Abstract
Introduction of the so-called biocompatible peritoneal dialysis (PD) fluids was based on a large body of experimental evidence and various clinical trials suggesting important clinical benefits. Of these, until now, only preservation of residual renal function—likely due to lower glucose degradation product load and, in case of icodextrin, improved fluid and blood pressure control—have consistently been proven, whereas the impact on important clinical endpoints such as infectious complications, preservation of PD membrane transport function, and patient outcome, are still debated. In view of the high morbidity and mortality rates of PD patients, novel approaches are warranted and comprise the search for alternative osmotic agents and enrichment of PD fluids with specific pharmacologic agents, such as alanyl-glutamine, potentially counteracting local but also systemic sequelae of uremia and PD.
Similar content being viewed by others
Medical need: What happens to the patient on PD in 2016?
Treatment with peritoneal dialysis (PD) allows home-based renal replacement therapy (RRT) and thus better patient integration into normal social life, such as school and other aspects important for quality of life (QoL), even though imposing a major burden to families. In pediatric nephrology, PD is the most frequently used dialysis modality until adolescence [1]. More than 90 % of young children are treated with PD as RRT within the first 2 years of life [2]. This is exactly the opposite distribution to adult patients on dialysis, in whom <10 % are treated by PD worldwide, despite improving outcome [3]. Whereas data on morbidity and mortality comparing different forms of dialysis in pediatrics are scarce, such data in adults mostly show comparable outcome, depending on population selection and cultural and socioeconomic background of the healthcare system in the countries in which the studies where performed. Latest analyses of adult patients on RRT even suggest a superior outcome of PD compared with hemodialysis (HD) but a strikingly declining PD usage, at least in Europe [3]. Moreover, studies in the adult population show consistent advantages of PD with regard to QoL indices and economic costs to healthcare providers [4, 5]. However, despite technological progress allowing an acceptable QoL for children waiting for renal transplantation [6], PD treatment is still frequently hampered by infectious and noninfectious complications. A recent large competitive risk analysis in almost 9,000 elderly patients, of whom 50 % required assistance at home, demonstrated that 25 % experienced at least one episode of peritonitis within 1 year. Even without having experienced peritonitis, within 2 years, 11 % of PD patients switched to HD, and >20 % of PD patients died [7]. The individual impact of PD on mortality is difficult to interpret due to the multimorbidity of these cohorts. In pediatrics, data from [2] demonstrated that 20 % of children who were started on PD within the first year of life and who had an array of comorbid conditions died within the first 2 years of treatment, mainly because of infections [2]. Overall, survival of pediatric patients on PD is 94 % at 5 years in countries with a per-capita gross national income above US $28,000 per year and 89 % in countries with lower income [8]. Thus, survival of children with chronic renal failure who end on PD therapy is no better than in children with common oncologic diagnoses [9]. Infectious complication and hospitalization rates declined over the past 30 years in children on PD but are still two- and three-fold higher than in children on HD and after kidney transplantation, respectively [10]. The International Pediatric Hemodialysis Network (IPHN; www.pedpd.org) has monitored children on HD for 3 years and will allow respective comparisons with children on PD. Taken together, there is a high medical need to improve the clinical outcome of children who undergo PD. Current clinical and experimental data suggest that the nonphysiological composition of PD fluids plays a major role in putting the child at risk for infectious and noninfectious complications. This review first focuses on the current status of PD fluids then discusses underlying pathomechanisms that put patients at risk for peritoneal and systemic complications and, second, provides a short summary and outlook on current research and development to tackle these problems in order to improve PD therapy.
Current PD solutions
The indication for PD fluids is replacement of renal function in acute and chronic renal failure, thus the removal of water and solutes (including uremic toxins) from the uremic patient. The therapeutic effects of these fluids are achieved through their physicochemical composition, i.e., ultrafiltration (UF) of water by the nonphysiologically increased concentration of osmotically or oncotically active agents (such as glucose, icodextrin or amino acids, resulting in an osmolality of 284 mOsmol/l with 7.5 % icodextrin to 511 mOsmol/l with 4.25 % glucose) and low concentrations or absence of solutes that should be removed (mostly intracellular ions, including potassium and phosphate and multiple metabolic waste products). Currently, registered single-chamber-bag glucose-based PD fluids are CAPD®, Dianeal®, and Gambrosol®, and the so-called biocompatible multi-chamber-bag fluids are BicaVera®, Balance®, Gambrosol trio®, Physioneal®, and the non-glucose-based fluids Nutrineal® and Extraneal® (details in [16]. Additional bioincompatibility of these fluids is introduced by pharmaceutical production (e.g., with heat sterilization), resulting in glucose degradation products (GDP) and adducts, but also by economic constraints (such as absence of essential nutrients, as would be present in most cell culture media). As a result, PD fluids are bioincompatible (if not frankly cytotoxic), with different profiles depending on the osmolar active compound and packaging [11].
Composition of PD fluids
Currently, all PD fluids are heat sterilized (Fig. 1). Worldwide, the most abundantly used mixture has remained largely unchanged since its clinical introduction about 50 years ago. In these single-chamber-bags, glucose levels >10–50× normal serum levels are heat sterilized together at acidic pH with selected electrolytes (Na, Ca, Mg, and Cl) and a buffer (lactate). Concentration of the nonphysiological dialysate buffer lactate is 35-fold above normal serum levels; the unphysiologically low pH (5.5) is chosen to reduce generation of highly reactive and cytotoxic GDP and glucose caramelization [12]. This bioincompatibility has been a matter of active research for >30 years and has resulted in more physiological compounding of glucose-based PD fluids in multihamber bags, in which glucose, electrolytes, and buffer substances are separately stored and heat sterilized [13]. This “second generation” of PD fluids allows use of the physiologic buffer bicarbonate at supraphysiological concentrations (34 mmol/l) or at physiological concentration when combined with lactate. Moreover, the separation of glucose and buffer substances allows heat sterilization of glucose at extremely low pH (2–3), resulting in markedly lower—but still biologically relevant—concentrations of GDP and a markedly higher pH (8–9) in the buffer compartment, resulting in neutral to physiological pH of the ready-mixed glucose-based PD fluids prior to clinical use (pH 7–7.4).
