Abstract
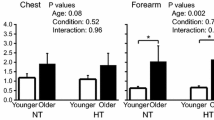
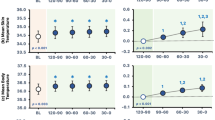
Thermal sensation represents the primary stimulus for behavioral and autonomic thermoregulation. We assessed whether the sensation of skin and core temperatures for the driving force of behavioral thermoregulation was modified by postural change from the supine (Sup) to sitting (Sit) during mild hyperthermia. Seventeen healthy young men underwent measurements of noticeable increase and decrease (±0.1 °C/s) of skin temperature (thresholds of warm and cold sensation on the skin, 6.25 cm2 of area) at the forearm and chest and of the whole-body warm sensation in the Sup and Sit during normothermia (NT; esophageal temperature (Tes), ∼36.6 °C) and mild hyperthermia (HT; Tes, ∼37.2 °C; lower legs immersion in 42 °C of water). The threshold for cold sensation on the skin at chest was lower during HT than NT in the Sit (P < 0.05) but not in Sup, and at the forearm was lower during HT than NT in the Sup and further in Sit (both, P < 0.05), with interactive effects of temperature (NT vs. HT) × posture (Sup vs. Sit) (chest, P = 0.08; forearm, P < 0.05). The threshold for warm sensation on the skin at both sites remained unchanged with changes in body posture or temperature. The whole-body warm sensation was higher during HT than NT in both postures and higher in the Sit than Sup during both NT and HT (all, P < 0.05). Thus, thermal sensation during mild hyperthermia is modulated by postural change from supine to sitting to sense lesser cold on the skin and more whole-body warmth.



Similar content being viewed by others
References
Attia M, Engel P, Hildebrandt G (1980) Quantification of thermal comfort parameters using a behavioural indicator. Physiol Behav 24(5):901–909
Badoer E, McKinlay D, Trigg L, McGrath BP (1997) Distribution of activated neurons in the rabbit brain following a volume load. Neuroscience 81(4):1065–1077
Bartlett G, Stewart JD, Tamblyn R, Abrahamowicz M (1998) Normal distributions of thermal and vibration sensory thresholds. Muscle Nerve 21(3):367–374
Campero M, Serra J, Bostock H, Ochoa JL (2001) Slowly conducting afferents activated by innocuous low temperature in human skin. J Physiol 535(Pt 3):855–865
Craig AD, Bushnell MC, Zhang ET, Blomqvist A (1994) A thalamic nucleus specific for pain and temperature sensation. Nature 372(6508):770–773. doi:10.1038/372770a0
Egan GF, Johnson J, Farrell M, McAllen R, Zamarripa F, McKinley MJ, Lancaster J, Denton D, Fox PT (2005) Cortical, thalamic, and hypothalamic responses to cooling and warming the skin in awake humans: a positron-emission tomography study. Proc Natl Acad Sci U S A 102(14):5262–5267. doi:10.1073/pnas.0409753102
Frank SM, Raja SN, Bulcao CF, Goldstein DS (1999) Relative contribution of core and cutaneous temperatures to thermal comfort and autonomic responses in humans. J Appl Physiol 86(5):1588–1593
Gagge AP, Stolwijk JA, Hardy JD (1967) Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res 1(1):1–20
Gagge AP, Stolwijk JA, Saltin B (1969) Comfort and thermal sensations and associated physiological responses during exercise at various ambient temperatures. Environ Res 2(3):209–229
Gelber DA, Pfeifer MA, Broadstone VL, Munster EW, Peterson M, Arezzo JC, Shamoon H, Zeidler A, Clements R, Greene DA, Porte D, Laudadioj C, Brilk V (1995) Components of variance for vibratory and thermal threshold testing in normal and diabetic subjects. J Diabetes Complicat 9(3):170–176
Gerrett N, Ouzzahra Y, Redortier B, Voelcker T, Havenith G (2015) Female thermal sensitivity to hot and cold during rest and exercise. Physiol Behav 152(Pt A):11–19. doi:10.1016/j.physbeh.2015.08.032
