Abstract
Background
Data on global (IV-G) and segmental (IV-S) diffuse proliferative lupus nephritis (DPLN) in children are lacking.
Methods
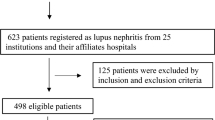
To determine the clinicopathology and prognosis of DPLN subclasses IV-G and IV-S, we analyzed the clinical, laboratory, and demographic data of 56 children aged <18 years diagnosed with DPLN [36 (64.3 %) with IV-G; 20 (35.7 %) with IV-S] between 2004 and 2013. Clinical endpoints were: (1) complete remission (CR), (2) chronic kidney disease [CKD; defined as estimated glomerular filtration rate (eGFR) of <60 mL/min/1.73 m2 or end-stage renal disease (ESRD)], and (3) death.
Results
Proteinuria and the activity index were higher in patients with IV-G (p < 0.05). Global endocapillary proliferation and leukocyte exudation were predominant in IV-G patients, whereas segmental endocapillary proliferation was predominant in patients with IV-S (p < 0.005). CR rates in IV-G and IV-S patients were 50 and 60 %, respectively (p = 0.47). Renal survival rates, defined as an eGFR of ≥60 mL/min/1.73 m2, were 93, 78, and 64 % at 1, 5, and 10 years, respectively. Patient survival rates at 1, 5, and 10 years were 98, 96, and 91 %, respectively. Patient and renal survival rates were similar in both subclasses.
Conclusions
Although patients with IV-G and IV-S displayed some clinical and histopathological disparities, renal outcomes were similar. The majority of children with DPLN reached adulthood but accrued significant renal damage. Treatment regimens which can slow the progression of CKD are needed.


Similar content being viewed by others
References
Perfumo F, Martini A (2005) Lupus nephritis in children. Lupus 14:83–88
Wong SN, Tse KC, Lee TL, Lee KW, Chim S, Lee KP, Wai-Po Chu R, Chan W, Fong KW, Hui J, Po-Siu Li S, Yeung PS, Yuen SF, Chi-Hang Ho A, Chuk-Kwan Leung L, Luk D, Tong PC, Chan SY, Cheung HM, Chow CM, Lau D (2006) Lupus nephritis in Chinese children—a territory-wide cohort study in Hong Kong. Pediatr Nephrol 21:1104–1112
Ruggiero B, Vivarelli M, Gianviti A, Benetti E, Peruzzi L, Barbano G, Corona F, Ventura G, Pecoraro C, Murer L, Ghiggeri GM, Pennesi M, Edefonti A, Coppo R, Emma F (2013) Lupus nephritis in children and adolescents: results of the Italian Collaborative Study. Nephrol Dial Transplant 28:1487–1496
Punaro MG (2013) The treatment of systemic lupus proliferative nephritis. Pediatr Nephrol 28:2069–2078
Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int 65:521–530
Hill GS, Delahousse M, Nochy D, Bariety J (2005) Class IV-S versus class IV-G lupus nephritis: clinical and morphologic differences suggesting different pathogenesis. Kidney Int 68:2288–2297
Silva CA, Avcin T, Brunner HI (2012) Taxonomy for systemic lupus erythematosus with onset before adulthood. Arthritis Care Res 64:1787–1793
Marks SD, Sebire NJ, Pilkington C, Tullus K (2007) Clinicopathological correlations of paediatric lupus nephritis. Pediatr Nephrol 22:77–83
Mackie FE, Kainer G, Adib N, Boros C, Elliott EJ, Fahy R, Munro J, Murray K, Rosenberg A, Wainstein B, Ziegler JB, Singh-Grewal D (2015) The national incidence and clinical picture of SLE in children in Australia—a report from the Australian Paediatric Surveillance Unit. Lupus 24:66–73
Hiraki LT, Benseler SM, Tyrrell PN, Hebert D, Harvey E, Silverman ED (2008) Clinical and laboratory characteristics and long-term outcome of pediatric systemic lupus erythematosus: a longitudinal study. J Pediatr 152:550–556
Sato VA, Marques ID, Goldenstein PT, Carmo LP, Jorge LB, Titan SM, Barros RT, Woronik V (2012) Lupus nephritis is more severe in children and adolescents than in older adults. Lupus 21:978–983
Gladman DD, Ibanez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29:288–291
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34:571–590
Austin HA 3rd, Muenz LR, Joyce KM, Antonovych TA, Kullick ME, Klippel JH, Decker JL, Balow JE (1983) Prognostic factors in lupus nephritis. Contribution of renal histologic data. Am J Med 75:382–391
