Abstract
Background
Transvascular (TV-AVI) or transapical (TA-AVI) aortic valve implantation (TAVI) is a treatment option for patients with aortic stenosis being at high or prohibitive risk for surgical aortic valve implantation (SAVR). Randomized data demonstrated that these subgroups can safely been treated with TAVI. However, a comparison of SAVR and TAVI in intermediate and low-risk patients is missing. Therefore, the aim of the analysis was to compare TAVI and SAVR in all patients who were treated for aortic valve stenosis in Germany throughout 1 year.
Methods
The mandatory quality assurance collects data on the in-hospital outcome from all patients (n = 20,340) undergoing either SAVR or TAVI in Germany. In order to compare the different treatment approaches patients were categorized into four risk groups using the logistic EuroScore I (ES). In-hospital mortality and peri- and postprocedural complications were analyzed.
Results
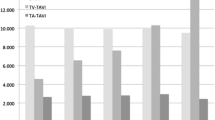
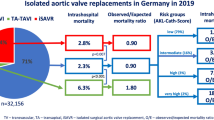
The in-hospital mortality did not differ between TV-AVI and SAVR in the low risk group (ES <10 %: TV-AVI 2.4 %, SAVR 2.0 %, p = 0.302) and was significantly higher for SAVR in all other risk groups (ES 10–20 %: TV-AVI 3.5 %, SAVR 5.3 %; p = 0.025; ES 20–30 %: TV-AVI 5.5 %, SAVR 12.2 %, p < 0.001; ES >30 %: TV-AVI 6.5 %, SAVR 12.9 %, p = 0.008). TA-AVI had a significantly higher mortality in all risk groups compared to TV-AVI. In comparison to SAVR, TA-AVI had a higher mortality in patients with ES <10, comparable mortality in ES 10–20 %, and lower mortality in patients with an ES >20 %. The overall stroke rate was 2.3 %. It occurred more frequently in patients with an ES <10 % treated with a transapical approach (SAVR 1.8 %, TV-AVI 1.9 %, TA-AVI 3.1 %, p < 0.01). There were no statistically significant differences in all other comparisons.
Conclusions
This study demonstrates that TAVI provides excellent outcomes in all risk categories. Compared with SAVR, TV-TAVI yields similar in-hospital mortality among low-risk patients and lower in-hospital mortality among intermediate and high-risk patient populations.



Similar content being viewed by others
References
Turina J, Hess O, Sepulcri F, Krayenbuehl HP (1987) Spontaneous course of aortic valve disease. Eur Heart J 8(5):471–483
Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology, European Association for Cardio-Thoracic Surgery, Vahanian A et al (2012) Guidelines on the management of valvular heart disease (version 2012). European Heart Journal. 33(19):2451–2496
Nishimura RA, Otto CM, Bonow RO et al (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63(22):e57–185
Iung B, Cachier A, Baron G et al (2005) Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J 26(24):2714–2720
Walther T, Mollmann H, van Linden A, Kempfert J (2011) Transcatheter aortic valve implantation transapical: step by step. Semin Thorac Cardiovasc Surg 23(1):55–61
Webb JG, Chandavimol M, Thompson CR et al (2006) Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 113(6):842–850
Cribier A, Eltchaninoff H, Bash A et al (2002) Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 106(24):3006–3008
Leon MB, Smith CR, Mack M et al (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363(17):1597–1607
Smith CR, Leon MB, Mack MJ et al (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364(23):2187–2198
Hamm CW, Mollmann H, Holzhey D et al (2014) The German Aortic Valve Registry (GARY): in-hospital outcome. Eur Heart J 35(24):1588–1598
Mohr FW, Holzhey D, Mollmann H et al (2014) The German Aortic Valve Registry: 1-year results from 13 680 patients with aortic valve diseasedagger. Eur J Cardiothoracc Surg 46(5):808–816
Gilard M, Eltchaninoff H, Iung B et al (2012) Registry of transcatheter aortic-valve implantation in high-risk patients. N Engl J Med 366(18):1705–1715
Milburn K, Bapat V, Thomas M (2014) Valve-in-valve implantations: is this the new standard for degenerated bioprostheses? Review of the literature. Clin Res Cardiol 103(6):417–429
Kim WK, Kempfert J, Walther T, Mollmann H (2015) Transfemoral valve-in-valve implantation of a St. Jude Medical Portico in a failing trifecta bioprosthesis: a case report. Clin Res Cardiol 104(4):363–365
Greif M, Lange P, Mair H et al (2012) Transcatheter Edwards Sapien XT valve in valve implantation in degenerated aortic bioprostheses via transfemoral access. Clin Res Cardiol 101(12):993–1001
Adams DH, Popma JJ, Reardon MJ et al (2014) Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 370(19):1790–1798
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R (1999) European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 16(1):9–13
Roques F, Nashef SA, Michel P et al (1999) Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg 15(6):816–822 (discussion 822–813)
Osswald BR, Gegouskov V, Badowski-Zyla D et al (2009) Overestimation of aortic valve replacement risk by EuroSCORE: implications for percutaneous valve replacement. Eur Heart J 30(1):74–80
Wendt D, Osswald BR, Kayser K et al (2009) Society of Thoracic Surgeons score is superior to the EuroSCORE determining mortality in high risk patients undergoing isolated aortic valve replacement. Ann Thorac Surg 88(2):468–474
Rosenhek R, Iung B, Tornos P et al (2012) ESC Working Group on Valvular Heart Disease Position Paper: assessing the risk of interventions in patients with valvular heart disease. Eur Heart J 33(7):822–828, 828a, 828b
Kim W-K, Liebetrau C, van Linden A et al (2015) Myocardial injury associated with transcatheter aortic valve implantation (TAVI). Clin Res Cardiol. doi:10.1007/s00392-015-0949-6
Walther T, Hamm CW, Schuler G et al (2015) Perioperative results and complications in 15,964 transcatheter aortic valve replacements: prospective data from the GARY registry. J Am Coll Cardiol 65(20):2173–2180
Saczynski JS, Marcantonio ER, Quach L et al (2012) Cognitive trajectories after postoperative delirium. N Engl J Med 367(1):30–39
Koster S, Hensens AG, van der Palen J (2009) The long-term cognitive and functional outcomes of postoperative delirium after cardiac surgery. Ann Thorac Surg 87(5):1469–1474
Sockalingam S, Parekh N, Bogoch II et al (2005) Delirium in the postoperative cardiac patient: a review. J Card Surg 20(6):560–567
Eggebrecht H, Schmermund A, Voigtlander T, Kahlert P, Erbel R, Mehta RH (2012) Risk of stroke after transcatheter aortic valve implantation (TAVI): a meta-analysis of 10,037 published patients. EuroIntervention 8(1):129–138
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Möllmann and K. Bestehorn contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Möllmann, H., Bestehorn, K., Bestehorn, M. et al. In-hospital outcome of transcatheter vs. surgical aortic valve replacement in patients with aortic valve stenosis: complete dataset of patients treated in 2013 in Germany. Clin Res Cardiol 105, 553–559 (2016). https://doi.org/10.1007/s00392-016-0962-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-016-0962-4