Guergova S, Dufour A (2011) Thermal sensitivity in the elderly: a review. Ageing Res Rev 10(1):80–92. doi:10.1016/j.arr.2010.04.009
Hagander LG, Midani HA, Kuskowski MA, Parry GJ (2000) Quantitative sensory testing: effect of site and skin temperature on thermal thresholds. Clin Neurophysiol 111(1):17–22
Hall JF Jr, Klemm FK (1969) Thermal comfort in disparate thermal environments. J Appl Physiol 27(5):601–606
Hilz MJ, Stemper B, Axelrod FB, Kolodny EH, Neundörfer B (1999) Quantitative thermal perception testing in adults. J Clin Neurophysiol 16(5):462–471
Horowitz M, Meiri U (1985) Thermoregulatory activity in the rat: effects of hypohydration, hypovolemia and hypertonicity and their interaction with short-term heat acclimation. Comparative biochemistry and physiology A, Comparative physiology 82(3):577–582
Inoue S, Murakami N (1976) Unit responses in the medulla oblongata of rabbit to changes in local and cutaneous temperature. J Physiol 259(2):339–356
Johnson JM, Rowell LB, Brengelmann GL (1974) Modification of the skin blood flow-body temperature relationship by upright exercise. J Appl Physiol 37(6):880–886
Kawano T, Kabasawa Y, Ashikawa S, Sato Y, Jinno S, Omura K (2009) Accuracy and reliability of thermal threshold measurement in the chin using heat flux technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108(4):500–504. doi:10.1016/j.tripleo.2009.05.034
Koltyn KF (2000) Analgesia following exercise: a review. Sports Med 29(2):85–98
Kubota K, Kurabayashi H, Tamura K, Kawada E, Tamura J, Shirakura T (1992) A transient rise in plasma beta-endorphin after a traditional 47 degrees C hot-spring bath in Kusatsu-spa, Japan. Life Sci 51(24):1877–1880
Lin CH, Tokizawa K, Nakamura M, Uchida Y, Mori H, Nagashima K (2012) Hyperosmolality in the plasma modulates behavioral thermoregulation in mice: the quantitative and multilateral assessment using a new experimental system. Physiol Behav 105(2):536–543. doi:10.1016/j.physbeh.2011.09.006
Morrison SF, Nakamura K (2011) Central neural pathways for thermoregulation. Front Biosci (Landmark Ed) 16:74–104
Mower GD (1976) Perceived intensity of peripheral thermal stimuli is independent of internal body temperature. J Comp Physiol Psychol 90(12):1152–1155
Nagashima K (2006) Central mechanisms for thermoregulation in a hot environment. Ind Health 44(3):359–367
Nagashima K, Nakai S, Konishi M, Su L, Kanosue K (2001) Increased heat-escape/cold-seeking behavior following hypertonic saline injection in rats. Am J Physiol Regul Integr Comp Physiol 280(4):R1031–R1036
Nagashima K, Nose H, Takamata A, Morimoto T (1998) Effect of continuous negative-pressure breathing on skin blood flow during exercise in a hot environment. J Appl Physiol 84(6):1845–1851
Nakajima Y, Nose H, Takamata A (1998) Plasma hyperosmolality and arterial pressure regulation during heating in dehydrated and awake rats. Am J Phys 275(5 Pt 2):R1703–R1711
Nakamura K, Morrison SF (2010) A thermosensory pathway mediating heat-defense responses. Proc Natl Acad Sci U S A 107(19):8848–8853. doi:10.1073/pnas.0913358107
Nose H, Mack GW, Shi XR, Morimoto K, Nadel ER (1990) Effect of saline infusion during exercise on thermal and circulatory regulations. J Appl Physiol 69(2):609–616
Okazaki K, Hayase H, Ichinose T, Mitono H, Doi T, Nose H (2009) Protein and carbohydrate supplementation after exercise increases plasma volume and albumin content in older and young men. J Appl Physiol 107(3):770–779. doi:10.1152/japplphysiol.91264.2008
Palmer ST, Martin DJ, Steedman WM, Ravey J (2000) C- and Adelta-fibre mediated thermal perception: response to rate of temperature change using method of limits. Somatosens Mot Res 17(4):325–333
