Abstract
Background
Children with chronic kidney disease (CKD) may have impaired caloric intake through a variety of mechanisms, with decreased appetite as a putative contributor. In adult CKD, decreased appetite has been associated with poor clinical outcomes. There is limited information about this relationship in pediatric CKD.
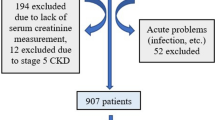
Methods
A total of 879 participants of the Chronic Kidney Disease in Children (CKiD) study were studied. Self-reported appetite was assessed annually and categorized as very good, good, fair, or poor/very poor. The relationship between appetite and iohexol or estimated glomerular filtration rate (ieGFR), annual changes in anthropometrics z-scores, hospitalizations, emergency room visits, and quality of life were assessed.
Results
An ieGFR < 30 ml/min per 1.73 m2 was associated with a 4.46 greater odds (95 % confidence interval: 2.80, 7.09) of having a worse appetite than those with ieGFR >90. Appetite did not predict changes in height, weight, or BMI z-scores. Patients not reporting a very good appetite had more hospitalizations over the next year than those with a very good appetite. Worse appetite was significantly associated with lower parental and patient reported quality of life.
Conclusions
Self-reported appetite in children with CKD worsens with lower ieGFR and is correlated with clinical outcomes, including hospitalizations and quality of life.
Similar content being viewed by others
References
Betts PR, Magrath G (1974) Growth pattern and dietary intake of children with chronic renal insufficiency. Br Med J 2:189–193
Norman LJ, Coleman JE, Macdonald IA, Tomsett AM, Watson AR (2000) Nutrition and growth in relation to severity of renal disease in children. Pediatr Nephrol 15:259–265
Rees L, Jones H (2013) Nutritional management and growth in children with chronic kidney disease. Pediatr Nephrol 28:527–536
Armstrong JE, Laing DG, Wilkes FJ, Kainer G (2010) Smell and taste function in children with chronic kidney disease. Pediatr Nephrol 25:1497–1504
Rees L, Rigden SP, Ward GM (1989) Chronic renal failure and growth. Arch Dis Child 64:573–577
Hijazi R, Abitbol CL, Chandar J, Seeherunvong W, Freundlich M, Zilleruelo G (2009) Twenty-five years of infant dialysis: a single center experience. J Pediatr 155:111–117
Zabel R, Ash S, King N, Juffs P, Bauer J (2012) Relationships between appetite and quality of life in hemodialysis patients. Appetite 59:194–199
Kalantar-Zadeh K, Block G, McAllister CJ, Humphreys MH, Kopple JD (2004) Appetite and inflammation, nutrition, anemia, and clinical outcome in hemodialysis patients. Am J Clin Nut 80:299–307
Furth SL, Abraham AG, Jerry-Fluker J, Schwartz GJ, Benfield M, Kaskel F, Wong C, Mak RH, Moxey-Mims M, Warady BA (2011) Metabolic abnormalities, cardiovascular disease risk factors, and GFR decline in children with chronic kidney disease. Clin J Am Soc Nephrol 6:2132–2140
Schwartz GJ, Abraham AG, Furth SL, Warady BA, Munoz A (2010) Optimizing iohexol plasma disappearance curves to measure the glomerular filtration rate in children with chronic kidney disease. Kidney Int 77:65–71
Ng DK, Schwartz GJ, Jacobson LP, Palella FJ, Margolick JB, Warady BA, Furth SL, Munoz A (2011) Universal GFR determination based on two time points during plasma iohexol disappearance. Kidney Int 80:423–430
Haycock GB, Schwartz GJ, Wisotsky DH (1978) Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr 93:62–66
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Burrowes JD, Larive B, Chertow GM, Cockram DB, Dwyer JT, Greene T, Kusek JW, Leung J, Rocco MV, Hemodialysis Study G (2005) Self-reported appetite, hospitalization and death in haemodialysis patients: findings from the Hemodialysis (HEMO) Study. Nephrol Dial Transplant 20:2765–2774
