Abstract
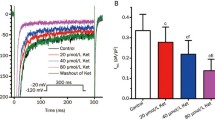
Blockade of the late Na+ current (I NaL) protects from ischemia/reperfusion damage; nevertheless, information on changes in I NaL during acute ischemia and their effect on intracellular milieu is missing. I NaL, cytosolic Na+ and Ca2+ activities (Nacyt, Cacyt) were measured in isolated rat ventricular myocytes during 7 min of simulated ischemia (ISC); in all the conditions tested, effects consistently exerted by ranolazine (RAN) and tetrodotoxin (TTX) were interpreted as due to I NaL blockade. The results indicate that I NaL was enhanced during ISC in spite of changes in action potential (AP) contour; I NaL significantly contributed to Nacyt rise, but only marginally to Cacyt rise. The impact of I NaL on Cacyt was markedly enhanced by blockade of the sarcolemmal(s) Na+/Ca2+ exchanger (NCX) and was due to the presence of (Na+-sensitive) Ca2+ efflux through mitochondrial NCX (mNCX). sNCX blockade increased Cacyt and decreased Nacyt, thus indicating that, throughout ISC, sNCX operated in the forward mode, in spite of the substantial Nacyt increment. Thus, a robust Ca2+ source, other than sNCX and including mitochondria, contributed to Cacyt during ISC. Most, but not all, of RAN effects were shared by TTX. (1) The paradigm that attributes Cacyt accumulation during acute ischemia to decrease/reversal of sNCX transport may not be of general applicability; (2) I NaL is enhanced during ISC, when the effect of Nacyt on mitochondrial Ca2+ transport may substantially contribute to I NaL impact on Cacyt; (3) RAN may act mostly, but not exclusively, through I NaL blockade during ISC.







Similar content being viewed by others
References
Aldakkak M, Camara AK, Heisner JS, Yang M, Stowe DF (2011) Ranolazine reduces Ca2+ overload and oxidative stress and improves mitochondrial integrity to protect against ischemia reperfusion injury in isolated hearts. Pharmacol Res 64:381–392. doi:10.1016/j.phrs.2011.06.018
Alemanni M, Rocchetti M, Re D, Zaza A (2011) Role and mechanism of subcellular Ca2+ distribution in the action of two inotropic agents with different toxicity. J Mol Cell Cardiol 50:910–918. doi:10.1016/j.yjmcc.2011.02.008
Allen DG, Xiao XH (2003) Role of the cardiac Na+/H+ exchanger during ischemia and reperfusion. Cardiovasc Res 57:934–941. doi:10.1016/s0008-6363(02)00836-2
Belardinelli L, Shryock JC, Fraser H (2006) Inhibition of the late sodium current as a potential cardioprotective principle: effects of the late sodium current inhibitor ranolazine. Heart 92(Suppl 4):iv6–iv14. doi:10.1136/hrt.2005.078790
Bernink FJ, Timmers L, Beek AM, Diamant M, Roos ST, van Rossum AC, Appelman Y (2014) Progression in attenuating myocardial reperfusion injury: an overview. Int J Cardiol 170:261–269. doi:10.1016/j.ijcard.2013.11.007
Boyman L, Williams GS, Khananshvili D, Sekler I, Lederer WJ (2013) NCLX: the mitochondrial sodium calcium exchanger. J Mol Cell Cardiol 59:205–213. doi:10.1016/j.yjmcc.2013.03.012
Calderon-Sanchez EM, Dominguez-Rodriguez A, Lopez-Haldon J, Jimenez-Navarro MF, Gomez AM, Smani T, Ordonez A (2016) Cardioprotective effect of ranolazine in the process of ischemia-reperfusion in adult rat cardiomyocytes. Rev Esp Cardiol (Engl Ed) 69:45–53. doi:10.1016/j.rec.2015.02.027
Caldwell JC, Burton FL, Cobbe SM, Smith GL (2012) Amplitude changes during ventricular fibrillation: a mechanistic insight. Front Physiol 3(147):1–8. doi:10.3389/fphys.2012.00147
Chen S, Li S (2012) The Na+/Ca(2)+ exchanger in cardiac ischemia/reperfusion injury. Med Sci Monit 18:RA161–RA165. doi:10.12659/MSM.883533
Cordeiro JM, Howlett SE, Ferrier GR (1994) Simulated ischaemia and reperfusion in isolated guinea pig ventricular myocytes. Cardiovasc Res 28:1794–1802. doi:10.1093/cvr/28.12.1794
