Abstract
Purpose
To compare the antibiotic susceptibilities and visual acuity (VA) outcomes in endophthalmitis caused by methicillin-resistant (MRSA) versus methicillin-sensitive S. aureus (MSSA).
Methods
The records of 34 cases of S. aureus endophthalmitis at The New York Eye and Ear Infirmary from Jan 1997 to June 2011 were reviewed. Antibiotic susceptibility profiles over time and VA at presentation and at 3, 6, and ≥12 months were recorded. S. aureus isolates were grouped based on oxacillin resistance.
Results
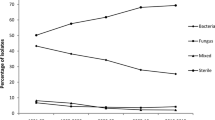
Of the 34 cases, 15 (44 %) were MRSA and 19 (56 %) MSSA. Median presenting VA was hand motions (logMAR 4.0) in both the MRSA and MSSA groups. There was no statistically significant difference in VA between the MRSA and MSSA groups at 3, 6, or ≥12 months. No MRSA isolates were resistant to vancomycin or gentamicin. While over 85 % of MRSA isolates tested for fourth-generation fluoroquinolones were resistant, just 10 % MSSA isolates tested were resistant. There was a trend suggesting an increase in the proportion of MRSA isolates compared to MSSA isolates over the course of the study period.
Conclusions
There was no statistical difference in short- or long-term VA outcomes between the MRSA and MSSA groups at any time point. Resistance to fourth-generation fluoroquinolones was present in over 85 % of MRSA isolates, but just 10 % of MSSA isolates. An increasing proportion of MRSA amongst S. aureus isolates was noted over the course of the study period.


Similar content being viewed by others
References
Major JC Jr, Engelbert M, Flynn HW Jr, Miller D, Smiddy WE, Davis J (2010) Staphylococcus aureus endophthalmitis: antibiotic susceptibilities, methicillin resistance, and clinical outcomes. Am J Ophthalmol 149(2):278.e271–283.e271. doi:10.1016/j.ajo.2009.08.023
Miller JJ, Scott IU, Flynn HW Jr, Smiddy WE, Newton J, Miller D (2005) Acute-onset endophthalmitis after cataract surgery (2000-2004): incidence, clinical settings, and visual acuity outcomes after treatment. Am J Ophthalmol 139(6):983–987. doi:10.1016/j.ajo.2005.01.025
Artunay O, Yuzbasioglu E, Rasier R, Sengul A, Bahcecioglu H (2009) Incidence and management of acute endophthalmitis after intravitreal bevacizumab (Avastin) injection. Eye (London, England) 23(12):2187–2193. doi:10.1038/eye.2009.7
Lyall DA, Tey A, Foot B, Roxburgh ST, Virdi M, Robertson C, MacEwen CJ (2012) Post-intravitreal anti-VEGF endophthalmitis in the United Kingdom: incidence, features, risk factors, and outcomes. Eye (London) 26(12):1517–1526. doi:10.1038/eye.2012.199
Shah CP, Garg SJ, Vander JF, Brown GC, Kaiser RS, Haller JA (2011) Outcomes and risk factors associated with endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmology 118(10):2028–2034. doi:10.1016/j.ophtha.2011.02.034
Ho V, Ho LY, Ranchod TM, Drenser KA, Williams GA, Garretson BR (2011) Endogenous methicillin-resistant Staphylococcus aureus endophthalmitis. Retina 31(3):596–601. doi:10.1097/IAE.0b013e3181ecccf0
Melo GB, Bispo PJ, Yu MC, Pignatari AC, Hofling-Lima AL (2011) Microbial profile and antibiotic susceptibility of culture-positive bacterial endophthalmitis. Eye (London) 25(3):382–387. doi:10.1038/eye.2010.236, quiz 388
Chambers HF (2005) Community-associated MRSA--resistance and virulence converge. N Engl J Med 352(14):1485–1487. doi:10.1056/NEJMe058023
Heilmann C (2011) Adhesion mechanisms of staphylococci. Adv Exp Med Biol 715:105–123. doi:10.1007/978-94-007-0940-9_7
Watkins RR, David MZ, Salata RA (2012) Current concepts on the virulence mechanisms of meticillin-resistant Staphylococcus aureus. J Med Microbiol 61(Pt 9):1179–1193. doi:10.1099/jmm.0.043513-0
Malachowa N, DeLeo FR (2010) Mobile genetic elements of Staphylococcus aureus. Cell Mol Life Sci 67(18):3057–3071. doi:10.1007/s00018-010-0389-4
Gillet Y, Issartel B, Vanhems P, Fournet JC, Lina G, Bes M, Vandenesch F, Piemont Y, Brousse N, Floret D, Etienne J (2002) Association between Staphylococcus aureus strains carrying gene for Panton–Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359(9308):753–759. doi:10.1016/s0140-6736(02)07877-7
Gonzalez BE, Martinez-Aguilar G, Hulten KG, Hammerman WA, Coss-Bu J, Avalos-Mishaan A, Mason EO Jr, Kaplan SL (2005) Severe Staphylococcal sepsis in adolescents in the era of community-acquired methicillin-resistant Staphylococcus aureus. Pediatrics 115(3):642–648. doi:10.1542/peds.2004-2300
Miller LG, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer AS, Tang AW, Phung TO, Spellberg B (2005) Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med 352(14):1445–1453. doi:10.1056/NEJMoa042683
Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo GR, Heffernan H, Liassine N, Bes M, Greenland T, Reverdy ME, Etienne J (2003) Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton–Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis 9(8):978–984. doi:10.3201/eid0908.030089
Han DP, Wisniewski SR, Wilson LA, Barza M, Vine AK, Doft BH, Kelsey SF (1996) Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol 122(1):1–17
Calfee DP (2011) The epidemiology, treatment, and prevention of transmission of methicillin-resistant Staphylococcus aureus. J Infus Nurs 34(6):359–364. doi:10.1097/NAN.0b013e31823061d6
No Authors Listed (1996) Microbiologic factors and visual outcome in the endophthalmitis vitrectomy study. Am J Ophthalmol 122(6):830–846
Chang DF, Braga-Mele R, Henderson BA, Mamalis N, Vasavada A (2015) Antibiotic prophylaxis of postoperative endophthalmitis after cataract surgery: results of the 2014 ASCRS member survey. J Cataract Refract Surg 41(6):1300–1305. doi:10.1016/j.jcrs.2015.01.014
Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW (2006) ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: preliminary report of principal results from a European multicenter study. J Cataract Refract Surg 32(3):407–410. doi:10.1016/j.jcrs.2006.02.021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was supported by The Macula Foundation, Inc.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Huz, J.I., Mukkamala, K., Pagan, I.R. et al. Clinical outcomes and antibiotic susceptibilities of Staphylococcus aureus endophthalmitis. Graefes Arch Clin Exp Ophthalmol 255, 651–656 (2017). https://doi.org/10.1007/s00417-016-3504-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3504-x