Abstract
Purpose
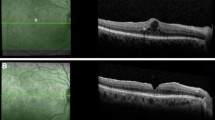
LR11 (also called SorLA or SORL1) is a migration regulator of adherent cells with the immature proliferative phenotype. The present study investigated the clinical and pathological involvement of the soluble form of LR11 (sLR11) in the idiopathic epiretinal membrane (iERM).
Methods
The subjects were 51 patients with iERM (24 cellophane macular reflex (CMR) and 27 preretinal macular fibrosis (PMF)) and 45 patients with macular holes as age and sex-matched controls. Vitreous sLR11 and transforming growth factor (TGF)β2 levels were measured by ELISA.
Results
The sLR11 levels in the vitreous fluids of patients with iERM (20.2 ± 8.1 ng/mL) were significantly higher than those in controls (11.4 ± 4.7 ng/mL). Among the patients with iERM, the vitreous sLR11 levels were significantly higher in PMF (23.6 ± 8.2 ng/mL), than those in CMR (16.5 ± 5.9 ng/mL). Multivariate regression analysis of the studied factors showed that sLR11 was a unique factor independently contributing to the discrimination of the iERM patients against the control subjects (odds ratio [OR] 1.35 per 1-ng/mL increase, 95% CI 1.09–1.67; P = 0.004). ROC analysis showed that the sensitivity and the specificity of sLR11, but not of other studied factors, categorized into the rank of moderate accuracy. Finally, there was a positive correlation (R = 0.588; P = 0.003) between the vitreous levels of sLR11 and TGFβ2 using the available samples.
Conclusions
sLR11 levels in vitreous fluids were specifically increased in patients with iERM, suggesting the involvement in the pathology of proliferative and migrating cells for the development of iERM.


Similar content being viewed by others
References
McLeod D, Hiscott PS, Grierson I (1987) Age-related cellular proliferation at the vitreoretinal juncture. Eye (Lond) 1(Pt 2):263–281. doi:10.1038/eye.1987.46
Foos RY (1977) Vitreoretinal juncture; epiretinal membranes and vitreous. Invest Ophthalmol Vis Sci 16:416–422
Smiddy WE, Maguire AM, Green WR, Michels RG, de la Cruz Z, Enger C, Jaeger M, Rice TA (1989) Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology 96:811–820, discussion 821
Sivalingam A, Kenney J, Brown GC, Benson WE, Donoso L (1990) Basic fibroblast growth factor levels in the vitreous of patients with proliferative diabetic retinopathy. Arch Ophthalmol 108:869–872
Harada C, Mitamura Y, Harada T (2006) The role of cytokines and trophic factors in epiretinal membranes: involvement of signal transduction in glial cells. Prog Retin Eye Res 25:149–164. doi:10.1016/j.preteyeres.2005.09.001
Campochiaro PA, Glaser BM (1985) Endothelial cells release a chemoattractant for retinal pigment epithelial cells in vitro. Arch Ophthalmol 103:1876–1880
Iannetti L, Accorinti M, Malagola R, Bozzoni-Pantaleoni F, Da Dalt S, Nicoletti F, Gradini R, Traficante A, Campanella M, Pivetti-Pezzi P (2011) Role of the intravitreal growth factors in the pathogenesis of idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 52:5786–5789. doi:10.1167/iovs.10-7116
Vinores SA, Henderer JD, Mahlow J, Chiu C, Derevjanik NL, Larochelle W, Csaky C, Campochiaro PA (1995) Isoforms of platelet-derived growth factor and its receptors in epiretinal membranes: immunolocalization to retinal pigmented epithelial cells. Exp Eye Res 60:607–619
Frank RN, Amin RH, Eliott D, Puklin JE, Abrams GW (1996) Basic fibroblast growth factor and vascular endothelial growth factor are present in epiretinal and choroidal neovascular membranes. Am J Ophthalmol 122:393–403
