Abstract
Purpose
Besides antibiotic prophylaxis, antiseptic skin preparation is an important measure to prevent surgical site infection (SSI). No reports have detailed the relationship between SSI and umbilical microflora following laparoscopic colorectal cancer with a transumbilical longitudinal incision.
Methods
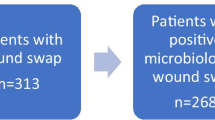
Risk factors and the rate of SSI were investigated in 453 patients who underwent laparoscopic colorectal resection over a 3-year period. Microbiological samples were collected from the umbilicus and SSI areas.
Results
After laparoscopic procedure, we observed SSIs in approximately 5% of cases, with superficial SSI in 15 (3.3%) patients and organ/space SSIs 7 (1.5%). In univariate analysis, preoperative albumin (Alb) value and anastomosis of enterocolostomy were significantly associated with superficial SSI development. Also, age, blood loss, stoma, tumor site (rectum), and Hartmann/abdominal perineal resection (APR) were significant risk factors for organ/space SSI. In multivariate analysis, the preoperative Alb value was the most significant factor associated with a predisposition to superficial SSI. The bacteria detected in SSI were mostly different from those at wound closure. Antibiotic-resistant bacteria were included in organ/space SSI all cases.
Conclusions
SSI development with laparoscopic surgery reportedly occurs in about 3–15% cases. The SSI rate in this study and other reports was comparable. Using small transumbilical longitudinal incision in laparoscopic colorectal surgery is less likely to cause SSI when sufficient control measures are enacted, even though the umbilicus contains resident bacteria in abundance.
Similar content being viewed by others
References
Watanabe T, Itabashi M, Shimada Y et al (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20:207–239. doi:10.1007/s10147-015-0801-z
Howard DP, Datta G, Cunnick G et al (2010) Surgical site infection rate is lower in laparoscopic than open colorectal surgery. Color Dis 12:423–427
Poon JT, Law WL, Wong IW et al (2009) Impact of laparoscopic colorectal resection on surgical site infection. Ann Surg 49:77–81
Kiran RP, El-Gazzaz GH, Vogel JD et al (2010) Laparoscopic approach significantly reduces surgical site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg 211:232–238
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection, 1999. U.S. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27:97–132
Yamamoto S, Fujita S, Akasu T et al (2007) Wound infection after elective laparoscopic surgery for colorectal carcinoma. Surg Endosc 21:2248–2252
Kennedy GD, Heise C, Rajamanickam V et al (2009) Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the National Surgical Quality Improvement Program. Ann Surg 249:596–601
Chang SK, Lomanto D, Mayasari M (2012) Single-port laparoscopic spleen preserving distal pancreatectomy. Minim Invasive Surg 2012:197429. doi:10.1155/2012/197429
Delgado S, Ibarzabal A, Adelsdorfer C et al (2012) Transumbilical single-port sleeve gastrectomy: initial experience and comparative study. Surg Endsc 26:1247–1253
Desai MM, Stein R, Rao P et al (2009) Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for advanced reconstruction: initial experience. Urology 73:182–187
Kleeff J, Erkan M, Jager C et al (2015) Umbilical microflora, antiseptic skin preparation and surgical site infection in abdominal surgery. Surg Infect 16:450–454
Hulcr J, Latimer AM, Henley JB et al (2012) A jungle in there: bacteria in belly buttons are highly diverse, but predictable. PLoS One 7:e47712. doi:10.1371/journal.pone.0047712
Paes TR, Stoker DL, Ng T et al (1987) Circumumbilical versus transumbilical abdominal incision. Br J Surg 74:822–823
Sharples A, McArthur D, McNamara K, Lengyel J (2011) Back to basics—cutting the cord on umbilical infections. Ann R Coll Surg Engl 93:120–122
Enad JG (1963) Midline abdominal transumbilical incision. Phillipp J Surg Spec 18:188–193
Kashimura N, Kusachi S, Konishi T et al (2012) Impact of surgical site infection after colorectal surgery on hospital stay and medical expenditure in Japan. Surg Today 42:639–645
Anderson DJ, Kaye KS, Classen D et al (2008) Strategies to prevent surgical site infections in acute care hospitals. Inf Cont Hosp Epideiol 29:S51–S61
Glyn GJ (2006) The anatomy of general surgical operations, 3rd edn. Churchill Livingstone, Philadelphia, pp 6–7
Chummy SS, Raymond JL (2006) Last’s anatomy. In: Elsevier Health Sciences, 11th edn. Maryland Heights, pp 240–241
Braga M, Vignali A, Zuliani W et al (2005) Laparoscopic versus open colorectal surgery; cost-benefit analysis in a single-center randomized trial. Ann Surg 242:890–896
Guillou P, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal (MRC CLASICC trial): multicenter, randomized controlled trial. Lancet 365:1718–1172
Hamzaoglu I, Baca B, Boler DE et al (2004) Is umbilical flora responsible for surgical site infection after laparoscopic surgery? Surg Laparosc Endosc Percutan Tech 14:263–267
Tschudin-Sutter S, Frei R, Egli-Gany D et al (2012) No risk of surgical site infections from residual bacteria after disinfection with povidone-iodine-alcohol in 1014 cases: a prospective observational study. Ann Surg 255:565–569
Cervantes-Sanchez CR, Gutierrez-Vega R, Vazquez-Carpizo JA et al (2000) Syringe pressure irrigation of subdermic tissue after appendectomy to decrease the incidence of postoperative wound infection. Would J Surg 24:38–41
Mazuski JE, Sawyer RG, Nathens AB et al (2002) The Surgical Infection Society guidelines on antimicrobial therapy for intra-abdominal infections: evidence for the recommendations. Surg Infect 3:161–173
Zhang HY, Zhao CL, Xie J et al (2016) To drain or not to drain in colorectal anastomosis: a meta-analysis. Int J Color Dis 31:951–960
Acknowledgements
The authors thank all members of the Iwate Medical University School of Medicine for their excellent assistance. The authors would like to thank Enago ( www.enago.jp ) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosures
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yaegashi, M., Otsuka, K., Kimura, T. et al. Transumbilical abdominal incision for laparoscopic colorectal surgery does not increase the risk of postoperative surgical site infection. Int J Colorectal Dis 32, 715–722 (2017). https://doi.org/10.1007/s00384-017-2753-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2753-4