Abstract
Introduction
Radiation protection is becoming more important with an ongoing increase in radiation exposure due to the use of X-rays in minimally invasive procedures in orthopaedic and trauma surgeries. However, sufficient education in medical physics and radiation protection can often be improved.
Materials and methods
A questionnaire consisting of four questions about personal data and ten questions about radiation protection was distributed to lead consultants, consultants, residents, medical students, and medical technical assistants at two institutions, a level 1 trauma center and a children’s hospital.
Results
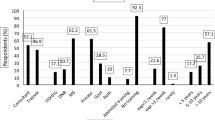
This study consisted of 83 participants. The compliance with radiation protection, i.e., usage of a dosimetry, an apron, and a thyroid shield on a regular basis was only seen in 54 %. Participants from the trauma center wore a dosimeter and thyroid shield significantly more often. The regular use of a thyroid shield differed significantly between job positions. It was observed in 80 % of students, but only 15 % of technical assistants. Only 65 % of all knowledge questions were answered correctly. There was a discrepancy between incorrectly answered knowledge questions (35 %) and those marked as uncertain (20 %). Different job positions did not have an impact on the answers to the questions in most instances.
Conclusions
The compliance with and the knowledge about radiation protection seems to be unnecessarily low in trauma physicians and technical assistants. The discrepancy in falsely answered questions and those marked as uncertain may suggest that participants may overestimate their knowledge about radiation protection, which is potentially harmful due to the increased radiation exposure. Therefore, we advocate a quick and valuable training of trauma surgeons and medical staff addressing the important preventive measures, some of which are illustrated in the present study. These consist of wearing dosimetry and protection devices, reduction in X-ray duration, preferably antero-posterior C-arm positioning with the image intensifier close to the patient and the surgeon, maximal distance, collimation, and increased voltage. Furthermore, the use of visual feedback on complex and potentially hazardous radiation facts may be useful for training purposes.
Study design
Cross-sectional study with a questionnaire.






Similar content being viewed by others
References
Singer G (2005) Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg 13(1):69–76
Theocharopoulos N, Perisinakis K, Damilakis J, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N (2003) Occupational exposure from common fluoroscopic projections used in orthopaedic surgery. J Bone Joint Surg Am 85-A(9):1698–1703
Oddy MJ, Aldam CH (2006) Ionising radiation exposure to orthopaedic trainees: the effect of sub-specialty training. Ann R Coll Surg Engl 88(3):297–301. doi:10.1308/003588406X98702
Maruthainar N, Bentley G, Williams A, Danin JC (2003) Availability of thyroid protective lead shields and their use by trainee orthopaedic surgeons. Occup Environ Med 60(5):381
Röntgen KW (1895) Über eine neue Art von Strahlen. Phys Med Gesellsch 9:132–141
Uzoigwe CE, Middleton RG (2012) Occupational radiation exposure and pregnancy in orthopaedics. J Bone Joint Surg Br 94(1):23–27. doi:10.1302/0301-620X.94B1.27689
Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, Howe G, Kaldor J, Muirhead CR, Schubauer-Berigan M, Yoshimura T, Bermann F, Cowper G, Fix J, Hacker C, Heinmiller B, Marshall M, Thierry-Chef I, Utterback D, Ahn YO, Amoros E, Ashmore P, Auvinen A, Bae JM, Bernar J, Biau A, Combalot E, Deboodt P, Diez Sacristan A, Eklöf M, Engels H, Engholm G, Gulis G, Habib RR, Holan K, Hyvonen H, Kerekes A, Kurtinaitis J, Malker H, Martuzzi M, Mastauskas A, Monnet A, Moser M, Pearce MS, Richardson DB, Rodriguez-Artalejo F, Rogel A, Tardy H, Telle-Lamberton M, Turai I, Usel M, Veress K (2007) The 15-Country Collaborative Study of Cancer Risk among Radiation Workers in the Nuclear Industry: estimates of radiation-related cancer risks. Radiat Res 167(4):396–416. doi:10.1667/RR0553.1
Herscovici D, Sanders RW (2000) The effects, risks, and guidelines for radiation use in orthopaedic surgery. Clin Orthop Relat Res 375:126–132
ICRP (2007) The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 37(2–4):1–332. doi:10.1016/j.icrp.2007.10.003
Pinto Dos Santos D, Hempel JM, Kloeckner R, Düber C, Mildenberger P (2014) Teleradiology-update 2014. Radiologe 54(5):487–490. doi:10.1007/s00117-014-2661-3
Gundestrup M, Storm HH (1999) Radiation-induced acute myeloid leukaemia and other cancers in commercial jet cockpit crew: a population-based cohort study. Lancet 354(9195):2029–2031. doi:10.1016/S0140-6736(99)05093-X
Devalia KL, Guha A, Devadoss VG (2004) The need to protect the thyroid gland during image intensifier use in orthopaedic procedures. Acta Orthop Belg 70(5):474–477
Müller LP, Suffner J, Wenda K, Mohr W, Rudig L (1996) Radiation burden to the hands of surgeons in intramedullary nailing. Unfallchirurgie 22(6):253–259
Norris TG (2002) Radiation safety in fluoroscopy. Radiol Technol 73 (6):511–533; quiz 534–516, 566
Fuchs M, Modler H, Schmid A, Dumont C, Stürmer KM (1999) Measuring intraoperative radiation exposure of the trauma surgeon. Measuring eye, thyroid gland and hand with highly sensitive thermoluminescent detectors. Unfallchirurg 102(5):371–376
Dresing K (2011) X-ray in trauma and orthopedic surgery. Physical and biological impact, reasonable use, and radiation protection in the operating room. Oper Orthop Traumatol 23(1):70–78. doi:10.1007/s00064-010-0001-y
Sanders R, Koval KJ, DiPasquale T, Schmelling G, Stenzler S, Ross E (1993) Exposure of the orthopaedic surgeon to radiation. J Bone Joint Surg Am 75(3):326–330
Ortiz AO, Natarajan V, Gregorius DR, Pollack S (2006) Significantly reduced radiation exposure to operators during kyphoplasty and vertebroplasty procedures: methods and techniques. AJNR Am J Neuroradiol 27(5):989–994
Durán A, Hian SK, Miller DL, Le Heron J, Padovani R, Vano E (2013) A summary of recommendations for occupational radiation protection in interventional cardiology. Catheter Cardiovasc Interv 81(3):562–567. doi:10.1002/ccd.24520
Botchu R, Ravikumar K (2008) Radiation exposure from fluoroscopy during fixation of hip fracture and fracture of ankle: effect of surgical experience. Indian J Orthop 42(4):471–473. doi:10.4103/0019-5413.43398
Noordeen MH, Shergill N, Twyman RS, Cobb JP, Briggs T (1993) Hazard of ionizing radiation to trauma surgeons: reducing the risk. Injury 24(8):562–564
Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M (2000) Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 25 (20):2637–2645
Fuchs M, Modler H, Schmid A, Stürmer KM (1999) Strahlenschutz im Operationssaal. Operative Orthopädie und Traumatologie 11:328–333
Tasbas BA, Yagmurlu MF, Bayrakci K, Ucaner A, Heybeli M (2003) Which one is at risk in intraoperative fluoroscopy? Assistant surgeon or orthopaedic surgeon? Arch Orthop Trauma Surg 123(5):242–244. doi:10.1007/s00402-003-0516-x
