Abstract
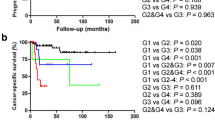
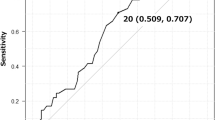
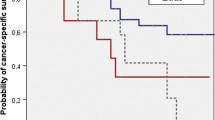
The purposes of this study are to evaluate the adequacy of pathologic lymph node (LN) staging in radical cystectomy specimens from patients with urothelial carcinoma of the bladder and to analyze the frequency of LN metastases among different anatomic regions. All radical cystectomies performed for primary urothelial bladder cancer over a 5-year period (January 2007–September 2012) at a single institution were reviewed. Particular attention was paid to the total number of LNs examined, the number and location of LNs with metastases (positive LNs), and the presence or absence of extranodal tumor extension and/or lymphovascular invasion in the cystectomy specimen. Results and data were analyzed with Origin 6.0 and Microsoft Office Excel 2007 software. A total of 248 radical cystectomies with 8,432 LNs were reviewed. A total of 60 (24 %) cases, with 274 positive LNs out of the 1,982 total (13.8 %), were identified with a male to female ratio of 6.5:1 (52 male, 8 female patients). The average number of LNs examined in each case was 33.0 ± 20.9 (range 5–112). The average number of positive LNs identified in each case was 4.5 ± 4.8 (range 1–26). Among all of the LNs, the hypogastric/obturator (internal iliac) LNs were the most commonly submitted (35.2 %) and also yielded the highest number of positive LNs (46.0 %). On average, for cases staged pN1 and pN2, there was one positive LN per 17.8 and 8.9 LNs examined from the primary drainage LNs, respectively. For pN3 cases, one out of 4.4 secondary drainage LNs was found to be positive. Similarly, one out of 4.0 distant LNs was found to be positive in cases with pM1 staging. Our study suggests that, on average, 23 LNs (including 18 primary drainage LNs and five secondary drainage LNs) should be submitted for optimal pN staging. For adequate pM1 staging, an average of four distal LNs should be evaluated. In total, an average of 27 LNs (23 for pN staging and 4 for pM staging) should be examined in radical cystectomy specimens. We also propose to stratify the number of positive LNs according to the drainage area.






Similar content being viewed by others
References
Leissner J, Ghoneim MA, Abol-Enein H et al (2004) Extended radical lymphadenectomy in patients with urothelial bladder cancer: results of a prospective multicenter study. J Urol 171(1):139–144
Abaza R, Dangle PP, Gong MC, Bahnson RR, Pohar KS (2012) Quality of lymphadenectomy is equivalent with robotic and open cystectomy using an extended template. J Urol 187(4):1200–1204
Dangle PP, Bahnson RR, Pohar KS (2009) How close are we to establishing standards of lymphadenectomy for invasive bladder cancer? Ther Adv Urol 1(3):167–174
Dhar NB, Klein EA, Reuther AM, Thalmann GN, Madersbacher S, Studer UE (2008) Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. J Urol 179(3):873–878, discussion 878
Dangle PP, Gong MC, Bahnson RR, Pohar KS (2010) How do commonly performed lymphadenectomy templates influence bladder cancer nodal stage? J Urol 183(2):499–503
Bochner BH, Herr HW, Reuter VE (2001) Impact of separate versus en bloc pelvic lymph node dissection on the number of lymph nodes retrieved in cystectomy specimens. J Urol 166(6):2295–2296
Herr HW (2003) Superiority of ratio based lymph node staging for bladder cancer. J Urol 169(3):943–945
Stein JP, Cai J, Groshen S, Skinner DG (2003) Risk factors for patients with pelvic lymph node metastases following radical cystectomy with en bloc pelvic lymphadenectomy: concept of lymph node density. J Urol 170(1):35–41
Lee EK, Herr HW, Dickstein RJ et al (2012) Lymph node density for patient counselling about prognosis and for designing clinical trials of adjuvant therapies after radical cystectomy. BJU Int 110(11 Pt B):E590–E595
Masson-Lecomte A, Vordos D, Hoznek A et al (2013) External validation of extranodal extension and lymph node density as predictors of survival in node-positive bladder cancer after radical cystectomy. Ann Surg Oncol 20(4):1389–1394
Quek ML, Flanigan RC (2009) The role of lymph node density in bladder cancer prognostication. World J Urol 27(1):27–32
Herr HW (2010) Extent of pelvic lymph node dissection during radical cystectomy: where and why! Eur Urol 57(2):212–213
Karl A, Carroll PR, Gschwend JE et al (2009) The impact of lymphadenectomy and lymph node metastasis on the outcomes of radical cystectomy for bladder cancer. Eur Urol 55(4):826–835
