Abstract
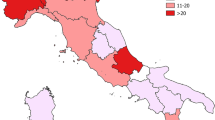
Evidence of the impact of air temperature and pressure on cardiovascular morbidity is still quite limited and controversial, and even less is known about the potential influence of geomagnetic activity. The objective of this study was to assess impacts of air temperature, barometric pressure and geomagnetic activity on hospitalizations with myocardial infarctions and brain strokes. We studied 2,833 myocardial infarctions and 1,096 brain strokes registered in two Moscow hospitals between 1992 and 2005. Daily event rates were linked with meteorological and geomagnetic conditions, using generalized linear model with controls for day of the week, seasonal and long-term trends. The number of myocardial infarctions decreased with temperature, displayed a U-shaped relationship with pressure and variations in pressure, and increased with geomagnetic activity. The number of strokes increased with temperature, daily temperature range and geomagnetic activity. Detrimental effects on strokes of low pressure and falling pressure were observed. Relative risks of infarctions and strokes during geomagnetic storms were 1.29 (95 % CI 1.19–1.40) and 1.25 (1.10–1.42), respectively. The number of strokes doubled during cold spells. The influence of barometric pressure on hospitalizations was relatively greater than the influence of geomagnetic activity, and the influence of temperature was greater than the influence of pressure. Brain strokes were more sensitive to inclement weather than myocardial infarctions. This paper provides quantitative estimates of the expected increases in hospital admissions on the worst days and can help to develop preventive health plans for cardiovascular diseases.


Similar content being viewed by others
References
Abe T, Ohde S, Ishimatsu S, Ogata H, Hasegawa T, Nakamura T, Tokuda Y (2008) Effects of meteorological factors on the onset of subarachnoid hemorrhage: a time-series analysis. J Clin Neurosci 15(9):1005–1010. doi:10.1016/j.jocn.2007.07.081
Abrignani MG, Corrao S, Biondo GB, Renda N, Braschi A, Novo G, Di Girolamo A, Braschi GB, Novo S (2009) Influence of climatic variables on acute myocardial infarction hospital admissions. Int J Cardiol 137(2):123–129. doi:10.1016/j.ijcard.2008.06.036
Berthelier A, Menvielle M (1993) Computation of AK equivalent amplitude. Int Assoc Geomagn Aeron News 32:23–25
Bhaskaran K, Hajat S, Haines A, Herrett E, Wilkinson P, Smeeth L (2009) Effects of ambient temperature on the incidence of myocardial infarction. Heart 95:1760–1769. doi:10.1136/hrt.2009.175000
Brezinski DA, Tofler GH, Muller JE, Pohjola-Sintonen S, Willich SN, Schafer AI, Czeisler CA, Williams GH (1988) Morning increase in platelet aggregability. Association with assumption of the upright posture. Circulation 78:35–40
Chang CL, Shipley M, Marmot M, Poulter N (2004) Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J Clin Epidemiol 57:749–757. doi:10.1016/j.jclinepi.2003.10.016
Coelho FM, Santos BF, Cendoroglo Neto M, Lisboa LF, Cypriano AS, Lopes TO, Miranda MJ, Avila AM, Alonso JB, Pinto HS (2010) Temperature variation in the 24 hours before the initial symptoms of stroke. Arq Neuropsiquiatr 68(2):242–245. doi:10.1590/S0004-282X2010000200017
Cornelissen G, Halberg F, Breus TK, Syutkina EV, Baevsky R, Weydahl A et al (2002) Non-photic solar associations of heart rate variability and myocardial infarction. J Atmos Solar Terr Phys 64:707–772. doi:10.1016/S1364-6826(02)00032-9
Dawson J, Weir C, Wright F, Bryden C, Aslanyan S, Lees K, Bird W, Walters M (2008) Associations between meteorological variables and acute stroke hospital admissions in the west of Scotland. Acta Neurol Scand 117(2):85–89. doi:10.1111/j.1600-0404.2007.00916.x
Delyukov A, Gorgo Y, Cornelissen G, Otsuka K, Halberg F (2001) Natural environmental associations in a 50-day human electrocardiogram. Int J Biometeorol 45(2):90–99. doi:10.1007/s004840100086
