Abstract
Background
Complement factor B gene (CFB) is an important component of the alternate pathway of complement activation that provides an active subunit that associates with C3b to form the C3 convertase, which is an essential element in complement activation. Among the complement-associated disorders, mutations and pathogenic variants in the CFB gene are relatively rare phenomena. Moreover, mutated CFB affiliation with immune-complex diffuse membranoproliferative glomerulonephritis (IC-MPGN) and atypical hemolytic uremic syndrome (aHUS) are considered a highly rare occurrence.
Case presentation
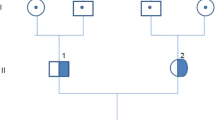
We describe the clinical presentation, course, and pathological findings in a 7-year-old boy who has confirmed CFB heterozygous variants with pathological features compatible with IC-MPGN. Mutational analysis revealed a heterozygous variant p.Glu566Arg in exon 13 of the CFB gene. The patient did not respond to steroids and mycophenolate mofetil (MMF) therapy but responded clinically and biochemically to eculizumab treatment. This is the first case report of CFB alteration associated with IC-MPGN and aHUS that was successfully treated with eculizumab.
Conclusions
Heterozygous variants in the CFB gene can be pathogenic and associated with IC-MPGN and aHUS. Early diagnosis and prompt management can be essential in preventing end-stage renal disease. Eculizumab may provide an effective modality of treatment.


Similar content being viewed by others
References
Wong EK, Goodship TH, Kavanagh D (2013) Complement therapy in atypical hemolytic uraemic syndrome (aHUS). Mol Immunol 56(3):199–212
Kavanagh D, Goodship TH, Richards A (2013) Atypical hemolytic uremic syndrome. Semin Nephrol 33(6):508–530
Sartz L, Olin AI, Kristoffersson AC, Ståhl AL, Johansson ME, Westman K, Fremeaux-Bacchi V, Nilsson-Ekdahl K, Karpman D (2012) A novel C3 mutation causing increased formation of the C3 convertase in familial atypical hemolytic uremic syndrome. J Immunol 188(4):2030–2037
Tawadrous H, Maga T, Sharma J, Kupferman J, Smith RJ, Schoeneman M (2010) A novel mutation in the complement factor B gene (CFB) and atypical hemolytic uremic syndrome. Pediatr Nephrol 25(5):947–951
Leroy V, Fremeaux-Bacchi V, Peuchmaur M, Baudouin V, Deschênes G, Macher MA, Loirat C (2011) Membranoproliferative glomerulonephritis with C3NeF and genetic complement dysregulation. Pediatr Nephrol 26(3):419–424
Hou J, Markowitz GS, Bomback AS, Appel GB, Herlitz LC, Barry Stokes M, D’Agati VD (2014) Toward a working definition of C3 glomerulopathy by immunofluorescence. Kidney Int 85(2):450–456
Sethi S, Fervenza FC (2012) Membranoproliferative glomerulonephritis--a new look at an old entity. N Engl J Med 366(12):1119–1131
Volokhina E, Westra D, Xue X, Gros P, van de Kar N, van den Heuvel L (2012) Novel C3 mutation p.Lys65Gln in aHUS affects complement factor H binding. Pediatr Nephrol 27(9):1519–1524
Cayci FS, Cakar N, Hancer VS, Uncu N, Acar B, Gur G (2012) Eculizumab therapy in a child with hemolytic uremic syndrome and CFI mutation. Pediatr Nephrol 27(12):2327–2331
Imamura H, Konomoto T, Tanaka E, Hisano S, Yoshida Y, Fujimura Y, Miyata T, Nunoi H (2015) Familial C3 glomerulonephritis associated with mutations in the gene for complement factor B. Nephrol Dial Transplant 30(5):862–864
Sethi S, Smith RJ, Dillon JJ, Fervenza FC (2015) C3 glomerulonephritis associated with complement factor B mutation. Am J Kidney Dis 65(3):520–521