Herr HW, Faulkner JR, Grossman HB et al (2004) Surgical factors influence bladder cancer outcomes: a cooperative group report. J Clin Oncol 22(14):2781–2789
Konety BR, Joslyn SA, O’Donnell MA (2003) Extent of pelvic lymphadenectomy and its impact on outcome in patients diagnosed with bladder cancer: analysis of data from the Surveillance, Epidemiology and End Results Program data base. J Urol 169(3):946–950
Capitanio U, Suardi N, Shariat SF et al (2009) Assessing the minimum number of lymph nodes needed at radical cystectomy in patients with bladder cancer. BJU Int 103(10):1359–1362
Shariat SF, Rink M, Ehdaie B et al (2013) Pathologic nodal staging score for bladder cancer: a decision tool for adjuvant therapy after radical cystectomy. Eur Urol 63(2):371–378
Koppie TM, Vickers AJ, Vora K, Dalbagni G, Bochner BH (2006) Standardization of pelvic lymphadenectomy performed at radical cystectomy: can we establish a minimum number of lymph nodes that should be removed? Cancer 107(10):2368–2374
Davies JD, Simons CM, Ruhotina N, Barocas DA, Clark PE, Morgan TM (2013) Anatomic basis for lymph node counts as measure of lymph node dissection extent: a cadaveric study. Urology 81(2):358–363
Edge SBBD, Compton CC, Fritz AG, Greene FL, Trotti A (2010) AJCC Cancer Staging Manual 7th Edition, 7th edn. Springer, Chicago
Stein JP, Lieskovsky G, Cote R et al (2001) Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol 19(3):666–675
Bruins HM, Stein JP (2008) Risk factors and clinical outcomes of patients with node-positive muscle-invasive bladder cancer. Expert Rev Anticancer Ther 8(7):1091–1101
Leadbetter WF, Cooper JF (1950) Regional gland dissection for carcinoma of the bladder; a technique for one-stage cystectomy, gland dissection, and bilateral uretero-enterostomy. J Urol 63(2):242–260
Tarin TV, Power NE, Ehdaie B et al (2012) Lymph node-positive bladder cancer treated with radical cystectomy and lymphadenectomy: effect of the level of node positivity. Eur Urol 61(5):1025–1030
Abol-Enein H, El-Baz M, Abd El-Hameed MA, Abdel-Latif M, Ghoneim MA (2004) Lymph node involvement in patients with bladder cancer treated with radical cystectomy: a patho-anatomical study—a single center experience. J Urol 172(5 Pt 1):1818–1821
Vazina A, Dugi D, Shariat SF, Evans J, Link R, Lerner SP (2004) Stage specific lymph node metastasis mapping in radical cystectomy specimens. J Urol 171(5):1830–1834
Dorin RP, Daneshmand S, Eisenberg MS et al (2011) Lymph node dissection technique is more important than lymph node count in identifying nodal metastases in radical cystectomy patients: a comparative mapping study. Eur Urol 60(5):946–952
Kassouf W, Svatek RS, Shariat SF et al (2013) Critical analysis and validation of lymph node density as prognostic variable in urothelial carcinoma of bladder. Urol Oncol 31(4):480–486
May M, Herrmann E, Bolenz C et al (2011) Lymph node density affects cancer-specific survival in patients with lymph node-positive urothelial bladder cancer following radical cystectomy. Eur Urol 59(5):712–718
Wright JL, Lin DW, Porter MP (2008) The association between extent of lymphadenectomy and survival among patients with lymph node metastases undergoing radical cystectomy. Cancer 112(11):2401–2408
Kassouf W, Agarwal PK, Herr HW et al (2008) Lymph node density is superior to TNM nodal status in predicting disease-specific survival after radical cystectomy for bladder cancer: analysis of pooled data from MDACC and MSKCC. J Clin Oncol 26(1):121–126
Leissner J, Hohenfellner R, Thuroff JW, Wolf HK (2000) Lymphadenectomy in patients with transitional cell carcinoma of the urinary bladder; significance for staging and prognosis. BJU Int 85(7):817–823
Herr HW, Bochner BH, Dalbagni G, Donat SM, Reuter VE, Bajorin DF (2002) Impact of the number of lymph nodes retrieved on outcome in patients with muscle invasive bladder cancer. J Urol 167(3):1295–1298
CAP Cancer Protocols and Checklists: Protocol for the examination of specimens from patients with carcinoma of the urinary bladder. College of American Pathologists 2013. http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2013/UrinaryBladder_13protocol_3210.pdf. Accessed Oct. 2013.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, L., Mudaliar, K., Mehta, V. et al. Seeking a standard for adequate pathologic lymph node staging in primary bladder carcinoma. Virchows Arch 464, 595–602 (2014). https://doi.org/10.1007/s00428-014-1575-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-014-1575-9