Ontology of peritoneal dialysis (PD) fluids: For ~50 years, conventional PD fluids have been based on glucose as the osmotically active agent and are heat sterilized in single-chamber bags at acidic pH with selected electrolytes (Na, Ca, Mg, and Cl) and a buffer (lactate), resulting in glucose degradation product (GDP) production. In the early 1990s, improved biocompatibility was achieved by introducing multichamber bags to reduce generation of GDP and allow the use of more physiologic buffers (such as bicarbonate) and pH. At the same time, alternative agents were introduced, such as an osmotically active amino acid mixture and the oncotically active glucose polymer icodextrin
In addition, alternative osmotically (or oncotically) active agents were introduced in single-chamber bags, such as the glucose polymer icodextrin and a mixture of amino acids. Albeit reducing the typical toxicity of glucose (heat sterilization of icodextrin still results in glucose degradation byproducts), these novel compounds exhibit nonspecific (such as low pH) and novel substance-specific bioincompatible properties. For example, use of icodextrin resulted in sterile inflammation, most likely due to contamination with bacterial fragments during the production process [14, 15], and an increase in serum levels of icodextrin and its degradation products. Use of amino acids (compounded in PD fluid at about 10× their physiologic serum levels) resulted in different specific perturbances of biological functions, such as vascular effects of arginine [16]. Stable isotope studies in adult continuous ambulatory peritoneal dialysis (CAPD) patients using once-daily amino acid PD solution together with glucose-containing fluid demonstrated improved protein anabolism and a 4 % higher protein synthesis rate compared with patients treated with a glucose-containing PD solution only [17, 18]. According to the International Pediatric Peritoneal Dialysis Network (IPPN) (www.pedpd.org), only 3 % of PD patients use amino-acid-containing fluids, presumably due to the limited anabolic effect and the widespread use of tube feeding.
Low-sodium PD fluids have yielded ambiguous findings in adult PD patients. Applying dialysate solutions with <105 mmol/l of sodium resulted in loss of UF, unless the decline in solution osmolarity was compensated for by glucose [19]. PD fluids with mildly reduced sodium content applied throughout increased dialytic sodium removal by 50 % and reduced blood pressure, but this was accompanied by a decline in residual renal function [20]. Likewise, the concept of adapted automated PD of combining small, short cycles followed by long, large cycles without increasing total dialysate fluid exposure per session might have the potential to improve dialytic sodium removal and blood pressure control and thus to mitigating cumulative PD-fluid-associated toxicity [21]. Mechanisms of the speculated enhanced diffusive transport, however, remain elusive and are not readily explained by the current three-pore model. Suggested benefits need to be balanced against potential risks, e.g., associated with higher intraperitoneal pressure during the large dwells, and require thorough assessment in the pediatric population [22].
Clinical impact of low GDP PD fluids
With regard to actual outcome data obtained in adequate clinical trials, the level of evidence for improved clinical outcome is still not undisputable in favor of the novel PD fluids. Early clinical trials demonstrated an improved biocompatibility based on effluent markers, such as mesothelial cell viability marker cancer antigen 125 (CA-125) [23, 24], interstitial integrity markers hyaluronan, procollagen-1-C-terminal peptide, and procollagen-3-N-terminal peptide [25], effluent surrogate marker of angiogenesis, vascular endothelial growth factor (VEGF), and of inflammation and interleukin (IL) 6 [26]. Effluent IL6 concentrations predict the highly variable individual peritoneal membrane solute transport function [27]. In a recent Cochrane analysis of clinical benefits of PD solutions, the authors concluded that low GDP fluids do not induce any further harm in PD patients but do not improve the incidence of infectious complications such as peritonitis or preserve long-term peritoneal membrane transport function [28]. Icodextrin solutions improve UF and hydration status. Initially unexpected, the use of two-chamber bags resulted in improved and prolonged maintenance of residual renal urine output and higher residual renal function >12 months of use [28], possibly due to the reduction of GDP-related renal cytotoxicity [29]. However, it can be regarded as a prototype of the level of evidence-based medicine in PD that the largest (and likely best) trial failed in its primary outcome parameter, slowing the rate of glomerular filtration rate (GFR) decline [30]. However, that trial turned out to provide evidence for a protective effect with regard to infectious complications by significantly reducing the incidence of nonpseudomonas Gram-negative peritonitis episodes and the overall severity of peritonitis episodes [31]. Based on these findings, cost effectiveness of low GDP fluid usage has been suggested [32]. Thus, current outcome data in adults still corroborate the notion of the European Pediatric Dialysis Working Group (EPDWG), published in this journal in 2011, that low GDP PD fluids should be used whenever possible [11]. This recommendation was based on randomized controlled trials (RCTs) in adult PD patients [23] and on crossover trials in children with low versus high GDP solutions, demonstrating similar peritoneal solute and water transport kinetics [24], reduced systemic GDP and advanced glycation end-product load [33], superior correction of metabolic acidosis, and higher effluent concentrations of mesothelial cell viability surrogate marker CA125 with the pure bicarbonate-based, low-GDP fluid [34]. Since then, some new clinical data have been reported in the pediatric population. A prospective randomized comparison of low GDP fluids revealed better preservation of UF capacity with bicarbonate versus lactate buffer [35]. Moreover, prospectively collected data in the IPPN suggests improved longitudinal growth in infants treated with low GDP fluids, potentially due to attenuated local and systemic inflammatory and carbonyl stress. This association prevailed even after correction for nutritional status and region but, however, does not rule out confounding factors such as specific socioeconomic status and quality of care associated with low and high GDP fluid usage within the four regions analyzed, and thus requires randomized controlled trials (RCTs) for verification [36].
