Abstract
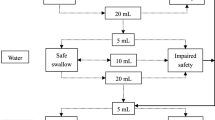
Thickeners are used in post-stroke oropharyngeal dysphagia (OD) as a compensatory therapeutic strategy against aspirations. To compare the therapeutic effects of modified starch (MS) and xanthan gum (XG) thickeners on swallow safety and efficacy in chronic post-stroke OD patients using clinical and videofluoroscopic (VFS) assessment. Patients were studied by clinical assessment (volume-viscosity swallow test, V-VST) and VFS using 3 volumes (5, 10, 20 mL) and 3 viscosities (liquid, nectar and spoon thick), comparing MS and XG. We studied 122 patients (46MS, 76XG). (A) V-VST showed that both thickeners similarly improved safety of swallow. Prevalence of safe swallowing significantly increased with enhanced viscosity (P < 0.001 vs liquid), MS: 47.83 % at liquid, 84.93 % at nectar and 92.96 % at spoon thick; XG: 55.31 % at liquid, 77.78 % at nectar and 97.84 % at spoon thick. Patients on MS reported higher prevalence of pharyngeal residue at spoon-thick viscosities. (B) VFS: increasing bolus viscosity with either thickener increased prevalence of safe swallows (P < 0.001 vs liquid), MS: 30.25 % liquid, 61.07 % nectar and 92.64 % spoon thick; XG: 29.12 % liquid, 71.30 % nectar and 89.91 % spoon thick. Penetration–aspiration scale score was significantly reduced with increased viscosity with both thickeners. MS increased oral and pharyngeal residues at nectar and spoon-thick viscosities but XG did not. Timing of airway protection mechanisms and bolus velocity were not affected by either thickener. Increasing bolus viscosity with MS and XG thickeners strongly and similarly improved safety of swallow in chronic post-stroke OD by a compensatory mechanism; in contrast only MS thickeners increased oropharyngeal residue.






Similar content being viewed by others
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30:744–8.
Rofes L, Arreola V, Romea M, Palomera E, Almirall J, Cabré M, Serra-Prat M, Clavé P. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol. Motil. 2010;22:851–8.
Clave P, de Kraa M, Arreola V, Girvent M, Farré R, Palomera E, Serra-Prat M. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24:1385–94.
Hilker R, Poetter C, Findeisen N, Sobesky J, Jacobs A, Neveling M, Heiss WD. Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine. Stroke. 2003;34:975–81.
Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U. Predictors of survival after severe dysphagic stroke. J Neurol. 2005;252:1510–6.
Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116:455–78.
Speyer R, Baijens L, Heijnen M, Zwijnenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25:40–65.
Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia. 2001;16:119–22.
Rofes L, Arreola V, Mukherjee R, Swanson J, Clave P. The effects of a xanthan gum-based thickener on the swallowing function of patients with dysphagia. Aliment Pharmacol Ther. 2014;39:1169–79.
Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG, Cook IJ, Lang IM. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990;258:G675–81.
Groher ME. Bolus management and aspiration pneumonia in patients with pseudobulbar dysphagia. Dysphagia. 1987;1:215–6.
Bhattacharyya N, Kotz T, Shapiro J. The effect of bolus consistency on dysphagia in unilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 2003;129:632–6.
Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, Coutts K, Dantas RO, Duivestein J, Giosa L, Hanson B, Lam P, Lecko C, Leigh C, Nagy A, Namasivayam AM, Nascimento WV, Odendaal I, Smith CH, Wang H. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30:2–26.
Matta Z, Chambers E, Garcia JM, Helverson JM. Sensory characteristics of beverages prepared with commercial thickeners used for dysphagia diets. J Am Diet Assoc. 2006;106:1049–54.
Garcia JM, Chambers E, Matta Z, Clark M. Viscosity measurements of nectar- and honey-thick liquids: product, liquid, and time comparisons. Dysphagia. 2005;20:325–35.
Cichero JA. Thickening agents used for dysphagia management: effect on bioavailability of water, medication and feelings of satiety. Nutr J. 2013;1(12):54.
Nita SP, Murith M, Chisholm H, Engmann J. Matching the rheological properties of videofluoroscopic contrast agents and thickened liquid prescriptions. Dysphagia. 2013;28:245–52.
Leonard RJ, White C, McKenzie S, Belafsky PC. Effects of bolus rheology on aspiration in patients with dysphagia. J Acad Nutr Diet. 2014;114:590–4.
Rofes L, Arreola V, Clavé P. The volume-viscosity swallow test for clinical screening of dysphagia and aspiration. Nestle Nutr Inst Workshop Ser. 2012;72:33–42.
