Abstract
Purpose
Our objective was to perform a meta-analysis on RCTs that compared outcomes in children with perforated appendicitis (PA) who underwent either early appendectomy (EA) or interval appendectomy (IA). We also sought to determine if the presence of an intra-abdominal abscess (IAA) at admission impacted treatment strategy and outcomes.
Methods
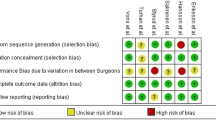
We identified two RCTs comparing EA versus IA in children with PA. A meta-analysis was performed using regression models and the overall adverse event rate was analyzed. The treatment effect variation depending on the presence of IAA at admission was also evaluated.
Results
EA significantly reduced the odds of an adverse event (OR 0.28, 95 % CI 0.1–0.77) and an unplanned readmission (OR 0.08, 95 % CI 0.01–0.67), as well as the total charges (79 % of the IA, 95 % CI 63–100) for those who did not have an IAA at admission. In children with an IAA, there was no difference between EA and IA. However, heterogeneity of treatment effect was present regarding IAA at presentation.
Conclusions
While EA appears to improve outcomes in patients without an abscess, the published data support no significant difference in outcomes between EA and IA in patients with an abscess.



Similar content being viewed by others
References
Ostlie DJ, St Peter SD (2010) The current state of evidence-based pediatric surgery. J Pediatr Surg 45(10):1940–1946
Stewart LA, Parmar MK (1993) Meta-analysis of the literature or of individual patient data: is there a difference? Lancet 341(8842):418–422
Newman K, Ponsky T, Kittle K, Dyk L, Throop C, Gieseker K et al (2003) Appendicitis 2000: variability in practice, outcomes, and resource utilization at thirty pediatric hospitals. J Pediatr Surg 38(3):372–379 (discussion372–379)
Blakely ML, Williams R, Dassinger MS, Eubanks JW, Fischer P, Huang EY et al (2011) Early vs interval appendectomy for children with perforated appendicitis. Arch Surg 146(6):660–665
St Peter SD, Aguayo P, Fraser JD, Keckler SJ, Sharp SW, Leys CM et al (2010) Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg 45(1):236–240
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, Tierney JF (2015) Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. JAMA 313(16):1657. doi:10.1001/jama.2015.3656
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
R Development Team (2005) R: a language and environment for statistical computing. google.com, Vienna, p 1820
Kraemer HC, Frank E, Kupfer DJ (2006) Moderators of treatment outcomes: clinical, research, and policy importance. JAMA 296(10):1286–1289
Brookes ST, Whitely E, Egger M, Smith GD, Mulheran PA, Peters TJ (2004) Subgroup analyses in randomized trials: risks of subgroup-specific analyses; power and sample size for the interaction test. J Clin Epidemiol 57(3):229–236
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ 326(7382):219
Altman DG, Matthews JN (1996) Statistics notes. Interaction 1: heterogeneity of effects. BMJ 313(7055):486
Acknowledgments
Supported by the National Center for Research Resources, Grant UL1RR024975-01 and National Center for Advancing Translational Sciences, Grant 2UL1TR000445-06.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Duggan, E.M., Marshall, A.P., Weaver, K.L. et al. A systematic review and individual patient data meta-analysis of published randomized clinical trials comparing early versus interval appendectomy for children with perforated appendicitis. Pediatr Surg Int 32, 649–655 (2016). https://doi.org/10.1007/s00383-016-3897-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3897-y