The impact of low GDP fluids on preservation of long-term peritoneal membrane transport function, however, remains elusive. Small-sized RCTs in adults found no differences in peritoneal transport capacity with low and high GDP fluids over time [37, 38], with the exception of UF capacity in the Euro-Balance trial, in which it declined with pure lactate-buffered low GDP fluid but was fully compensated for by a concomitant increase in residual urine production [23]. In the Balanz trial [39], patients with low GDP fluid usage initially had significantly higher peritoneal solute transport rates, which remained stable over the 2-year follow-up period, and peritoneal UF was lower but increased significantly over time. Patients receiving conventional PD solutions experienced progressive increases in peritoneal solute transport rates and stable peritoneal UF over time. Adequately powered RCTs primarily addressing PD-fluid-induced changes in peritoneal membrane function over time are warranted.
Compelling evidence for a persistently high degree of bioincompatibility of low GDP fluids and thus the still great medical need to improve PD fluids to be used in the pediatric population is emerging from the International Pediatric Peritoneal Biopsy Study Group (see Fig. 2). Data from 110 children (85 % on low GDP fluid) obtained in a global effort and analyzed within the European Training and Research in Peritoneal Dialysis (EuTRiPD) consortium (www.eutripd.eu) demonstrate major transformation of the peritoneal membrane with low GDP fluids, including inflammation, progressive fibrosis and angiogenesis [40], i.e. alterations as previously described with high GDP fluids in adults [41], and clearly exceeding uremia-related alterations reported in adults [42]. Quantitative assessment of the healthy parietal peritoneum and omentum in >100 individuals revealed marked age-dependent variations in blood- and lymphatic-vessel density, and derived reference ranges now provide a framework for future histomorphometric analyses and peritoneal transport modeling [43].
Representative section of the peritoneum of a 13.5-year-old girl on chronic peritoneal dialysis (CPD) devoid of peritonitis. The mesothelial cell layer is still preserved; the submesothelial vessel density [brown cluster of differentiation (CD31) staining], however, is markedly increased despite low glucose degradation product (GDP) fluid usage. The three-layer structure of vessels as reported in healthy controls [43] has disappeared (scale bar = 100 μm)
Pathomechanisms relevant in PD
PD fluids play a major role in triggering and/or propagating pathomechanisms that are likely relevant for local and systemic complications in PD (see Fig. 3). These complications can be categorized into local and systemic and into infectious and noninfectious complications.
Combination of bioincompatibility of current peritoneal dialysis (PD) fluids in combination with infection and chronic inflammation results in abnormal peritoneal repair processes. Oxidative stress, senescence, and inadequate cellular stress responses are pathomechanisms that mediate glucose-related toxicity, enhance chronic inflammation, and reduce peritoneal host defence, thereby contributing to a vicious circle. Epithelial mesenchymal transdifferentiation (EMT) further mediates peritoneal membrane damage by peritoneal fibrosis and angiogenesis, ultimately resulting in technical failure of PD. These pathomechanisms might be amenable to therapeutic interventions by specific counteracting compounds
Local infectious complications—in particular, peritonitis—still belong to the most frequent, debilitating, and costly complications of PD [10]. There is a broad body of clinical and experimental data demonstrating that, in particular, heat-sterilized glucose-based dialysis fluids are detrimental for peritoneal host defense [44]. Initial studies focusing on in vitro exposure of different cells of the peritoneal immune system to glucose-based, single-chamber-bag, acidic, lactate-buffered PD fluids provided clear evidence for severe functional impairment and even cell death following more extended exposure [45]. Earlier studies used unspecific cytotoxicity assays, whereas later studies increasingly focused on the role of glucose-related impairment of cells relevant in peritoneal immune defense [12]. Introduction of the multi-chamber-bag PD fluids has markedly reduced the level of acute cytotoxicity; still, these PD fluids are heat sterilized and contain glucose and GDP at concentrations beyond those that were reported in diabetes patients [46]. Metabolic stress by nonphysiological high-glucose levels induces cellular signaling systems (also) involved in immune defense, thereby increasing the risk of peritoneal infection despite reduced amounts of GDP [47]. Currently marketed alternate osmotic agents also appear to result in relatively impaired peritoneal host defense [48]. Thus, intermittent exposure of the immune-compromised peritoneal cavity with bacterial, viral, or fungal species via touch contamination or transintestinal migration still frequently causes subclinical and clinical inflammatory episodes. At present, peritonitis results in technique failure in 8 % of children on PD and in lethal outcome in 1 % [49].
Infectious stimuli together with repeated physicochemical insults by bioincompatible PD fluids propagate smouldering inflammation in the peritoneal cavity. Experimental research in animal and cell culture systems has established a clear role for IL6 in chronic smouldering inflammation triggered by infectious stimuli [50]. IL6 is not only associated with changes in peritoneal transport characteristics, likely reflecting peritoneal remodeling, but also—when measured systemically—with overall outcome and patient mortality [51]. More recently, the IL17 system has been identified as a further important player in peritoneal inflammation [52–54].