Dormann C, Elith J, Bacher S, Buchmann C, Carl G, Carré G et al (2012) Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. doi:10.1111/j.1600-0587.2012.07348.x
Fedin AI, Rumiantseva SA, Kuznetsov OR, Evseev VN (2004) Antloxidant and actoprotector therapy of ischemic stroke. Tactic-Studio, Moscow (in Russian)
Feigin VL, Nikitin YP, Bots ML, Vinogradova TE, Grobbee DE (2000) A population-based study of the associations of stroke occurrence with weather parameters in Siberia, Russia (1982–1992). Eur J Neurol 7:171–178
Ghione S, Mezzasalma L, Del Seppia C, Papi F (1998) Do geomagnetic disturbances of solar origin affect arterial blood pressure? J Hum Hypertens 12:749–754
Giua A, Abbas M, Murgia N, Corea F (2010) Climate and stroke: a controversial association. Int J Biometeorol 54:1–3. doi:10.1007/s00484-009-0253-0
Gmitrov J, Gmitrova A (2004) Geomagnetic field effect on cardiovascular regulation. Bioelectromagnetics 25:92–101. doi:10.1002/bem.10173
Gmitrov J, Ohkubo C (1999) Geomagnetic field decreases cardiovascular variability. Electro-Magnetobiol 18:291–303. doi:10.3109/15368379909022585
Goldberg MS, Giannetti N, Burnett RT, Mayo NE, Valois MF, Brophy JM (2008) A panel study in congestive heart failure to estimate the short-term effects from personal factors and environmental conditions on oxygen saturation and pulse rate. Occup Environ Med 65:659–666. doi:10.1136/oem.2007.034934
Gurfinkel YI, Voeikov VL (2006) Solar activity effects on blood of patients with coronary heart disease. In: Atkov OY, Gurfinkel YI (eds) Proceedings of International Scientific Workshop «Space weather effects on biological systems and human health». Reprocenter, Moscow, pp 101–103 (in Russian)
Gurfinkel YI, Liubimov VV, Oraevski VN, Parfenova LM, Yuriev AS (1995) The effect of geomagnetic disturbances on capillary blood flow in ischemic heart disease patients. Biofizika 40(4):793–799 (in Russian)
Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H (2003) Ischemic stroke associated with decrease in temperature. Epidemiology 14:473–478. doi:10.1097/01.ede.0000078420.82023.e3
Hori A, Hashizume M, Tsuda Y, Tsukahara T, Nomiyama T (2012) Effects of weather variability and air pollutants on emergency admissions for cardiovascular and cerebrovascular diseases. Int J Environ Health Res 22(5):416–430. doi:10.1080/09603123.2011.650155
Houck PD, Lethen JE, Riggs MW, Gantt DS, Denmer GJ (2005) Relation of atmospheric pressure changes and the occurrences of acute myocardial infarction and stroke. Am J Cardiol 96:45–51. doi:10.1080/09603123.2011.650155
Interfax (2012) Press release of 16.05.12. http://www.interfax-russia.ru/Moscow/report.asp?id=315045. Accessed February 20 2013 (in Russian)
ISIS-2 (Second International Study of Infarct Survival) Collaborative Group (1992) Morning peak in the incidence of myocardial infarction: experience in the ISIS-2 trial. Eur Heart J 13(5):594–598
Jimenez-Conde J, Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Subirana I, Roquer J (2008) Weather as a trigger of stroke. Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis 26(4):348–354. doi:10.1159/000151637
Kavanagh A, Denton M (2007) High-speed solar-wind streams and geospace interactions. Astron Geophys 48:6.24–6.26. doi:10.1111/j.1468-4004.2007.48624.x
Kloner RA (2006) Natural and unnatural triggers of myocardial infarction. Prog Cardiovasc Dis 48(4):285–300. doi:10.1016/j.pcad.2005.07.001
Koton S (2003) Triggering risk factors for ischemic stroke. Dissertation, Tel Aviv University. http://primage.tau.ac.il/libraries/theses/lifemed/free/1925818.pdf. Accessed 20 February 2013
Kyobutungi C, Grau A, Stieglbauer G, Becher H (2005) Absolute temperature, temperature changes and stroke risk: a case-crossover study. Eur J Epidemiol 20:693–698. doi:10.1007/s10654-005-0703-x
Landers AT, Narotam PK, Govender ST, van Dellen JR (1997) The effect of changes in barometric pressure on the risk of rupture of intracranial aneurysms. Br J Neurosurg 11(3):191–195. doi:10.1080/02688699746230