Coronel R, Wilms-Schopman FJ, Fiolet JW, Opthof T, Janse MJ (1995) The relation between extracellular potassium concentration and pH in the border zone during regional ischemia in isolated porcine hearts. J Mol Cell Cardiol 27:2069–2073. doi:10.1016/0022-2828(95)90028-4
Cox DA, Conforti L, Sperelakis N, Matlib MA (1993) Selectivity of inhibition of Na(+)–Ca2+ exchange of heart mitochondria by benzothiazepine CGP-37157. J Cardiovasc Pharmacol 21:595–599. doi:10.1097/00005344-199304000-00013
Dehina L, Descotes J, Chevalier P, Bui-Xuan B, Romestaing C, Dizerens N, Mamou Z, Timour Q (2014) Protective effects of ranolazine and propranolol, alone or combined, on the structural and functional alterations of cardiomyocyte mitochondria in a pig model of ischemia/reperfusion. Fundam Clin Pharmacol 28:257–267. doi:10.1111/fcp.12033
Gadicherla AK, Stowe DF, Antholine WE, Yang M, Camara AK (2012) Damage to mitochondrial complex I during cardiac ischemia reperfusion injury is reduced indirectly by anti-anginal drug ranolazine. Biochim Biophys Acta 1817:419–429. doi:10.1016/j.bbabio.2011.11.021
Garciarena CD, Youm JB, Swietach P, Vaughan-Jones RD (2013) H(+)-activated Na(+) influx in the ventricular myocyte couples Ca(2)(+)-signalling to intracellular pH. J Mol Cell Cardiol 61:51–59. doi:10.1016/j.yjmcc.2013.04.008
Hale SL, Leeka JA, Kloner RA (2006) Improved left ventricular function and reduced necrosis after myocardial ischemia/reperfusion in rabbits treated with ranolazine, an inhibitor of the late sodium channel. J Pharmacol Exp Ther 318:418–423. doi:10.1124/jpet.106.103242
Hamilton NB, Kolodziejczyk K, Kougioumtzidou E, Attwell D (2016) Proton-gated Ca(2+)-permeable TRP channels damage myelin in conditions mimicking ischaemia. Nature 529:523–527. doi:10.1038/nature16519
Imahashi K, Pott C, Goldhaber JI, Steenbergen C, Philipson KD, Murphy E (2005) Cardiac-specific ablation of the Na+–Ca2+ exchanger confers protection against ischemia/reperfusion injury. Circ Res 97:916–921. doi:10.1161/01.RES.0000187456.06162.cb
Jung IS, Lee SH, Yang MK, Park JW, Yi KY, Yoo SE, Kwon SH, Chung HJ, Choi WS, Shin HS (2010) Cardioprotective effects of the novel Na+/H+ exchanger-1 inhibitor KR-32560 in a perfused rat heart model of global ischemia and reperfusion: involvement of the Akt-GSK-3beta cell survival pathway and antioxidant enzyme. Arch Pharm Res 33:1241–1251. doi:10.1007/s12272-010-0815-z
Kaibara M, Kameyama M (1988) Inhibition of the calcium channel by intracellular protons in single ventricular myocytes of the guinea-pig. J Physiol 403:621–640. doi:10.1113/jphysiol.1988.sp017268
Kirichok Y, Krapivinsky G, Clapham DE (2004) The mitochondrial calcium uniporter is a highly selective ion channel. Nature 427:360–364. doi:10.1038/nature02246
Kohlhaas M, Maack C (2013) Calcium release microdomains and mitochondria. Cardiovasc Res 98:259–268. doi:10.1093/cvr/cvt032
Lazdunski M, Frelin C, Vigne P (1985) The sodium/hydrogen exchange system in cardiac cells: its biochemical and pharmacological properties and its role in regulating internal concentrations of sodium and internal pH. J Mol Cell Cardiol 17:1029–1042. doi:10.1016/S0022-2828(85)80119-X
Linz WJ, Busch AE (2003) NHE-1 inhibition: from protection during acute ischaemia/reperfusion to prevention/reversal of myocardial remodelling. Naunyn Schmiedebergs Arch Pharmacol 368:239–246. doi:10.1007/s00210-003-0808-2
Lu J, Zang WJ, Yu XJ, Chen LN, Zhang CH, Jia B (2005) Effects of ischaemia-mimetic factors on isolated rat ventricular myocytes. Exp Physiol 90:497–505. doi:10.1113/expphysiol.2004.029421