Rosenbek J, Robbins J, Roecker E. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Clavé P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27:806–15.
The National Dysphagia Diet Task Force. National dysphagia diet: standardization for optimal care. Chicago: American Dietetic Association; 2002.
Dooley CP, Schlossmacher B, Valenzuela JE. Effects of alterations in bolus viscosity on esophageal peristalsis in humans. Am J Physiol. 1988;254:G8–11.
Lazarus CL, Logemann JA, Rademaker AW, Kahrilas PJ, Pajak T, Lazar R, Halper A. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Arch Phys Med Rehabil. 1993;74:1066–70.
Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL. Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Hear Res. 1994;37:1041–9.
Hind JA, Gensler G, Brandt DK, Gardner PJ, Blumenthal L, Gramigna GD, Kosek S, Lundy D, McGarvey-Toler S, Rockafellow S, Sullivan PA, Villa M, Gill GD, Lindblad AS, Logemann JA, Robbins J. Comparison of trained clinician ratings with expert ratings of aspiration on videofluoroscopic images from a randomized clinical trial. Dysphagia. 2009;24:211–7.
Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: how do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723–7.
Rofes L, Arreola V, Martin A, Clavé P. Natural capsaicinoids improve swallow response in older patients with oropharyngeal dysphagia. Gut. 2013;62:1280–7.
Hind J, Divyak E, Zielinski J, Taylor A, Hartman M, Gangnon R, Robbins J. Comparison of standardized bariums with varying rheological parameters on swallowing kinematics in males. J Rehabil Res Dev. 2012;49:1399–404.
Perlman AL, Booth BM, Grayhack JP. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia. 1994;9:90–5.
Aviv JE, Martin JH, Sacco RL, Zagar D, Diamond B, Keen MS, Blitzer A. Supraglottic and pharyngeal sensory abnormalities in stroke patients with dysphagia. Ann Otol Rhinol Laryngol. 1996;105:92–7.
Pelletier CA, Dhanaraj GE. The effect of taste and palatability on lingual swallowing pressure. Dysphagia. 2006;21:121–8.
Momosaki R, Abo M, Kobayashi K. Swallowing analysis for semisolid food texture in poststroke dysphagic patients. J Stroke Cerebrovasc Dis. 2013;22:267–70.
Leder SB, Judson BL, Sliwinski E, Madson L. Promoting safe swallowing when puree is swallowed without aspiration but thin liquid is aspirated: nectar is enough. Dysphagia. 2013;28:58–62.
Hamdy S, Jilani S, Price V, Parker C, Hall N, Power M. Modulation of human swallowing behaviour by thermal and chemical stimulation in health and after brain injury. Neurogastroenterol Motil. 2003;15:69–77.
Goulding R, Bakheit AM. Evaluation of the benefits of monitoring fluid thickness in the dietary management of dysphagic stroke patients. Clin Rehabil. 2000;14:119–24.
McGrail A, Kelchner LN. Adequate oral fluid intake in hospitalized stroke patients: does viscosity matter? Rehabil Nurs. 2012;37:252–7.
Ebihara T, Ebihara S, Watando A, Okazaki T, Asada M, Ohrui T, Yamaya M, Arai H. Effects of menthol on the triggering of the swallowing reflex in elderly patients with dysphagia. Br J Clin Pharmacol. 2006;62:369–71.
Ebihara T, Ebihara S, Maruyama M, Kobayashi M, Itou A, Arai H, Sasaki H. A randomized trial of olfactory stimulation using black pepper oil in older people with swallowing dysfunction. J Am Geriatr Soc. 2006;54:1401–6.
Rofes L, Arreola V, Martin A, Clavé P. Effect of oral piperine on the swallow response of patients with oropharyngeal dysphagia. J Gastroenterol. 2014;49:1517–23
Acknowledgments
We would like to thank our patients for their cooperation and all the members of the Dysphagia Team and the X-ray Department of the Hospital de Mataró, Nestlé Health Science and Nestlé Research Center who have participated in this study. We also thank Jane Lewis for English correction.
Funding
This study was supported by Grants from Fundació La Marató de TV3 and Nestlé Health Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The company that partially financed the study had no influence on or involvement in the results or the writing of the article.
Rights and permissions
About this article
Cite this article
Vilardell, N., Rofes, L., Arreola, V. et al. A Comparative Study Between Modified Starch and Xanthan Gum Thickeners in Post-Stroke Oropharyngeal Dysphagia. Dysphagia 31, 169–179 (2016). https://doi.org/10.1007/s00455-015-9672-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9672-8