The combination of chronic infectious, inflammatory, and cytotoxic insults—in particular, in the context of a diabetes-like milieu—results in abnormal peritoneal repair and stress processes. In particular, regulation of epithelial mesenchymal transdifferentiation (EMT) has been shown to play a major role in peritoneal fibrosis and angiogenesis, ultimately resulting in UF failure in PD [55]. Regarding how far EMT merely represents a good biomarker by which to monitor PD patient management, or whether EMT is an independent pathomechanism that might be amenable for specific interventions, is an ongoing scientific debate [56]. In addition, oxidative stress and senescence are pathomechanisms that likely mediate glucose-related toxicity, in particular glycation processes by reactive carbonyl compounds, resulting in advanced glycosylation end products (AGEs) [57]. Finally, PD fluids result in abnormal cellular stress responses, with dampening of heat-shock proteins, and increased vulnerability of peritoneal cell populations and thereby in enhanced chronic inflammation, peritoneal membrane damage, and hampered host defense [58–60] .
Ultimately, the above described pathomechanisms might not be relevant for local infectious and noninfectious complications only but also for systemic effects, such as further propagating uremia-induced systemic inflammation. Indeed, use of PD fluids that are more biocompatible has resulted in some evidence of reduced systemic inflammation [61] and better maintained residual renal function [28].
Future solutions
Based on the concept that the common denominator for most pathomechanisms underlying local and systemic complications of PD is glucose-related toxicity, two PD-fluid-related work streams to improve PD therapy become obvious: replacement of glucose by alternative, biologically inert, but osmotic active substances; and/or addition of active compounds to counteract glucose-related toxicity.
The main problem in replacing glucose in PD fluids comes from the massive total daily amount of any such osmotic compound needed. Provided an average prescription of four 2-l bags of 1.5 % glucose-based PD fluid to an adult patient, the local peritoneal exposure amounts to 120 g of glucose, of which more than half is systemically absorbed. Replacement of glucose by amino acids is therefore limited to a single exchange per day due to specific adverse effects, such as elevation of blood urea nitrogen, metabolic acidosis, and uremic symptoms [62]. Absorption of the osmotic agent can only be reduced by using larger compounds, such as icodextrin, but still results in potentially relevant systemic loads [63]. Taken together, the daily absorbed amount of any small/low molecular weight solute from PD fluid needs careful consideration of eventual systemic intolerability, especially in this population with virtually nonexistent renal clearance. Although in experimental PD systems several compounds with attractive biochemical profiles have been successfully applied to replace glucose, only very few of these were ultimately tested in PD patients, and none of them has been approved for clinical use to date. Recently, the glucose-replacing sweetener, stevioside, has been patented for PD use. Hyperbranched polyglycerol has experimentally been introduced as a non-glucose-based osmotic agent in PD fluid and showed promising data in early animal studies [64]. However, due to the above-mentioned need to exclude long-term systemic toxicity of these compounds, administered at doses far above the naturally occurring exposure levels in the vulnerable PD population, extensive safety studies are required prior to their introduction into clinical practice. Therefore, the use of clinically available alternative solids is currently limited to icodextrin and an amino acid mix dosed as a single bag per day.
Due to the relative safety of glucose experienced over >50 years of intraperitoneal use and its well-known side effects, an alternative approach is the addition of active compounds counteracting glucose-related toxicity (see Fig. 3). The majority of these compounds (as reviewed in detail in [65] and in [66]) have been selected by a hypothesis-driven approach. Several of these compounds are highly specific pharmacologic agents or biologics that counteract specific pathways identified to be relevant in PD-related complications. For example, peroxisome proliferator-activated receptor (PPAR)-gamma agonists, such as rosiglitazone, have been shown in experimental PD systems to result in improved membrane integrity and to reduce inflammation. Addition of bone morphogenic protein (BMP)-7 mitigates mechanisms such as chronic inflammation and EMT (reviewed in detail in [65], [66]). More recently, use of antagomir has proven to effectively counteract peritoneal fibrosis in a rodent model of PD [67]. However, similar to the case with complete replacement of glucose, these specific medications will need thorough preclinical and clinical testing before the possibility of their clinical use. According to www.clinicaltrials.gov, of these compounds, only glycosaminoglycans such as heparin and low molecular weight heparinoids have reached the clinical stage but have not resulted in reproducible clinical benefits (online search January 2016).
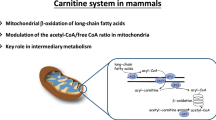
Another promising approach is the addition of nontoxic agents to PD fluids in doses shown to be safe by prior use as nutritional supplements in patients with stage 5 chronic kidney disease on dialysis (CKD5D). Historically, several such compounds were tested in experimental settings but did not successfully undergo further clinical development (http://www.uptodate.com/contents/peritoneal-dialysis-solutions). Of these compounds, only carnitine and alanyl-glutamine dipeptide are in clinical development. For both agents, favorable profiles of systemic effects have been previously reported, such as improved metabolism and immune competence [68]. In a recent phase II trial in nondiabetic PD patients, carnitine-enriched PD fluids improved glucose metabolism [69]. Addition of alanyl-glutamine has resulted in restoration of cellular stress responses, attenuation of peritoneal inflammation, and protection of the peritoneal membrane in experimental systems [54, 60] and is being tested in a phase II trial (EudraCT Number: 2013-000400-42). It certainly remains to be proven in prospective phase III trials whether novel “third-generation PD fluids” are able to prevent the complications that currently hamper PD treatment.