Ma J, Song Y, Shryock JC, Hu L, Wang W, Yan X, Zhang P, Belardinelli L (2014) Ranolazine attenuates hypoxia- and hydrogen peroxide-induced increases in sodium channel late openings in ventricular myocytes. J Cardiovasc Pharmacol 64:60–68. doi:10.1097/FJC.0000000000000090
Maack C, Cortassa S, Aon MA, Ganesan AN, Liu T, O’Rourke B (2006) Elevated cytosolic Na+ decreases mitochondrial Ca2+ uptake during excitation-contraction coupling and impairs energetic adaptation in cardiac myocytes. Circ Res 99:172–182. doi:10.1161/01.RES.0000232546.92777.05
MacDonald AC, Howlett SE (2008) Differential effects of the sodium calcium exchange inhibitor, KB-R7943, on ischemia and reperfusion injury in isolated guinea pig ventricular myocytes. Eur J Pharmacol 580:214–223. doi:10.1016/j.ejphar.2007.10.055
Matlib MA, Zhou Z, Knight S, Ahmed S, Choi KM, Krause-Bauer J, Phillips R, Altschuld R, Katsube Y, Sperelakis N, Bers DM (1998) Oxygen-bridged dinuclear ruthenium amine complex specifically inhibits Ca2+ uptake into mitochondria in vitro and in situ in single cardiac myocytes. J Biol Chem 273:10223–10231. doi:10.1074/jbc.273.17.10223
Nakamura T, Hayashi H, Satoh H, Katoh H, Kaneko M, Terada H (1999) A single cell model of myocardial reperfusion injury: changes in intracellular Na+ and Ca2+ concentrations in guinea pig ventricular myocytes. Mol Cell Biochem 194:147–157. doi:10.1023/A:1006919929104
Namekata I, Shimada H, Kawanishi T, Tanaka H, Shigenobu K (2006) Reduction by SEA0400 of myocardial ischemia-induced cytoplasmic and mitochondrial Ca2+ overload. Eur J Pharmacol 543:108–115. doi:10.1016/j.ejphar.2006.06.012
Park CO, Xiao XH, Allen DG (1999) Changes in intracellular Na+ and pH in rat heart during ischemia: role of Na+/H+ exchanger. Am J Physiol 276:H1581–H1590
Robertson S, Thomson AL, Carter R, Stott HR, Shaw CA, Hadoke PW, Newby DE, Miller MR, Gray GA (2014) Pulmonary diesel particulate increases susceptibility to myocardial ischemia/reperfusion injury via activation of sensory TRPV1 and beta1 adrenoreceptors. Part Fibre Toxicol 11:12. doi:10.1186/1743-8977-11-12
Rocchetti M, Sala L, Rizzetto R, Staszewsky LI, Alemanni M, Zambelli V, Russo I, Barile L, Cornaghi L, Altomare C, Ronchi C, Mostacciuolo G, Lucchetti J, Gobbi M, Latini R, Zaza A (2014) Ranolazine prevents INaL enhancement and blunts myocardial remodelling in a model of pulmonary hypertension. Cardiovasc Res 104:37–48. doi:10.1093/cvr/cvu188
Salameh A, Dhein S, Beuckelmann DJ (2002) Role of the cardiac Na(+)/H(+)exchanger in [Ca(2+)](i)and [Na(+)](i)handling during intracellular acidosis. Effect of cariporide (Hoe 642). Pharmacol Res 45:35–41. doi:10.1006/phrs.2001.0908
Sanchez JA, Garcia MC, Sharma VK, Young KC, Matlib MA, Sheu SS (2001) Mitochondria regulate inactivation of L-type Ca2+ channels in rat heart. J Physiol 536:387–396. doi:10.1111/j.1469-7793.2001.0387c.xd
Saotome M, Katoh H, Satoh H, Nagasaka S, Yoshihara S, Terada H, Hayashi H (2005) Mitochondrial membrane potential modulates regulation of mitochondrial Ca2+ in rat ventricular myocytes. Am J Physiol Heart Circ Physiol 288:H1820–H1828. doi:10.1152/ajpheart.00589.2004
Sato R, Noma A, Kurachi Y, Irisawa H (1985) Effects of intracellular acidification on membrane currents in ventricular cells of the guinea pig. Circ Res 57:553–561. doi:10.1161/01.res.57.4.553
Soliman D, Wang L, Hamming KS, Yang W, Fatehi M, Carter CC, Clanachan AS, Light PE (2012) Late sodium current inhibition alone with ranolazine is sufficient to reduce ischemia- and cardiac glycoside-induced calcium overload and contractile dysfunction mediated by reverse-mode sodium/calcium exchange. J Pharmacol Exp Ther 343:325–332. doi:10.1124/jpet.112.196949
Song Y, Shryock JC, Wagner S, Maier LS, Belardinelli L (2006) Blocking late sodium current reduces hydrogen peroxide-induced arrhythmogenic activity and contractile dysfunction. J Pharmacol Exp Ther 318:214–222. doi:10.1124/jpet.106.101832
