Abstract
Purpose
To determine the relationship between prelaminar structural changes of the optic nerve head (ONH) and optic nerve waxy pallor in retinitis pigmentosa (RP) using spectral-domain optical coherence tomography (SD-OCT) and fundus photography.
Methods
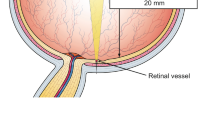
An observational cross-sectional case control study of patients with RP with and without ONH waxy pallor and controls. Subjects underwent clinical examination, fundus photography, and SD-OCT raster imaging of the ONH. Four independent specialists reviewed the images in a masked fashion.
Results
Fifty-five eyes of 31 subjects with RP and 28 eyes of 14 controls were included. Optic nerve head waxy pallor was seen in 29 RP eyes (52.7 %) and none in controls. SD-OCT showed a hyper-reflective structure suggestive of a glial membrane-like structure on the surface of ONH in 16 of RP eyes (55.1 %). In the RP group, there was a significant positive correlation between the ONH pallor and the presence of a prelaminar structure (p = 0.006).
Conclusions
There is a presence of glial membrane-like structures on the optic nerve head surface in eyes with RP compared to healthy eyes. As the presence of glial membranes correlated with the presence of ONH waxy pallor, in such cases these membranes might be responsible for ONH waxy pallor.



Similar content being viewed by others
References
Berson EL (1993) Retinitis pigmentosa. The Friedenwald Lecture. Invest Ophthalmol Vis Sci 34:1659–1676
Hartong DT, Berson EL, Dryja TP (2006) Retinitis pigmentosa. Lancet 368:1795–1809
Bhatti MT (2006) Retinitis pigmentosa, pigmentary retinopathies, and neurologic diseases. Curr Neurol Neurosci Rep 6(5):403–13
Lee SH, Yu HG, Seo JM et al (2010) Hereditary and clinical features of retinitis pigmentosa in Koreans. J Korean Med Sci 25(6):918–923
Szamier RB (1981) Ultrastructure of the preretinal membrane in retinitis pigmentosa. Invest Ophthalmol Vis Sci 21(2):227–236
Milam AH, Li ZY, Fariss RN (1998) Histopathology of the human retina in retinitis pigmentosa. Prog Retin Eye Res 17:175–205
Goldberg MF, Lee FL, Tso MO, Fishman GA (1989) Histopathologic study of autosomal dominant vitreoretinochoroidopathy. Peripheral annular pigmentary dystrophy of the retina. Ophthalmology 96(12):1736–46
Hwang YH, Kim SW, Kim YY et al (2012) Optic nerve head, retinal nerve fiber layer, and macular thickness measurements in young patients with retinitis pigmentosa. Curr Eye Res 37(10):914–20
Pruett RC (1983) Retinitis pigmentosa: clinical observations and correlations. Trans Am Ophthalmol Soc 81:693–735
Garcia-Martin E, Pinilla I, Sancho E et al (2012) Optical coherence tomography in retinitis pigmentosa: reproducibility and capacity to detect macular and retinal nerve fiber layer thickness alterations. Retina 32(8):1581–91
Oishi A, Otani A, Sasahara M et al (2009) Retinal nerve fiber layer thickness in patients with retinitis pigmentosa. Eye (Lond) 23:561–566
Anastasakis A, Genead MA, McAnany JJ, Fishman GA (2012) Evaluation of retinal nerve fiber layer thickness in patients with retinitis pigmentosa using spectral-domain optical coherence tomography. Retina 32:358–363
Sung KR, Wollstein G, Bilonick RA et al (2009) Effects of age on optical coherence tomography measurements of healthy retinal nerve fiber layer, macula, and optic nerve head. Ophthalmology 116:1119–1124
Roth AM, Foos RY (1972) Surface structure of the optic nerve head. 1. Epipapillary membranes. Am J Ophthalmol 74(5):977–85
Conflict of Interest Statement
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al Rashaed, S., Khan, A.O., Nowilaty, S.R. et al. Spectral-domain optical coherence tomography reveals prelaminar membranes in optic nerve head pallor in eyes with retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol 254, 77–81 (2016). https://doi.org/10.1007/s00417-015-3015-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3015-1