Jiang M, Bujo H, Ohwaki K, Unoki H, Yamazaki H, Kanaki T, Shibasaki M, Azuma K, Harigaya K, Schneider WJ, Saito Y (2008) Ang II-stimulated migration of vascular smooth muscle cells is dependent on LR11 in mice. J Clin Invest 118:2733–2746. doi:10.1172/jci32381
Matsuo M, Ebinuma H, Fukamachi I, Jiang M, Bujo H, Saito Y (2009) Development of an immunoassay for the quantification of soluble LR11, a circulating marker of atherosclerosis. Clin Chem 55:1801–1808. doi:10.1373/clinchem.2009.127027
Takahashi M, Bujo H, Shiba T, Jiang M, Maeno T, Shirai K (2012) Enhanced circulating soluble LR11 in patients with diabetic retinopathy. Am J Ophthalmol 154:187–192. doi:10.1016/j.ajo.2012.01.035
Ogita M, Miyauchi K, Jiang M, Kasai T, Tsuboi S, Naito R, Konishi H, Dohi T, Yokoyama T, Okazaki S, Shimada K, Bujo H, Daida H (2014) Circulating soluble LR11, a novel marker of smooth muscle cell proliferation, is enhanced after coronary stenting in response to vascular injury. Atherosclerosis 237:374–378. doi:10.1016/j.atherosclerosis.2014.08.044
Ogita M, Miyauchi K, Kasai T, Tsuboi S, Wada H, Naito R, Konishi H, Dohi T, Tamura H, Okazaki S, Yanagisawa N, Shimada K, Suwa S, Jiang M, Bujo H, Daida H (2016) Prognostic impact of circulating soluble LR11 on long-term clinical outcomes in patients with coronary artery disease. Atherosclerosis 244:216–221. doi:10.1016/j.atherosclerosis.2015.11.004
Jin W, Jiang M, Han X, Han X, Murano T, Hiruta N, Ebinuma H, Piao L, Schneider WJ, Bujo H (2016) Circulating soluble form of LR11, a regulator of smooth muscle cell migration, is a novel marker for intima-media thickness of carotid arteries in type 2 diabetes. Clin Chim Acta 457:137–141. doi:10.1016/j.cca.2016.04.016
Shiba T, Bujo H, Takahashi M, Sato Y, Jiang M, Hori Y, Maeno T, Shirai K (2013) Vitreous fluid and circulating levels of soluble lr11, a novel marker for progression of diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 251:2689–2695. doi:10.1007/s00417-013-2373-9
Mitchell P, Smith W, Chey T, Wang JJ, Chang A (1997) Prevalence and associations of epiretinal membranes. Ophthalmology 104:1033–1040. doi:10.1016/s0161-6420(97)30190-0
Ng CH, Cheung N, Wang JJ, Islam AF, Kawasaki R, Meuer SM, Cotch MF, Klein BE, Klein R, Wong TY (2011) Prevalence and risk factors for epiretinal membranes in a multi-ethnic United States population. Ophthalmology 118:694–699. doi:10.1016/j.ophtha.2010.08.009
Nohara A, Kobayashi J, Kawashiri MA, Tada H, Inazu A, Jiang M, Mabuchi H, Bujo H (2014) Clinical significance of measuring soluble LR11, a circulating marker of atherosclerosis and HbA1c in familial hypercholesterolemia. Clin Biochem 47:1326–1328. doi:10.1016/j.clinbiochem.2014.05.003
Miyazaki M, Nakamura H, Kubo M, Kiyohara Y, Iida M, Ishibashi T, Nose Y (2003) Prevalence and risk factors for epiretinal membranes in a Japanese population: the Hisayama study. Graefes Arch Clin Exp Ophthalmol 241:642–646. doi:10.1007/s00417-003-0723-8
Kawasaki R, Wang JJ, Sato H, Mitchell P, Kato T, Kawata S, Kayama T, Yamashita H, Wong TY (2009) Prevalence and associations of epiretinal membranes in an adult Japanese population: the Funagata study. Eye (Lond) 23:1045–1051. doi:10.1038/eye.2008.238
Whittle AJ, Jiang M, Peirce V, Relat J, Virtue S, Ebinuma H, Fukamachi I, Yamaguchi T, Takahashi M, Murano T, Tatsuno I, Takeuchi M, Nakaseko C, Jin W, Jin Z, Campbell M, Schneider WJ, Vidal-Puig A, Bujo H (2015) Soluble LR11/SorLA represses thermogenesis in adipose tissue and correlates with BMI in humans. Nat Commun 6:8951. doi:10.1038/ncomms9951
Bellhorn MB, Friedman AH, Wise GN, Henkind P (1975) Ultrastructure and clinicopathologic correlation of idiopathic preretinal macular fibrosis. Am J Ophthalmol 79:366–373