Renal Disease Subcommittee of the American College of Rheumatology Ad Hoc Committee on Systemic Lupus Erythematosus Response Criteria (2006) The American College of Rheumatology response criteria for proliferative and membranous renal disease in systemic lupus erythematosus clinical trials. Arthritis Rheum 54:421–432
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS (2003) National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421
Najafi CC, Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J (2001) Significance of histologic patterns of glomerular injury upon long-term prognosis in severe lupus glomerulonephritis. Kidney Int 59:2156–2163
Mittal B, Hurwitz S, Rennke H, Singh AK (2004) New subcategories of class IV lupus nephritis: are there clinical, histologic, and outcome differences? Am J Kidney Dis 44:1050–1059
Haring CM, Rietveld A, van den Brand JA, Berden JH (2012) Segmental and global subclasses of class IV lupus nephritis have similar renal outcomes. J Am Soc Nephrol 23:149–154
Yu F, Tan Y, Wu LH, Zhu SN, Liu G, Zhao MH (2009) Class IV-G and IV-S lupus nephritis in Chinese patients: a large cohort study from a single center. Lupus 18:1073–1081
Zappitelli M, Duffy CM, Bernard C, Gupta IR (2008) Evaluation of activity, chronicity and tubulointerstitial indices for childhood lupus nephritis. Pediatr Nephrol 23:83–91
Wu Q, Tanaka H, Hirukawa T, Endoh M, Fukagawa M (2012) Characterization and quantification of proliferating cell patterns in endocapillary proliferation. Nephrol Dial Transplant 27:3234–3241
Nived O, Hallengren CS, Alm P, Jonsen A, Sturfelt G, Bengtsson AA (2013) An observational study of outcome in SLE patients with biopsy-verified glomerulonephritis between 1986 and 2004 in a defined area of southern Sweden: the clinical utility of the ACR renal response criteria and predictors for renal outcome. Scand J Rheumatol 42:383–389
Schwartz MM, Korbet SM, Katz RS, Lewis EJ (2009) Evidence of concurrent immunopathological mechanisms determining the pathology of severe lupus nephritis. Lupus 18:149–158
Sule SD, Moodalbail DG, Burnham J, Fivush B, Furth SL (2015) Predictors of kidney disease in a cohort of pediatric patients with lupus. Lupus. doi:10.1177/0961203315570162
Wu JY, Yeh KW, Huang JL (2014) Early predictors of outcomes in pediatric lupus nephritis: focus on proliferative lesions. Semin Arthritis Rheum 43:513–520
Knight AM, Weiss PF, Morales KH, Keren R (2014) National trends in pediatric systemic lupus erythematosus hospitalization in the United States: 2000–2009. J Rheumatol 41:539–546
Pereira T, Abitbol CL, Seeherunvong W, Katsoufis C, Chandar J, Freundlich M, Zilleruelo G (2011) Three decades of progress in treating childhood-onset lupus nephritis. Clin J Am Soc Nephrol 6:2192–2199
Lee BS, Cho HY, Kim EJ, Kang HG, Ha IS, Cheong HI, Kim JG, Lee HS, Choi Y (2007) Clinical outcomes of childhood lupus nephritis: a single center’s experience. Pediatr Nephrol 22:222–231
Gibson KL, Gipson DS, Massengill SA, Dooley MA, Primack WA, Ferris MA, Hogan SL (2009) Predictors of relapse and end stage kidney disease in proliferative lupus nephritis: focus on children, adolescents, and young adults. Clin J Am Soc Nephrol 4:1962–1967
Ethical approval
This study was approved by the Institutional Review Board Committee of Faculty of Medicine, Chulalongkorn University. All procedures performed in studies involving human participants are in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. Patient anonymity was preserved.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rianthavorn, P., Buddhasri, A. Long-term renal outcomes of childhood-onset global and segmental diffuse proliferative lupus nephritis. Pediatr Nephrol 30, 1969–1976 (2015). https://doi.org/10.1007/s00467-015-3138-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-015-3138-y