Lee JH, Chae SC, Yang DH, Park HS, Cho Y, Jun JE, Park WH, Kam S, Lee WK, Kim YJ, Kim KS, Hur SH, Jeong MH, Korea Acute Myocardial Infarction Registry Investigators (2010) Influence of weather on daily hospital admissions for acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry). Int J Cardiol 144(1):16–21. doi:10.1016/j.ijcard.2009.03.122
Liemohn MW, Jazowski M, Kozyra JU, Ganushkina N, Thomsen MF (2010) CIR versus CME drivers of the ring current during intense magnetic storms. Proc R Soc A 466:3305–3328. doi:10.1098/rspa.2010.0075
Lim YH, Kim H (2011) Diurnal temperature range and cause-specific cardiovascular hospital admission in Seoul, Korea – time-series analysis and temperature-matched case-crossover design. Epidemiology 22(1):S13–S14. doi:10.1097/01.ede.0000391696.12070.b1
Linares С, Diaz J (2008) Impact of high temperatures on hospital admissions: comparative analysis with previous studies about mortality (Madrid). Eur J Public Health 18:317–322. doi:10.1093/eurpub/ckm108
Magalhães R, Silva MC, Correia M, Bailey T (2011) Are stroke occurrence and outcome related to weather parameters? Results from a population-based study in northern Portugal. Cerebrovasc Dis 32(6):542–551. doi:10.1159/000331473
McArthur K, Dawson J, Walters M (2010) What is it with the weather and stroke? Expert Rev Neurother 10(2):243–249. doi:10.1586/ern.09.154
Meehl GA, Tebaldi C (2004) More intense, more frequent, and longer lasting heat waves in the 21st century. Science 305:994–997. doi:10.1126/science.1098704
Menvielle M, Berthelier A (1991) The K-derived planetary indices: description and availability. Rev Geophys 29:415–432. doi:10.1029/91RG00994
Messner T, Lundberg V, Wikstrom B (2002) A temperature rise is associated with an increase in the number of acute myocardial infarctions in the subarctic area. Int J Circumpolar Health 61:201–207
Morabito M, Crisci A, Orlandini S, Maracchi G, Gensini GF, Modesti PA (2008) A synoptic approach to weather conditions discloses a relationship with ambulatory blood pressure in hypertensives. Am J Hypertens 21:748–752. doi:10.1038/ajh.2008.177
Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S (2011) Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke 42:593–600. doi:10.1161/STROKEAHA.110.602037
NOAA (US National Oceanic and Atmospheric Administration) (2005) Space weather scales. http://www.swpc.noaa.gov/NOAAscales/. Accessed 20 February 2013
Oinuma S, Kubo Y, Otsuka K, Yamanaka T, Murakami S, Matsuoka O et al (2002) Graded response of heart rate variability, associated with an alteration of geomagnetic activity in a subarctic area. Biomed Pharmacother 56:284s–288s
Otsuka K, Oinuma S, Cornelissen G, Weydahl A, Ichimary Y, Kobayashi M et al (2001a) Alternating light-darkness-influenced human electrocardiographic magnetoreception in association with geomagnetic pulsations. Biomed Pharmacother 55:63–75. doi:10.1016/S0753-3322(01)90007-1
Otsuka K, Cornelissen G, Weydahl A, Holmeslet B, Hansen TL, Shinagawa M et al (2001b) Geomagnetic disturbance associated with decrease in heart rate variability in a subarctic area. Biomed Pharmacother 55(Suppl 1):51–56. doi:10.1016/S0753-3322(01)90005-8
Palmer S, Rycroft M, Cermack M (2006) Solar and geomagnetic activity, extremely low frequency magnetic and electric fields and human health at the Earth’s surface. Surv Geophys 27:557–595. doi:10.1007/s10712-006-9010-7
Pikin DA, Gurfinkel YI, Oraevskii VN (1998) Effect of geomagnetic disturbances on the blood coagulation system in patients with ischemic heart disease and prospects for correction with medication. Biofizika 43:617–622 (in Russian)
RIA (Russian Information Agency) (2010) Press conference of head physician of Moscow first-aid station of 06.08.2010. http://ria.ru/hs_news/20100805/262028009.html. Accessed 20 February 2013 (in Russian)