Perspectives
A large body of experimental evidence and respective RCTs have resulted in the introduction of the currently available, so-called biocompatible, PD fluids, which have yielded certain clinical benefits such as better preservation of residual renal function and, in the case of icodextrin, improved fluid control and blood pressure. However, they still exert considerable toxicity, and their benefits regarding infectious complications, PD membrane preservation, cardiovascular health, and patient survival still need demonstration. PD patient morbidity and mortality is still unacceptably high in both adult and pediatric patients, mandating innovative approaches, i.e., PD fluids with less local and systemic toxicity and, ideally, even actively counteracting uremic sequelae such as carbonyl and oxidative stress, as may be the case with specific pharmacologic agents such as alanyl-glutamine dipeptide. Introduction of various novel PD fluids with specific local and systemic benefits should allow for a more personalized treatment of PD patients. Not all patients may benefit from these more costly PD fluids, and thus identification of those who will have a particularly high benefit from the novel therapy or who have a particularly high risk with the current standard fluids is required. Thus, development of new PD fluids must go hand-in-hand with the development of biomarkers to identify patients in need of these innovative therapies. How far this approach will improve overall outcome and QoL of PD patients will be the topic of future research.
References
Kramer AM, van Stralen KJ, Jager KJ, Schaefer F, Verrina E, Seeman T, Lewis MA, Boehm M, Simonetti GD, Novljan G, Groothoff JW (2011) Demographics of blood pressure and hypertension in children on renal replacement therapy in Europe. Kidney Int 80:1092–1098
van Stralen KJ, Borzych-Duzalka D, Hataya H, Kennedy SE, Jager KJ, Verrina E, Inward C, Ronnholm K, Vondrak K, Warady BA, Zurowska AM, Schaefer F, Cochat P, ESPN/ERA-EDTA registry, IPPN registry, ANZDATA registry, Japanese RRT registry (2014) Survival and clinical outcomes of children starting renal replacement therapy in the neonatal period. Kidney Int 86:168–174
van de Luijtgaarden MW, Jager KJ, Segelmark M, Pascual J, Collart F, Hemke AC, Remon C, Metcalfe W, Miguel A, Kramar R, Aasarod K, Abu Hanna A, Krediet RT, Schon S, Ravani P, Caskey FJ, Couchoud C, Palsson R, Wanner C, Finne P, Noordzij M (2016) Trends in dialysis modality choice and related patient survival in the ERA-EDTA Registry over a 20-year period. Nephrol Dial Transplant 31:120–128
Park KS, Hwang YJ, Cho MH, Ko CW, Ha IS, Kang HG, Cheong HI, Park YS, Lee YJ, Lee JH, Cho HY (2012) Quality of life in children with end-stage renal disease based on a PedsQL ESRD module. Pediatr Nephrol 27:2293–2300
Klarenbach SW, Tonelli M, Chui B, Manns BJ (2014) Economic evaluation of dialysis therapies. Nat Rev Nephrol 10:644–652
Chiu MC, Ng CF, Lee LP, Lai WM, Lau SC (2007) Automated peritoneal dialysis in children and adolescents--benefits: a survey of patients and parents on health-related quality of life. Perit Dial Int 27(Suppl 2):S138–142
Evans DW, Ryckelynck JP, Fabre E, Verger C (2010) Peritonitis-free survival in peritoneal dialysis: an update taking competing risks into account. Nephrol Dial Transplant 25:2315–2322
Schaefer F, Borzych-Duzalka D, Azocar M, Munarriz RL, Sever L, Aksu N, Barbosa LS, Galan YS, Xu H, Coccia PA, Szabo A, Wong W, Salim R, Vidal E, Pottoore S, Warady BA, IPPN investigators (2012) Impact of global economic disparities on practices and outcomes of chronic peritoneal dialysis in children: insights from the International Pediatric Peritoneal Dialysis Network Registry. Perit Dial Int 32:399–409
Pui CH, Yang JJ, Hunger SP, Pieters R, Schrappe M, Biondi A, Vora A, Baruchel A, Silverman LB, Schmiegelow K, Escherich G, Horibe K, Benoit YC, Izraeli S, Yeoh AE, Liang DC, Downing JR, Evans WE, Relling MV, Mullighan CG (2015) Childhood Acute Lymphoblastic Leukemia: Progress Through Collaboration. J Clin Oncol 33:2938–2948
Lofaro D, Vogelzang JL, van Stralen KJ, Jager KJ, Groothoff JW (2015) Infection-related hospitalizations over 30 years of follow-up in patients starting renal replacement therapy at pediatric age. Pediatr Nephrol 31:315–323
Schmitt CP, Bakkaloglu SA, Klaus G, Schroder C, Fischbach M (2011) Solutions for peritoneal dialysis in children: recommendations by the European Pediatric Dialysis Working Group. Pediatr Nephrol 26:1137–1147
Wieslander AP, Kjellstrand PT, Rippe B (1995) Heat sterilization of glucose-containing fluids for peritoneal dialysis: biological consequences of chemical alterations. Perit Dial Int 15(7 Suppl):S52–59, discussion S59-60
Passlick-Deetjen J, Lage C (2000) Lactate-buffered and bicarbonate-buffered solutions with less glucose degradation products in a two-chamber system. Perit Dial Int 20(Suppl 2):S42–47
