Abstract
Objective
Ankylosing spondylitis (AS) is a chronic systemic inflammatory disease. Via autoimmune mediators, AS can damage the auditory system similar to other systems. Otoacoustic emission studies in AS patients showed that the damage that causes hearing loss was in the outer hair cells. The medial olivocochlear (MOC) reflex is used to evaluate the MOC efferent system (MOES), which includes the outer hair cells. The aim of this study was to evaluate the presence of subclinical damage in the inner ear with the aid of the MOC reflex test in AS patients with no hearing complaints.
Patients and methods
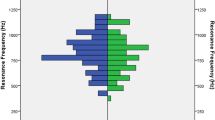
Thirty-four patients with AS and a control group of 30 healthy volunteers with similar demographic characteristics were evaluated in the study. Otoacoustic emission responses, MOC reflex results, and frequency-specific and total suppression findings were compared between the groups. The relationship between clinical and laboratory findings for the AS patients, and the MOC reflex data were also investigated.
Results
Reduced MOC reflex response (p = 0.04) and suppression (p = 0.019) were detected in AS patients. When the clinical and laboratory findings for the AS patients and the MOC reflex test results were compared, a significant correlation was found only between the MOC reflex and the erythrocyte sedimentation rate.
Conclusion
The results showed that AS can damage the inner ear, especially the MOES, and can reduce the MOC reflex response without clinical hearing loss.
Zusammenfassung
Ziel
Spondylitis ankylosans (AS) ist eine chronische systemische entzündliche Erkrankung. Über autoimmun wirkende Mediatoren kann die AS das Hörsystem – ähnlich wie andere Systeme – schädigen. Die Untersuchung otoakustischer Emissionen bei AS-Patienten ergab, dass die Schädigung, welche die Schwerhörigkeit bedingt, in den äußeren Haarzellen bestand. Der mediale olivocochleäre (MOC-)Reflex wird eingesetzt, um das mediale olivocochleäre efferente System (MOES) zu untersuchen, welches auch die äußeren Haarzellen umfasst. Ziel der vorliegenden Studie war es, das Vorliegen subklinischer Schädigungen im Innenohr mithilfe der Untersuchung des MOC-Reflexes bei AS-Patienten ohne Hörbeschwerden zu ermitteln.
Patienten und Methoden
In der Studie wurden 34 AS-Patienten und eine Kontrollgruppe von 30 gesunden Probanden mit ähnlichen demographischen Merkmalen untersucht. Die Ergebnisse der Messung der otoakustischen Emissionen, des MOC-Reflexes und frequenzspezifische Befunde sowie Gesamtbefunde für die (kontralaterale) Suppression wurden zwischen den beiden Gruppen verglichen. Der Zusammenhang zwischen den klinischen und den Laborbefunden für die AS-Patienten und den MOC-Reflex-Daten wurden ebenfalls untersucht.
Ergebnisse
Bei den AS-Patienten wurden eine abgeschwächte Reaktion auf die Prüfung des MOC-Reflexes (p = 0,04) und bei der Untersuchung der Suppression (p = 0,019) festgestellt. Im Rahmen des Vergleichs der klinischen und der Laborbefunde für die AS-Patienten mit den Ergebnissen beim MOC-Reflex-Test stellte sich eine signifikante Korrelation nur zwischen dem MOC-Reflex und der Blutkörperchensenkungsgeschwindigkeit heraus.
Schlussfolgerung
Die vorliegenden Ergebnisse zeigen, dass durch AS das Innenohr, insbesondere das MOES, geschädigt werden und die Reaktion beim MOC-Reflex auch ohne bestehende klinische Schwerhörigkeit abgeschwächt sein kann.




Similar content being viewed by others
References
Amor-Dorado JC, Barreira-Fernandez MP, Vazquez-Rodriguez TR et al (2011) Audiovestibular manifestations in patients with ankylosing spondylitis. Medicine 90:99–109
Magaro M, Ceresia G, Frustaci A (1984) Arthritis of the middle ear in ankylosing spondylitis. Ann Rheum Dis 43:658–659
Alatas N, Yazgan P, Ozturk A et al (2005) Audiological findings in patients with ankylosing spondylitis. J Laryngol Otol 119:534–539
Dagli M, Sivas Acar F, Karabulut H et al (2007) Evaluation of hearing and cochlear function by DPOAE and audiometric tests in patients with ankylosing spondilitis. Rheumatol Int 27:511–516
Kahveci OK, Demirdal US, Duran A et al (2012) Hearing and cochlear function of patients with ankylosing spondylitis. Clin Rheumatol 31:1103–1108
Papadimitraki ED, Kyrmizakis DE, Kritikos I et al (2004) Ear-nose-throat manifestations of autoimmune rheumatic diseases. Clin Exp Rheumatol 22:485–494
Raza K, Karokis D, Wilson F et al (1998) Sensorineural hearing loss, iritis and ankylosing spondylitis. Br J Rheumatol 37:1363
Guinan JJ Jr (2010) Cochlear efferent innervation and function. Curr Opin Otolaryngol Head Neck Surg 18:447–453
Rabbitt RD, Brownell WE (2011) Efferent modulation of hair cell function. Curr Opin Otolaryngol Head Neck Surg 19:376–381
Guinan JJ Jr (2006) Olivocochlear efferents: anatomy, physiology, function, and the measurement of efferent effects in humans. Ear Hear 27:589–607
Wersinger E, Fuchs PA (2011) Modulation of hair cell efferents. Hear Res 279:1–12
Linden S van der, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
Garrett S, Jenkinson T, Kennedy LG et al (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21:2286–2291
Machado P, Landewe R, Lie E et al (2011) Ankylosing Spondylitis Disease Activity Score (ASDAS): defining cut-off values for disease activity states and improvement scores. Ann Rheum Dis 70:47–53
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, Jenkinson T (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21:2281–2285
Braun J, Bollow M, Remlinger G, Eggens U, Rudwaleit M, Distler A, Sieper J (1998) Prevalence of spondylarthropathies in HLA-B27 positive and negative blood donors. Arthritis Rheum 41:58–67
Eryilmaz A, Dagli M, Karabulut H et al (2007) Evaluation of hearing loss in patients with ankylosing spondylitis. J Laryngol Otol 121:845–849
Khedr EM, Rashad SM, Hamed SA et al (2009) Neurological complications of ankylosing spondylitis: neurophysiological assessment. Rheumatol Int 29:1031–1040
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.S. Beyazal, A. Özgür, S. Terzi, M. Çeliker, and E. Dursun declare that there are no conflicts of interest and that there is no support or funding for research in this study.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Beyazal, M.S., Özgür, A., Terzi, S. et al. Medial olivocochlear reflex in ankylosing spondylitis patients. Z Rheumatol 75, 1016–1020 (2016). https://doi.org/10.1007/s00393-016-0100-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-016-0100-8