procter D, Sheridan J, Heath J, Susnerwala S (2012) An exploratory randomized controlled trial comparing telephone and hospital follow-up after treatment for colorectal cancer. Colorectal Dis 14:1201–1209
Carmack CL, Basen-Engquist K, Yuan Y, Greisinger A, Rodriguez-Bigas M, Wolff RA, Barker T, Baum G, Pennebaker JW (2011) Feasibility of an expressive-disclosure group intervention for post-treatment colorectal cancer patients: results of the Healthy Expressions study. Cancer 117:4993–5002
Cheung YL, Molassiotis A, Chang AM (2003) The effect of progressive muscle relaxation training on anxiety and quality of life after stoma surgery in colorectal cancer patients. Psychooncology 12:254–266
Edgar L, Rosberger Z, Collet JP (2001) Lessons learned: outcomes and methodology of a coping skills intervention trial comparing individual and group formats for patients with cancer. Int J Psychiatry Med 31:289–304
Haase O, Schwenk W, Hermann C, Muller JM (2005) Guided imagery and relaxation in conventional colorectal resections: a randomized, controlled, partially blinded trial. Dis Colon Rectum 48:1955–1963
Harrison JD, Young JM, Solomon MJ, Butow PN, Secomb R, Masya L (2011) Randomized pilot evaluation of the supportive care intervention “CONNECT” for people following surgery for colorectal cancer. Dis Colon Rectum 54:622–631
Hendren S, Griggs JJ, Epstein R, Humiston S, Jean-Pierre P, Winters P, Sanders M, Loader S, Fiscella K (2012) Randomized controlled trial of patient navigation for newly diagnosed cancer patients: effects on quality of life. Cancer Epidemiol Biomark Prev 21:1682–1690
Lee AM, Ho JW, Chan CL (2010) Efficacy of psychosocial intervention in improving quality of life and psychological well-being of Chinese patients with colorectal cancer: a randomised controlled trial. Hong Kong Med J 16:20–24
O’Connor G, Coates V, O’Neill S (2014) Randomised controlled trial of a tailored information pack for patients undergoing surgery and treatment for rectal cancer. Eur J Oncol Nurs 18:183–191
Reese JB, Porter LS, Regan KR, Keefe FJ, Azad NS, Diaz LA, Herman JM, Haythornthwaite JA (2014) A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psychooncology 23:1005–1013
Ross L, Thomsen BL, Karlsen RV, Boesen EH, Johansen C (2005) A randomized psychosocial intervention study on the effect of home visits on the well-being of Danish colorectal cancer patients—the INCA Project. Psychooncology 14:949–961
White VM, Macvean ML, Grogan S, D’Este C, Akkerman D, Ieropoli S, Hill DJ, Sanson-Fisher R (2012) Can a tailored telephone intervention delivered by volunteers reduce the supportive care needs, anxiety and depression of people with colorectal cancer? A randomised controlled trial. Psychooncology 21:1053–1062
Young JM, Butow PN, Walsh J, Durcinoska I, Dobbins TA, Rodwell L, Harrison JD, White K, Gilmore A, Hodge B, Hicks H, Smith S, O’Connor G, Byrne CM, Meagher AP, Jancewicz S, Sutherland A, Ctercteko G, Pathma-Nathan N, Curtin A, Townend D, Abraham NS, Longfield G, Rangiah D, Young CJ, Eyers A, Lee P, Fisher D, Solomon MJ (2013) Multicenter randomized trial of centralized nurse-led telephone-based care coordination to improve outcomes after surgical resection for colorectal cancer: the CONNECT intervention. J Clin Oncol 31:3585–3591
Zhang M, Chan SW, You L, Wen Y, Peng L, Liu W, Zheng M (2014) The effectiveness of a self-efficacy-enhancing intervention for Chinese patients with colorectal cancer: a randomized controlled trial with 6-month follow up. Int J Nurs Stud 51:1083–1092
Adams RN, Mosher CE, Blair CK, Snyder DC, Sloane R, Demark-Wahnefried W (2015) Cancer survivors’ uptake and adherence in diet and exercise intervention trials: an integrative data analysis. Cancer 121:77–83
Hann KEJ, McCracken LM (2014) A systematic review of randomized controlled trials of acceptance and commitment therapy for adults with chronic pain: outcome domains, design quality, and efficacy. J Contextual Behav Sci 3:217–227
Hayes SC, Villatte M, Levin M, Hildebrandt M (2011) Open, aware, and active: contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annu Rev Clin Psychol 7:141–168
Stanton AL, Luecken LJ, MacKinnon DP, Thompson EH (2013) Mechanisms in psychosocial interventions for adults living with cancer: opportunity for integration of theory, research, and practice. J Consult Clin Psychol 81:318–335
Phelan SM, Griffin JM, Jackson GL, Zafar SY, Hellerstedt W, Stahre M, Nelson D, Zullig LL, Burgess DJ, van Ryn M (2013) Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psychooncology 22:65–73
Grumann MM, Noack EM, Hoffmann IA, Schlag PM (2001) Comparison of quality of life in patients undergoing abdominoperineal extirpation or anterior resection for rectal cancer. Ann Surg 233:149–156
Earle CC, Chretien Y, Morris C, Ayanian JZ, Keating NL, Polgreen LA, Wallace R, Ganz PA, Weeks JC (2010) Employment among survivors of lung cancer and colorectal cancer. J Clin Oncol 28:1700–1705
Chambers, SK, Morris, BA, Clutton, S, Foley, E, Giles, L, Schofield, P, O’Connell, D, Dunn, J (2015) Psychological wellness and health-related stigma: a pilot study of an acceptance-focused cognitive behavioural intervention for people with lung cancer. Eur J Cancer Care 24:60–70
Brotto LA, Yule M, Breckon E (2010) Psychological interventions for the sexual sequelae of cancer: a review of the literature. J Cancer Surviv 4:346–360
McCorkle R, Ercolano E, Lazenby M, Schulman-Green D, Schilling LS, Lorig K, Wagner EH (2011) Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin 61:50–62
Acknowledgements
Catherine Mosher’s work was supported by the National Cancer Institute [grant numbers: K07CA168883 and K05CA175048]. Its content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Mosher, C.E., Winger, J.G., Given, B.A. et al. A systematic review of psychosocial interventions for colorectal cancer patients. Support Care Cancer 25, 2349–2362 (2017). https://doi.org/10.1007/s00520-017-3693-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3693-9