Martis L, Patel M, Giertych J, Mongoven J, Taminne M, Perrier MA, Mendoza O, Goud N, Costigan A, Denjoy N, Verger C, Owen WF Jr (2005) Aseptic peritonitis due to peptidoglycan contamination of pharmacopoeia standard dialysis solution. Lancet 365:588–594
Adam FU, Singan M, Ozelsancak R, Torun D, Ozdemir FN, Haberal M (2007) Icodextrin-associated sterile peritonitis: a recent outbreak in Turkey. Perit Dial Int 27:598–599
Reimann D, Dachs D, Meye C, Gross P (2004) Amino acid-based peritoneal dialysis solution stimulates mesothelial nitric oxide production. Perit Dial Int 24:378–384
Tjiong HL, van den Berg JW, Wattimena JL, Rietveld T, van Dijk LJ, van der Wiel AM, van Egmond AM, Fieren MW, Swart R (2005) Dialysate as food: combined amino acid and glucose dialysate improves protein anabolism in renal failure patients on automated peritoneal dialysis. J Am Soc Nephrol 16:1486–1493
Tjiong HL, Rietveld T, Wattimena JL, van den Berg JW, Kahriman D, van der Steen J, Hop WC, Swart R, Fieren MW (2007) Peritoneal dialysis with solutions containing amino acids plus glucose promotes protein synthesis during oral feeding. Clin J Am Soc Nephrol 2:74–80
Davies S, Carlsson O, Simonsen O, Johansson AC, Venturoli D, Ledebo I, Wieslander A, Chan C, Rippe B (2009) The effects of low-sodium peritoneal dialysis fluids on blood pressure, thirst and volume status. Nephrol Dial Transplant 24:1609–1617
Rutkowski B, Tam P, van der Sande FM, Vychytil A, Schwenger V, Himmele R, Gauly A (2016) Low-Sodium Versus Standard-Sodium Peritoneal Dialysis Solution in Hypertensive Patients: A Randomized Controlled Trial. Am J Kidney Dis 67:753–761
Fischbach M, Issad B, Dubois V, Taamma R (2011) The beneficial influence on the effectiveness of automated peritoneal dialysis of varying the dwell time (short/long) and fill volume (small/large): a randomized controlled trial. Perit Dial Int 31:450–458
Fischbach M, Schmitt CP, Shroff R, Zaloszyc A, Warady BA (2016) Increasing sodium removal on peritoneal dialysis: applying dialysis mechanics to the peritoneal dialysis prescription. Kidney Int 89:761–766
Williams JD, Topley N, Craig KJ, Mackenzie RK, Pischetsrieder M, Lage C, Passlick-Deetjen J (2004) The Euro-Balance Trial: the effect of a new biocompatible peritoneal dialysis fluid (balance) on the peritoneal membrane. Kidney Int 66:408–418
Schmitt CP, Haraldsson B, Doetschmann R, Zimmering M, Greiner C, Boswald M, Klaus G, Passlick-Deetjen J, Schaefer F (2002) Effects of pH-neutral, bicarbonate-buffered dialysis fluid on peritoneal transport kinetics in children. Kidney Int 61:1527–1536
Rippe B, Simonsen O, Heimburger O, Christensson A, Haraldsson B, Stelin G, Weiss L, Nielsen FD, Bro S, Friedberg M, Wieslander A (2001) Long-term clinical effects of a peritoneal dialysis fluid with less glucose degradation products. Kidney Int 59:348–357
Cooker LA, Luneburg P, Holmes CJ, Jones S, Topley N (2001) IL6 levels decrease in effluent from patients dialyzed with bicarbonate/lactate-based peritoneal dialysis solutions. Perit Dial Int 21(Suppl 3):S102–107
Lambie M, Chess J, Donovan KL, Kim YL, Do JY, Lee HB, Noh H, Williams PF, Williams AJ, Davison S, Dorval M, Summers A, Williams JD, Bankart J, Davies SJ, Topley N, Global Fluid Study Investigators (2013) Independent effects of systemic and peritoneal inflammation on peritoneal dialysis survival. J Am Soc Nephrol 24:2071–2080
Cho Y, Johnson DW, Craig JC, Strippoli GF, Badve SV, Wiggins KJ (2014) Biocompatible dialysis fluids for peritoneal dialysis. Cochrane Database Syst Rev 3, CD007554
Muller-Krebs S, Kihm LP, Zeier B, Gross ML, Deppisch R, Wieslander A, Henle T, Penndorf I, Oh J, Reiser J, Nawroth PP, Zeier M, Schwenger V (2008) Renal toxicity mediated by glucose degradation products in a rat model of advanced renal failure. Eur J Clin Invest 38:296–305
Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, Foo MW, Jones B, Kulkarni H, Langham R, Ranganathan D, Schollum J, Suranyi M, Tan SH, Voss D (2012) Effects of Biocompatible versus Standard Fluid on Peritoneal Dialysis Outcomes. J Am Soc Nephrol 23:1097–1107
Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, Foo MW, Jones B, Kulkarni H, Langham R, Ranganathan D, Schollum J, Suranyi MG, Tan SH, Voss D, balANZ Trial Investigators (2012) The effects of biocompatible compared with standard peritoneal dialysis solutions on peritonitis microbiology, treatment, and outcomes: the balANZ trial. Perit Dial Int 32:497–506
Howard K, Hayes A, Cho Y, Cass A, Clarke M, Johnson DW (2015) Economic evaluation of neutral-pH, low-glucose degradation product peritoneal dialysis solutions compared with standard solutions: a secondary analysis of the balANZ Trial. Am J Kidney Dis 65:773–779
Schmitt CP, von Heyl D, Rieger S, Arbeiter K, Bonzel KE, Fischbach M, Misselwitz J, Pieper AK, Schaefer F (2007) Reduced systemic advanced glycation end products in children receiving peritoneal dialysis with low glucose degradation product content. Nephrol Dial Transplant 22:2038–2044