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL (2000) CDC growth charts: United States. Adv Data 8;(314):1–27
Hullmann SE, Ryan JL, Ramsey RR, Chaney JM, Mullins LL (2011) Measures of general pediatric quality of life: Child Health Questionnaire (CHQ), DISABKIDS Chronic Generic Measure (DCGM), KINDL-R, Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales, and Quality of My Life Questionnaire (QoML). Arthritis Care Res (Hoboken) 63(Suppl 11):S420–S430
Buscher AK, Buscher R, Hauffa BP, Hoyer PF (2010) Alterations in appetite-regulating hormones influence protein-energy wasting in pediatric patients with chronic kidney disease. Pediatr Nephrol 25:2295–2301
Gunta SS, Mak RH (2013) Ghrelin and leptin pathophysiology in chronic kidney disease. Pediatr Nephrol 28:611–616
Foster BJ, McCauley L, Mak RH (2012) Nutrition in infants and very young children with chronic kidney disease. Pediatr Nephrol 27:1427–1439
Bonthuis M, van Stralen KJ, Verrina E, Groothoff JW, Alonso Melgar A, Edefonti A, Fischbach M, Mendes P, Molchanova EA, Paripovic D, Peco-Antic A, Printza N, Rees L, Rubik J, Stefanidis CJ, Sinha MD, Zagozdzon I, Jager KJ, Schaefer F (2013) Underweight, overweight and obesity in paediatric dialysis and renal transplant patients. Nephrol Dial Transplant 28(Suppl 4):iv195–iv204
Wong CS, Hingorani S, Gillen DL, Sherrard DJ, Watkins SL, Brandt JR, Ball A, Stehman-Breen CO (2002) Hypoalbuminemia and risk of death in pediatric patients with end-stage renal disease. Kidney Int 61:630–637
Wong CS, Gipson DS, Gillen DL, Emerson S, Koepsell T, Sherrard DJ, Watkins SL, Stehman-Breen C (2000) Anthropometric measures and risk of death in children with end-stage renal disease. Am J Kidney Dis 36:811–819
Avram MM, Mittman N, Bonomini L, Chattopadhyay J, Fein P (1995) Markers for survival in dialysis: a seven-year prospective study. Am J Kidney Dis 26:209–219
Menon V, Greene T, Wang X, Pereira AA, Marcovina SM, Beck GJ, Kusek JW, Collins AJ, Levey AS, Sarnak MJ (2005) C-reactive protein and albumin as predictors of all-cause and cardiovascular mortality in chronic kidney disease. Kidney Int 68:766–772
Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS, Sarnak MJ (2008) The relationship between nontraditional risk factors and outcomes in individuals with stage 3 to 4 CKD. Am J Kidney Dis 51:212–223
Acknowledgments
Data in this manuscript were collected by the Chronic Kidney Disease in Children prospective cohort study (CKiD) with clinical coordinating centers (Principal Investigators) at Children's Mercy Hospital and the University of Missouri - Kansas City (Bradley Warady, MD) and Children's Hospital of Philadelphia (Susan Furth, MD, PhD), Central Biochemistry Laboratory (George Schwartz, MD) at the University of Rochester Medical Center, and data coordinating center (Alvaro Muñoz, PhD) at the Johns Hopkins Bloomberg School of Public Health. The CKiD Study is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Heart, Lung, and Blood Institute (U01-DK-66143, U01-DK-66174, U01DK-082194, U01-DK-66116). The CKiD website is located at http://www.statepi.jhsph.edu/ckid. Research at Emory University supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000454. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
The study design and conduct were approved by an external study monitoring board appointed by the National Institute of Diabetes and Digestive and Kidney Diseases and by the institutional review boards of each participating center.
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Rights and permissions
About this article
Cite this article
Ayestaran, F.W., Schneider, M.F., Kaskel, F.J. et al. Perceived appetite and clinical outcomes in children with chronic kidney disease. Pediatr Nephrol 31, 1121–1127 (2016). https://doi.org/10.1007/s00467-016-3321-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3321-9