Swietach P, Youm JB, Saegusa N, Leem CH, Spitzer KW, Vaughan-Jones RD (2013) Coupled Ca2+/H+ transport by cytoplasmic buffers regulates local Ca2+ and H+ ion signaling. Proc Natl Acad Sci USA 110:E2064–E2073. doi:10.1073/pnas.1222433110
Tanaka H, Nishimaru K, Aikawa T, Hirayama W, Tanaka Y, Shigenobu K (2002) Effect of SEA0400, a novel inhibitor of sodium-calcium exchanger, on myocardial ionic currents. Br J Pharmacol 135:1096–1100. doi:10.1038/sj.bjp.0704574
Tang Q, Ma J, Zhang P, Wan W, Kong L, Wu L (2012) Persistent sodium current and Na+/H+ exchange contributes to the augmentation of the reverse Na+/Ca2+ exchange during hypoxia or acute ischemia in ventricular myocytes. Pflugers Arch 463:513–522. doi:10.1007/s00424-011-1070-y
Tanonaka K, Motegi K, Arino T, Marunouchi T, Takagi N, Takeo S (2012) Possible pathway of Na(+) flux into mitochondria in ischemic heart. Biol Pharm Bull 35:1661–1668. doi:10.1248/bpb.b12-00010
Undrovinas AI, Belardinelli L, Undrovinas NA, Sabbah HN (2006) Ranolazine improves abnormal repolarization and contraction in left ventricular myocytes of dogs with heart failure by inhibiting late sodium current. J Cardiovasc Electrophysiol 17(Suppl 1):S169–S177. doi:10.1111/j.1540-8167.2006.00401.x
Undrovinas AI, Fleidervish IA, Makielski JC (1992) Inward sodium current at resting potentials in single cardiac myocytes induced by the ischemic metabolite lysophosphatidylcholine. Circ Res 71:1231–1241. doi:10.1161/01.res.71.5.1231
van Borren MM, Baartscheer A, Wilders R, Ravesloot JH (2004) NHE-1 and NBC during pseudo-ischemia/reperfusion in rabbit ventricular myocytes. J Mol Cell Cardiol 37:567–577. doi:10.1016/j.yjmcc.2004.05.017
Wang XJ, Wang LL, Fu C, Zhang PH, Wu Y, Ma JH (2014) Ranolazine attenuates the enhanced reverse Na(+)-Ca(2)(+) exchange current via inhibiting hypoxia-increased late sodium current in ventricular myocytes. J Pharmacol Sci 124:365–373. doi:10.1254/jphs.13202FP
Wilde AA, Escande D, Schumacher CA, Thuringer D, Mestre M, Fiolet JW, Janse MJ (1990) Potassium accumulation in the globally ischemic mammalian heart. A role for the ATP-sensitive potassium channel. Circ Res 67:835–843. doi:10.1161/01.res.67.4.835
Williams IA, Xiao XH, Ju YK, Allen DG (2007) The rise of [Na(+)] (i) during ischemia and reperfusion in the rat heart-underlying mechanisms. Pflugers Arch 454:903–912. doi:10.1007/s00424-007-0241-3
Zaza A, Rocchetti M (2013) The late Na+ current—origin and pathophysiological relevance. Cardiovasc Drugs Ther 27:61–68. doi:10.1007/s10557-012-6430-0
Acknowledgements
This research was supported by grant from Gilead Inc. (Fremont, CA, US) and FAR 2015 to A. Zaza. We are grateful to Dr. Luiz Belardinelli for providing stimulating discussion throughout the execution of the study and Dr. Luca Sala for contributing to some experiments and providing insightful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All experiment were approved and conducted in accordance with guidelines issued by the Animal Care Committee of the University Milano-Bicocca, in compliance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The manuscript does not contain human data.
Conflict of interest
The study has been partially funded by Gilead, Inc. (Fremont, CA), which is the patent holder for Ranolazine. The authors declare that they have no further conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ronchi, C., Torre, E., Rizzetto, R. et al. Late sodium current and intracellular ionic homeostasis in acute ischemia. Basic Res Cardiol 112, 12 (2017). https://doi.org/10.1007/s00395-017-0602-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-017-0602-9