Haas S, Schmitt CP, Arbeiter K, Bonzel KE, Fischbach M, John U, Pieper AK, Schaub TP, Passlick-Deetjen J, Mehls O, Schaefer F (2003) Improved acidosis correction and recovery of mesothelial cell mass with neutral-pH bicarbonate dialysis solution among children undergoing automated peritoneal dialysis. J Am Soc Nephrol 14:2632–2638
Schmitt CP, Nau B, Gemulla G, Bonzel KE, Holtta T, Testa S, Fischbach M, John U, Kemper MJ, Sander A, Arbeiter K, Schaefer F (2013) Effect of the dialysis fluid buffer on peritoneal membrane function in children. Clin J Am Soc Nephrol 8:108–115
Rees L, Azocar M, Borzych D, Watson AR, Buscher A, Edefonti A, Bilge I, Askenazi D, Leozappa G, Gonzales C, van Hoeck K, Secker D, Zurowska A, Ronnholm K, Bouts AH, Stewart H, Ariceta G, Ranchin B, Warady BA, Schaefer F, International Pediatric Peritoneal Dialysis Network (IPPN) registry (2011) Growth in very young children undergoing chronic peritoneal dialysis. J Am Soc Nephrol 22:2303–2312
Szeto CC, Chow KM, Lam CW, Leung CB, Kwan BC, Chung KY, Law MC, Li PK (2007) Clinical biocompatibility of a neutral peritoneal dialysis solution with minimal glucose-degradation products--a 1-year randomized control trial. Nephrol Dial Transplant 22:552–559
Kim S, Oh J, Kim S, Chung W, Ahn C, Kim SG, Oh KH (2009) Benefits of biocompatible PD fluid for preservation of residual renal function in incident CAPD patients: a 1-year study. Nephrol Dial Transplant 24:2899–2908
Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, Foo MW, Jones B, Kulkarni H, Langham R, Ranganathan D, Schollum J, Suranyi MG, Tan SH, Voss D, balANZ Trial Investigators (2012) The effect of low glucose degradation product, neutral pH versus standard peritoneal dialysis solutions on peritoneal membrane function: the balANZ trial. Nephrol Dial Transplant 27:4445–4453
Schaefer B, Bartosova M, Taylan C, VandeWalle J, Querfeld U, Krmar R, Warady BA, Schmitt CP (2016) The PD membrane microvasculature in uremia and PD – recent findings from the International Pediatric PD biobank. Pediatr Nephrol 31:1729
Williams JD, Craig KJ, Topley N, Von Ruhland C, Fallon M, Newman GR, Mackenzie RK, Williams GT, Peritoneal Biopsy Study Group (2002) Morphologic changes in the peritoneal membrane of patients with renal disease. J Am Soc Nephrol 13:470–479
Williams JD, Craig KJ, von Ruhland C, Topley N, Williams GT (2003) The natural course of peritoneal membrane biology during peritoneal dialysis. Kidney Int Suppl S43-49
Schaefer B, Bartosova M, Macher-Goeppinger S, Ujszaszi A, Wallwiener M, Nyarangi-Dix J, Sallay P, Burkhardt D, Querfeld U, Pfeifle V, Lahrmann B, Schwenger V, Wuhl E, Holland-Cunz S, Schaefer F, Schmitt CP (2016) Quantitative Histomorphometry of the Healthy Peritoneum. Sci Rep 6(6):21344
Mortier S, Lameire NH, De Vriese AS (2004) The effects of peritoneal dialysis solutions on peritoneal host defense. Perit Dial Int 24:123–138
Mackenzie R, Holmes CJ, Jones S, Williams JD, Topley N (2003) Clinical indices of in vivo biocompatibility: the role of ex vivo cell function studies and effluent markers in peritoneal dialysis patients. Kidney Int Suppl 64(Suppl 88):S84–93
Sitter T, Sauter M (2005) Impact of glucose in peritoneal dialysis: saint or sinner? Perit Dial Int 25:415–425
Kumar PS, Mauriello CT, Hair PS, Rister NS, Lawrence C, Raafat RH, Cunnion KM (2015) Glucose-based dialysis fluids inhibit innate defense against Staphylococcus aureus. Mol Immunol 67:575–583
Mortier S, Faict D, Gericke M, Lameire N, De Vriese A (2005) Effects of new peritoneal dialysis solutions on leukocyte recruitment in the rat peritoneal membrane. Nephron Exp Nephrol 101:e139–145
Warady BA, Feneberg R, Verrina E, Flynn JT, Muller-Wiefel DE, Besbas N, Zurowska A, Aksu N, Fischbach M, Sojo E, Donmez O, Sever L, Sirin A, Alexander SR, Schaefer F, IPPR (2007) Peritonitis in children who receive long-term peritoneal dialysis: a prospective evaluation of therapeutic guidelines. J Am Soc Nephrol 18:2172–2179
Fielding CA, Jones GW, McLoughlin RM, McLeod L, Hammond VJ, Uceda J, Williams AS, Lambie M, Foster TL, Liao CT, Rice CM, Greenhill CJ, Colmont CS, Hams E, Coles B, Kift-Morgan A, Newton Z, Craig KJ, Williams JD, Williams GT, Davies SJ, Humphreys IR, O’Donnell VB, Taylor PR, Jenkins BJ, Topley N, Jones SA (2014) IL6 signaling drives fibrosis in unresolved inflammation. Immunity 40:40–50
Cho Y, Johnson DW, Vesey DA, Hawley CM, Pascoe EM, Clarke M, Topley N, balANZ Trial Investigators (2015) Baseline serum interleukin-6 predicts cardiovascular events in incident peritoneal dialysis patients. Perit Dial Int 35:35–42
Gonzalez-Mateo GT, Fernandez-Millara V, Bellon T, Liappas G, Ruiz-Ortega M, Lopez-Cabrera M, Selgas R, Aroeira LS (2014) Paricalcitol Reduces Peritoneal Fibrosis in Mice through the Activation of Regulatory T Cells and Reduction in IL-17 Production. PLoS One 9, e108477