Burns S, Thornton R, Dauer LT, Quinn B, Miodownik D, Hak DJ (2013) Leaded eyeglasses substantially reduce radiation exposure of the surgeon’s eyes during acquisition of typical fluoroscopic views of the hip and pelvis. J Bone Joint Surg Am 95(14):1307–1311. doi:10.2106/JBJS.L.00893
Wolf K, Bohndorf K, Vollert K, Kopp J (1996) Diagnostic imaging and radiation protection in trauma surgery. 2. Unfallchirurg 99(12):975–985
Giachino AA, Cheng M (1980) Irradiation of the surgeon during pinning of femoral fractures. J Bone Joint Surg Br 62-B(2):227–229
Mehlman CT, DiPasquale TG (1997) Radiation exposure to the orthopaedic surgical team during fluoroscopy: “how far away is far enough?”. J Orthop Trauma 11(6):392–398
Arnstein PM, Richards AM, Putney R (1994) The risk from radiation exposure during operative X-ray screening in hand surgery. J Hand Surg Br 19(3):393–396
Tremains MR, Georgiadis GM, Dennis MJ (2001) Radiation exposure with use of the inverted-c-arm technique in upper-extremity surgery. J Bone Joint Surg Am 83-A(5):674–678
Alonso JA, Shaw DL, Maxwell A, McGill GP, Hart GC (2001) Scattered radiation during fixation of hip fractures. Is distance alone enough protection? J Bone Joint Surg Br 83(6):815–818
Goldstone KE, Wright IH, Cohen B (1993) Radiation exposure to the hands of orthopaedic surgeons during procedures under fluoroscopic X-ray control. Br J Radiol 66(790):899–901
Tse V, Lising J, Khadra M, Chiam Q, Nugent R, Yeaman L, Mulcahy M (1999) Radiation exposure during fluoroscopy: should we be protecting our thyroids? Aust N Z J Surg 69(12):847–848
Synowitz M, Kiwit J (2006) Surgeon’s radiation exposure during percutaneous vertebroplasty. J Neurosurg Spine 4(2):106–109. doi:10.3171/spi.2006.4.2.106
Bott OJ, Wagner M, Duwenkamp C, Hellrung N, Dresing K (2009) Improving education on C-arm operation and radiation protection with a computer-based training and simulation system. Int J Comput Assist Radiol Surg 4(4):399–407. doi:10.1007/s11548-009-0322-1
Bott OJ, Dresing K, Wagner M, Raab BW, Teistler M (2011) Informatics in radiology: use of a C-arm fluoroscopy simulator to support training in intraoperative radiography. Radiographics 31(3):E65–E75. doi:10.1148/rg.313105125
Wagner M, Dresing K, Ludwig W, Ahrens CA, Bott OJ (2012) SIScaR-GPU: fast simulation and visualization of intraoperative scattered radiation to support radiation protection training. Stud Health Technol Inform 180:968–972
Wagner M, Duwenkamp C, Dresing K, Bott OJ (2009) An approach to calculate and visualize intraoperative scattered radiation exposure. Stud Health Technol Inform 150:831–835
Bundeskanzleramt (2014) Bundesrecht konsolidiert: Gesamte Rechtsvorschrift für Strahlenschutzverordnung fliegendes Personal, Fassung vom 22.08.2014. http://www.ris.bka.gv.at/GeltendeFassung.wxe?Abfrage=Bundesnormen&Gesetzesnummer=20004796. Accessed 22 Aug 2014
Strahlenschutz Bf (2014) Ionising Radiation > Occupational Radiation Protection > So wird überwacht. http://www.bfs.de/en/ion/beruf_schutz/methodik. Accessed 22 Aug 2014
Acknowledgments
A modified version of this abstract was accepted as an oral presentation at the DKOU, Congress of Orthopaedics and Traumatology (October 2015), Berlin, Germany. Furthermore, we would like to thank Ms. De-Simio-Hilton for her help with the preparation of the figures.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jentzsch, T., Pietsch, C.M., Stigler, B. et al. The compliance with and knowledge about radiation protection in operating room personnel: a cross-sectional study with a questionnaire. Arch Orthop Trauma Surg 135, 1233–1240 (2015). https://doi.org/10.1007/s00402-015-2257-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2257-z