Rostoker G, Sharma RP (1980) Correlation of high latitude tropospheric pressure with the structure of the interplanetary magnetic field. Can J Phys 58:255–269
Shindell D, Rind D, Balachandran N, Leon J, Lonergan P (1999) Solar cycle variability, ozone, and climate. Science 284:304–308. doi:10.1126/science.284.5412.305
Siebert M, Meyer J (1996) Geomagnetic activity indices. In: Dieminger W et al (eds) The upper atmosphere. Springer, Berlin, pp 887–911
Stoupel E, Keret R, Assa S, Kaufman H, Shimshoni M, Laron Z (1983) Secretion of growth hormone, prolactin and corticosteroids during different levels of geomagnetic activity. Neuroendocrinol Lett 5:365–368
Stoupel E, Martfel JN, Rotenberg Z (1994) Paroxysmal atrial fibrillation and stroke (cerebrovascular accidents) in males and females above and below age 65 on days of different geomagnetic activity levels. J Basic Clin Physiol Pharmacol 5:315–329. doi:10.1515/JBCPP.1994.5.3-4.315
Stoupel E, Wittenberg C, Zabludowski J, Boner G (1995a) Ambulatory blood pressure monitoring in patients with hypertension on days of high and low geomagnetic activity. J Human Hypertens 9:293–294
Stoupel E, Abramson E, Sulkes J, Martfel J, Stein N, Handelman M et al (1995b) Relationship between suicide and myocardial infarction with regard to changing physical environmental conditions. Int J Biometerol 38:199–203. doi:10.1007/BF01245389
Sung FC, Huang LY, Huang YL, Wang YC (2011) Population-based study on risk of stroke associated with temperature change. Abstracts of the 23th ISEE conference. http://ehp03.niehs.nih.gov/isee/PDF/isee11Abstract00336.pdf. Accessed 20 February 2013
Tofler GH, Brezinski D, Schafer AI, Czeisler CA, Rutherford JD, Willich SN, Gleason RE, Williams GH, Muller JE (1987) Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med 316:1514–1518
Vlak MHM, Rinkel GJE, Greebe P, Van Der Bom JG, Algra A (2011) Trigger factors and their attributable risk for rupture of intracranial aneurysms: a case-crossover study. Stroke 42:1878–1882. doi:10.1161/STROKEAHA.110.606558
Wang XY, Barnett AG, Hu W, Tong S (2009) Temperature variation and emergency hospital admissions for stroke in Brisbane, Australia, 1996–2005. Int J Biometeorol 53:535–541. doi:10.1007/s00484-009-0241-4
Watanabe Y, Hillman DC, Otsuka K, Bingham C, Breus TK, Comtlissen G et al (1994) Cross-spectral coherence between geomagnetic disturbance and human cardiovascular variables at nonsocietal frequencies. Chronobiologia 21:265–272
Watanabe Y, Cornelissen G, Halberg F, Otsuka K, Ohkawa SI (2000) Associations by signatures and coherences between the human circulation and helio- and geomagnetic activity. Biomed Pharmacother 55(Suppl 1):s76–s83. doi:10.1016/S0753-3322(01)90008-3
Wichmann J, Ketzel M, Ellermann T, Loft S (2012) Apparent temperature and acute myocardial infarction hospital admissions in Copenhagen, Denmark: a case-crossover study. Environ Health 11:19. doi:10.1186/1476-069X-11-19
Willich SN (1999) Circadian variation and triggering of cardiovascular events. Vasc Med 4(1):41–49. doi:10.1177/1358836X9900400108
Wolf K, Schneider A, Breitner S, von Klot S, Meisinger C, Cyrys J, Hymer H, Wichmann HE, Peters A (2009) Air temperature and the occurrence of myocardial infarction in Augsburg, Germany. Circulation 120(9):735–742. doi:10.1161/CIRCULATIONAHA.108.815860
Acknowledgments
The authors thank Dr. Julia Shugai from the Skobeltsyn Institute of Nuclear Physics for her consultations on geomagnetic field issues. This research was supported by the grant program of Presidium of Russian Academy of Sciences “Fundamental Sciences for Medicine”.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaposhnikov, D., Revich, B., Gurfinkel, Y. et al. The influence of meteorological and geomagnetic factors on acute myocardial infarction and brain stroke in Moscow, Russia. Int J Biometeorol 58, 799–808 (2014). https://doi.org/10.1007/s00484-013-0660-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-013-0660-0