Kishi S (2016) Vitreous anatomy and the vitreomacular correlation. Jpn J Ophthalmol 60:239–273. doi:10.1007/s10384-016-0447-z
Heldin CH, Westermark B (1999) Mechanism of action and in vivo role of platelet-derived growth factor. Physiol Rev 79:1283–1316
Okada M, Ogino N, Matsumura M, Honda Y, Nagai Y (1995) Histological and immunohistochemical study of idiopathic epiretinal membrane. Ophthalmic Res 27:118–128
Kawahara S, Hata Y, Kita T, Arita R, Miura M, Nakao S, Mochizuki Y, Enaida H, Kagimoto T, Goto Y, Hafezi-Moghadam A, Ishibashi T (2008) Potent inhibition of cicatricial contraction in proliferative vitreoretinal diseases by statins. Diabetes 57:2784–2793. doi:10.2337/db08-0302
Minchiotti S, Stampachiacchiere B, Micera A, Lambiase A, Ripandelli G, Billi B, Bonini S (2008) Human idiopathic epiretinal membranes express NGF and NGF receptors. Retina 28:628–637. doi:10.1097/IAE.0b013e31815ec275
Guidry C (1997) Tractional force generation by porcine Muller cells. Development and differential stimulation by growth factors. Invest Ophthalmol Vis Sci 38:456–468
Bu SC, Kuijer R, van der Worp RJ, Postma G, Renardel de Lavalette VW, Li XR, Hooymans JM, Los LI (2015) Immunohistochemical evaluation of idiopathic epiretinal membranes and in vitro studies on the effect of TGF-beta on Muller cells. Invest Ophthalmol Vis Sci 56:6506–6514. doi:10.1167/iovs.14-15971
Kritzenberger M, Junglas B, Framme C, Helbig H, Gabel VP, Fuchshofer R, Tamm ER, Hillenkamp J (2011) Different collagen types define two types of idiopathic epiretinal membranes. Histopathology 58:953–965. doi:10.1111/j.1365-2559.2011.03820.x
George B, Chen S, Chaudhary V, Gonder J, Chakrabarti S (2009) Extracellular matrix proteins in epiretinal membranes and in diabetic retinopathy. Curr Eye Res 34:134–144. doi:10.1080/02713680802585946
Kohno RI, Hata Y, Kawahara S, Kita T, Arita R, Mochizuki Y, Aiello LP, Ishibashi T (2009) Possible contribution of hyalocytes to idiopathic epiretinal membrane formation and its contraction. Br J Ophthalmol 93:1020–1026. doi:10.1136/bjo.2008.155069
Acknowledgements
Design and conduct study: R.H. and H.B. Collection: R.H., T.S. and T.M.; management, analysis, and interpretation of the data: R.H., M.J., N.H., M.T., M.H., Y.H. and H.B.; and preparation, review, or approval of the manuscript: R.H., M.J., T.S., N.H., M.T., M.H., Y.H., H.B. and T.M. We had no statistical consultation or assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the institutional review board of Toho University Sakura Medical Center (No.S16036) and with the 1964 Helsinki Declaration. Informed consent was obtained from all individual participants included in the study.
Funding
This study was supported, in part, by Grants-in–aid for Scientific Research to Hideaki Bujo (24390231 and 15 K15198) and Meizi Jiang (24790907), and by a supported program for the Strategic Research Foundation at Private Universities (S1411015) from Japanese Ministry of Education, Culture, Sports, Science and Technology. This study was also supported by Japan Health and Labour Sciences Research Grant to Hideaki Bujo (H22-rinkensui-ippan-001), and by the Toho University Research Fund to Ryuya Hashimoto.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speaker’s bureaus; membership, employment, consultancies, stock ownership).
Rights and permissions
About this article
Cite this article
Hashimoto, R., Jiang, M., Shiba, T. et al. Soluble form of LR11 is highly increased in the vitreous fluids of patients with idiopathic epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 255, 885–891 (2017). https://doi.org/10.1007/s00417-017-3585-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3585-1