Marinozzi MC, Vergoz L, Rybkine T, Ngo S, Bettoni S, Pashov A, Cayla M, Tabarin F, Jablonski M, Hue C, Smith RJ, Noris M, Halbwachs-Mecarelli L, Donadelli R, Fremeaux-Bacchi V, Roumenina LT (2014) Complement factor B mutations in atypical hemolytic uremic syndrome-disease-relevant or benign? J Am Soc Nephrol 25(9):2053–2065
Cooper DN, Krawczak M, Polychronakos C, Tyler-Smith C, Kehrer-Sawatzki H (2013) Where genotype is not predictive of phenotype: towards an understanding of the molecular basis of reduced penetrance in human inherited disease. Hum Genet 132(10):1077–1130
Goicoechea de Jorge E, Harris CL, Esparza-Gordillo J, Carreras L, Arranz EA, Garrido CA, López-Trascasa M, Sánchez-Corral P, Morgan BP, Rodríguez de Córdoba S (2007) Gain-of-function mutations in complement factor B are associated with atypical hemolytic uremic syndrome. Proc Natl Acad Sci U S A 104(1):240–245
Bohnsack JF, Tenner AJ, Laurie GW, Kleinman HK, Martin GR, Brown EJ (1985) The C1q subunit of the first component of complement binds to laminin: a mechanism for the deposition and retention of immune complexes in basement membrane. Proc Natl Acad Sci U S A 82(11):3824–3828
Pickering MC, D’Agati VD, Nester CM, Smith RJ, Haas M, Appel GB, Alpers CE, Bajema IM, Bedrosian C, Braun M, Doyle M, Fakhouri F, Fervenza FC, Fogo AB, Frémeaux-Bacchi V, Gale DP, Goicoechea de Jorge E, Griffin G, Harris CL, Holers VM, Johnson S, Lavin PJ, Medjeral-Thomas N, Paul Morgan B, Nast CC, Noel LH, Peters DK, Rodríguez de Córdoba S, Servais A, Sethi S, Song WC, Tamburini P, Thurman JM, Zavros M, Cook HT (2013) C3 glomerulopathy: consensus report. Kidney Int 84(6):1079–1089
Khalighi MA, Wang S, Henriksen KJ, Bock M, Keswani M, Meehan SM, Chang A (2016) Revisiting post-infectious glomerulonephritis in the emerging era of C3 glomerulopathy. Clin Kidney J 9(3):397–402
Vernon KA, Goicoechea de Jorge E, Hall AE, Fremeaux-Bacchi V, Aitman TJ, Cook HT, Hangartner R, Koziell A, Pickering MC (2012) Acute presentation and persistent glomerulonephritis following streptococcal infection in a patient with heterozygous complement factor H-related protein 5 deficiency. Am J Kidney Dis 60(1):121–125
Kavanagh D, Richards A, Atkinson J (2008) Complement regulatory genes and hemolytic uremic syndromes. Annu Rev Med 59:293–309
Sethi S, Fervenza FC (2014) Pathology of renal diseases associated with dysfunction of the alternative pathway of complement: C3 glomerulopathy and atypical hemolytic uremic syndrome (aHUS). Semin Thromb Hemost 40(4):416–421
Authors’ contributions
• Khalid Alfakeeh: Clinical management and follow-up, data collection and review of the manuscript.
• Mohammed Azar: Clinical management and follow-up, data collection and writing the manuscript.
• Majid Alfadhel: Comment on genetic analysis and review of the manuscript.
• Alsuayri Mansour Abdullah: Data collection.
• Nourah Aludah: Pathological interpretation, image capture, and manuscript review.
• Khaled O. Alsaad: Pathological interpretation, manuscript composition
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consent for the publication of this case report and any accompanying images has been obtained from the patient’s mother. A copy of the written consent is available for review by the editor.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Alfakeeh, K., Azar, M., Alfadhel, M. et al. Rare genetic variant in the CFB gene presenting as atypical hemolytic uremic syndrome and immune complex diffuse membranoproliferative glomerulonephritis, with crescents, successfully treated with eculizumab. Pediatr Nephrol 32, 885–891 (2017). https://doi.org/10.1007/s00467-016-3577-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3577-0