Ramanathan NL (1964) A new weighting system for mean surface temperature of the human body. J Appl Physiol 19:531–533
Rowell LB (1993) Reflex control during orthostasis. In: Rowell LB (ed) Human cardiovascular control. Oxford Univesity Press, New york, pp. 37–80
Shafton AD, Ryan A, McGrath B, Badoer E (1999) Volume expansion does not activate neuronal projections from the NTS or depressor VLM to the RVLM. Am J Phys 277(1 Pt 2):R39–R46
Simon E, Pierau FK, Taylor DC (1986) Central and peripheral thermal control of effectors in homeothermic temperature regulation. Physiol Rev 66(2):235–300
Sosenko JM, Kato M, Soto R, Ayyar DR (1989) Determinants of quantitative sensory testing in non-neuropathic individuals. Electromyogr Clin Neurophysiol 29(7–8):459–463
Stevens JC, Choo KK (1998) Temperature sensitivity of the body surface over the life span. Somatosens Mot Res 15(1):13–28
Strigo IA, Carli F, Bushnell MC (2000) Effect of ambient temperature on human pain and temperature perception. Anesthesiology 92(3):699–707
Tochihara Y, Kumamoto T, Lee JY, Hashiguchi N (2011) Age-related differences in cutaneous warm thresholds of human males in thermoneutral and cool environments. J Therm Biol 36:105–111
Tokizawa K, Yasuhara S, Nakamura M, Uchida Y, Crawshaw LI, Nagashima K (2010) Mild hypohydration induced by exercise in the heat attenuates autonomic thermoregulatory responses to the heat, but not thermal pleasantness in humans. Physiol Behav 100(4):340–345. doi:10.1016/j.physbeh.2010.03.008
Werner J, Mekjavic IB, Taylor NAS (2008) Concepts in physiological regulation: a thermoregulatory perspective. In: Taylor NAS, Groeller H (eds) Physiological bases of human performance during work and exercise. Elsevier, Philadelphia, pp. 325–340
Yamazaki F, Nakayama Y, Sone R (2006) Whole-body heating decreases skin vascular response to low orthostatic stress in the lower extremities. J Physiol Sci 56(2):157–164. doi:10.2170/physiolsci.RP000406
Acknowledgments
We are very grateful to the volunteers who participated in this study. We also thank Dr. Takaaki Okumoto from our laboratory, and Dr. Shinya Matsumura from the department of Sport Science and Medical Science, Osaka University of Health and Sport Science, for useful comments and suggestions regarding this manuscript.
Author contributions
R.T. contributed to the design of the experiment, data collection, assembly, analysis and interpretation, and drafted the article; D.I., A.S., A.O., N.N., Y.Y., and Y.H. contributed to data collection, analysis and interpretation, and revised the article; H.Y. and T.M. contributed to data interpretation and revised the article; K.O. contributed to the conception, the design of the experiment, data interpretation, and revised the article critically for important intellectual content. All authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study procedure was approved by the Institutional Review Board of Osaka City University Graduate School of Medicine and conformed to the standards set by the Declaration of Helsinki.
ᅟ
Conflict of Interest
The authors declare that they have no conflict of interest.
Source of funding
This study was supported in part by a Grant-in-Aid for Young Scientists A 23689014 and Challenging Exploratory Research 25560372 (to K. Okazaki) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Electronic Supplementary Material
ESM 1
(DOCX 99 kb)
Rights and permissions
About this article
Cite this article
Takeda, R., Imai, D., Suzuki, A. et al. Thermal sensation during mild hyperthermia is modulated by acute postural change in humans. Int J Biometeorol 60, 1925–1932 (2016). https://doi.org/10.1007/s00484-016-1179-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-016-1179-y