Abstract
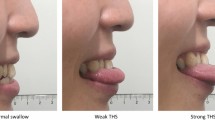
The aim of this prospective observational study was to determine the associations among age, maximum lingual isometric pressures, and maximum swallow pressures in specific regions of the tongue. Individuals 21 years and older who reported normal swallowing were enrolled. Seventy-one healthy adults were stratified by age into young (21–40 years), middle (41–60), and old (61–82) groups. Maximum pressures were measured for each individual during isometric tongue press tasks as well as saliva, 5, and 10 mL thin liquid bolus swallows at 5 sensors located on the hard palate: front, middle, left, right, and back. Lower maximum lingual pressures for all tasks were associated with increased age (p < 0.04). Saliva pressures exhibited a different pressure pattern than bolus swallows with pressures higher than bolus swallows on middle (p < 0.03) and back (p < 0.05) tongue sensors but not in the front. Diminished swallow pressure reserve (maximum isometric pressure–maximum swallow pressure) also was found with increased age (p < 0.03). Isometric pressures were greater than swallow pressures in young and middle age groups at both the front (p < 0.04) and back (p < 0.03) sensors, but only significantly greater at the front sensor for the oldest group (p < 0.04). Older healthy adults have lower lingual isometric pressures and lower swallow pressures than younger healthy adults. Elders have a decreased swallow pressure reserve to draw upon during occasions of physiological stress. While the exact mechanisms for age-related decline in lingual pressures remain unclear, they are likely due, at least in part, to sarcopenia. Saliva, 5, and 10 mL thin boluses also exhibit different age-related declines in pressure at specific sensors, indicating they may elicit different muscle activation patterns.




Similar content being viewed by others
References
Morris H. Dysphagia in the elderly- a management challenge for nurses. Br J Nurs. 2006;15(10):558–62.
Anderson M, Anzalone J, Holland L, Tracey E. Treatment of language, motor speech impairments, and Dysphagia, Continuum (Minneap Minn). Neurorehabilitation. 2011;17(3):471–93.
Park Y-H, Han H-R, Oh B-M, Lee J, Park J, Yu SJ, Chang H. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs. 2013;34(3):212–7.
Chen P-H, Golub JS, Hapner ER, Johns MM. Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia. 2009;24(1):1–6.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46.
Pikus L, Levine MS, Yang Y-X, Rubesin SE, Katzka DA, Laufer I, Gefter WB. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. AJR Am J Roentgenol. 2003;180(6):1613–6.
Sokoloff AJ. Activity of tongue muscles during respiration: it takes a village? J Appl Physiol. 2004;96(2):438–9.
Stål P, Marklund S, Thornell L-E, De Paul R, Eriksson P-O. Fibre composition of human intrinsic tongue muscles. Cells Tissues Organs. 2003;173(3):147–61.
von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle. 2010;1(2):129–33.
Evans WJ. What is sarcopenia? J Gerontol A Biol Sci Med Sci. 1995;50:5–8.
Buehring B, Hind J, Fidler E, Krueger D, Binkley N, Robbins J. Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc. 2013;61(3):418–22.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50(5):M257–62.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The Effects of Lingual Exercise on Swallowing in Older Adults. J Am Geriatr Soc. 2005;53(9):1483–9.
Youmans SR, Youmans GL, Stierwalt JAG. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24(1):57–65.
Crow HC, Ship JA. Tongue strength and endurance in different aged individuals. J Gerontol A Biol Sci Med Sci. 1996;51(5):M247–50.
Steele CM, Bailey GL, Molfenter SM. Tongue pressure modulation during swallowing: water versus nectar-thick liquids. J Speech Lang Hear Res. 2010;53(2):273–83.
Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103(3):823–9.
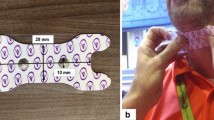
Robbins JA, Bomsztyk ED, Heppner AL, Koranda CL, Kroner AR, Kuchenreuther JM, Meister DM, Staerkel BS. Apparatus for measuring tongue/hard palate contact pressure. US6702765 B2. 2004.
Robbins JA, Hind JA, Hewitt AL. Oral-lever resistance exercise device. US7238145 B2. 2007.
IBM Corp. IBM SPSS statistics for windows. Armonk: IBM Corp.; 2013.
Lazarus CL, Logemann JA, Rademaker AW, Kahrilas PJ, Pajak T, Lazar R, Halper A. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Arch Phys Med Rehabil. 1993;74(10):1066–70.
Nicosia MA, Hind JA, Roecker EB, Carnes M, Doyle J, Dengel GA, Robbins J. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A Biol Sci Med Sci. 2000;55(11):M634–40.
Steele CM. Optimal approaches for measuring tongue-pressure functional reserve. J Aging Res. 2013;2013:542909.
Levine R, Robbins JA, Maser A. Periventricular white matter changes and oropharyngeal swallowing in normal individuals. Dysphagia. 1992;7(3):142–7.
Okada R, Okada T, Okada A, Muramoto H, Katsuno M, Sobue G, Hamajima N. Severe brain atrophy in the elderly as a risk factor for lower respiratory tract infection. Clin Interv Aging. 2012;7:481–7.
Birdsill AC, Koscik RL, Jonaitis EM, Johnson SC, Okonkwo OC, Hermann BP, Larue A, Sager MA, Bendlin BB. Regional white matter hyperintensities: aging, Alzheimer’s disease risk, and cognitive function. Neurobiol Aging. 2014;35(4):769–76.
Acknowledgments
The authors would like to thank Ronald Gangnon, PhD, for his guidance regarding statistical analysis for this manuscript. This article is the result of work supported by resources at the University of Wisconsin School of Medicine and Public Health (UW SMPH), the University of Wisconsin Department of Biomedical Engineering, and the William S. Middleton Memorial VA Hospital Geriatric Research Education and Clinical Center (GRECC), Madison, Wisconsin. The manuscript was prepared at the William S. Middleton Veteran Affairs Hospital in Madison, WI; GRECC manuscript #2015-016. The views and content expressed in this article are solely the responsibility of the authors and do not necessarily reflect the position, policy, or official views of the Department of Veteran Affairs or the U.S. government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
There are no relevant conflicts of interest to report for Nicole Rogus-Pulia, Naomi Humpal, or Kelsey Banaszynski. Jacqueline Hind is an employee of Swallow Solutions, LLC. JoAnne Robbins is inventor on patents administered through the Wisconsin Alumni Research Foundation, two of which have been licensed, one to Bracco Diagnostic Imaging and another to Swallow Solutions, LLC of which she is the founder.
Rights and permissions
About this article
Cite this article
Robbins, J., Humpal, N.S., Banaszynski, K. et al. Age-Related Differences in Pressures Generated During Isometric Presses and Swallows by Healthy Adults. Dysphagia 31, 90–96 (2016). https://doi.org/10.1007/s00455-015-9662-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9662-x