Sandoval P, Loureiro J, Gonzalez-Mateo G, Perez-Lozano ML, Maldonado-Rodriguez A, Sanchez-Tomero JA, Mendoza L, Santamaria B, Ortiz A, Ruiz-Ortega M, Selgas R, Martin P, Sanchez-Madrid F, Aguilera A, Lopez-Cabrera M (2010) PPAR-gamma agonist rosiglitazone protects peritoneal membrane from dialysis fluid-induced damage. Lab Invest 90:1517–1532
Ferrantelli E, Liappas G, Vila Cuenca M, Keuning ED, Foster TL, Vervloet MG, Lopez-Cabrera M, Beelen RH (2016) The dipeptide alanyl-glutamine ameliorates peritoneal fibrosis and attenuates IL-17 dependent pathways during peritoneal dialysis. Kidney Int 89:625–635
Aroeira LS, Aguilera A, Sanchez-Tomero JA, Bajo MA, del Peso G, Jimenez-Heffernan JA, Selgas R, Lopez-Cabrera M (2007) Epithelial to mesenchymal transition and peritoneal membrane failure in peritoneal dialysis patients: pathologic significance and potential therapeutic interventions. J Am Soc Nephrol 18:2004–2013
Liu Y, Dong Z, Liu H, Zhu J, Liu F, Chen G (2015) Transition of mesothelial cell to fibroblast in peritoneal dialysis: EMT, stem cell or bystander? Perit Dial Int 35:14–25
Witowski J, Ksiazek K, Jorres A (2008) New insights into the biology of peritoneal mesothelial cells: the roles of epithelial-to-mesenchymal transition and cellular senescence. Nephron Exp Nephrol 108:e69–73
Bender TO, Kratochwill K, Herzog R, Ulbrich A, Bohm M, Jorres A, Aufricht C (2015) Injury-induced inflammation and inadequate HSP expression in mesothelial cells upon repeat exposure to dual-chamber bag peritoneal dialysis fluids. Int J Artif Organs 38:530–536
Kratochwill K, Lechner M, Lichtenauer AM, Herzog R, Lederhuber HC, Siehs C, Endemann M, Mayer B, Rizzi A, Aufricht C (2011) Interleukin-1 receptor-mediated inflammation impairs the heat shock response of human mesothelial cells. Am J Pathol 178:1544–1555
Kratochwill K, Boehm M, Herzog R, Lichtenauer AM, Salzer E, Lechner M, Kuster L, Bergmeister K, Rizzi A, Mayer B, Aufricht C (2012) Alanyl-glutamine dipeptide restores the cytoprotective stress proteome of mesothelial cells exposed to peritoneal dialysis fluids. Nephrol Dial Transplant 27:937–946
Szeto CC, Kwan BC, Chow KM, Cheng PM, Kwong VW, Choy AS, Law MC, Leung CB, Li PK (2015) The Effect of Neutral Peritoneal Dialysis Solution with Low Glucose-Degradation-Product on the Fluid Status and Body Composition--A Randomized Control Trial. PLoS One 10, e0141425
Dombros NV, Prutis K, Tong M, Anderson GH, Harrison J, Sombolos K, Digenis G, Pettit J, Oreopoulos DG (1990) Six-month overnight intraperitoneal amino-acid infusion in continuous ambulatory peritoneal dialysis (CAPD) patients--no effect on nutritional status. Perit Dial Int 10:79–84
Garcia-Lopez E, Lindholm B (2009) Icodextrin metabolites in peritoneal dialysis. Perit Dial Int 29:370–376
Mendelson AA, Guan Q, Chafeeva I, da Roza GA, Kizhakkedathu JN, Du C (2013) Hyperbranched polyglycerol is an efficacious and biocompatible novel osmotic agent in a rodent model of peritoneal dialysis. Perit Dial Int 33:15–27
Farhat K, Stavenuiter AW, Beelen RH, Ter Wee PM (2014) Pharmacologic targets and peritoneal membrane remodeling. Perit Dial Int 34:114–123
Ditsawanon P, Aramwit P (2015) Preserving the peritoneal membrane in long-term peritoneal dialysis patients. J Clin Pharm Ther. doi:10.1111/jcpt.12318
Yu JW, Duan WJ, Huang XR, Meng XM, Yu XQ, Lan HY (2014) MicroRNA-29b inhibits peritoneal fibrosis in a mouse model of peritoneal dialysis. Lab Invest 94:978–990
Tao KM, Li XQ, Yang LQ, Yu WF, Lu ZJ, Sun YM, Wu FX (2014) Glutamine supplementation for critically ill adults. Cochrane Database Syst Rev 9, CD010050
Bonomini M, Di Liberato L, Del Rosso G, Stingone A, Marinangeli G, Consoli A, Bertoli S, De Vecchi A, Bosi E, Russo R, Corciulo R, Gesualdo L, Giorgino F, Cerasoli P, Di Castelnuovo A, Monaco MP, Shockley T, Rossi C, Arduini A (2013) Effect of an L-carnitine-containing peritoneal dialysate on insulin sensitivity in patients treated with CAPD: a 4-month, prospective, multicenter randomized trial. Am J Kidney Dis 62:929–938
Acknowledgments
Claus Peter Schmitt and Christoph Aufricht were principal investigator and supported by the European Training and Research in Peritoneal Dialysis (EuTRiPD) program, a project funded by the European Union within the Marie Curie scheme (287813). Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christoph Aufricht has received research grants and lecture honoraria from Fresenius Medical Care and Baxter Healthcare and is cofounder of Zytoprotec GmbH, a spinoff of the Medical University Vienna that holds the patent “Carbohydrate-based peritoneal dialysis fluid comprising glutamine residue” (International Publication Number WO 2008/106702 A1).
Claus Peter Schmitt has received research grants and lecture honoraria from Fresenius Medical Care and lecture honoraria from Baxter Healthcare.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Schmitt, C.P., Aufricht, C. Is there such a thing as biocompatible peritoneal dialysis fluid?. Pediatr Nephrol 32, 1835–1843 (2017). https://doi.org/10.1007/s00467-016-3461-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3461-y