Abstract
Objectives
Our objectives were to: (1) delineate factors associated with surgery at <1 year and (2) determine if early intervention was associated with increased risk of readmission.
Methods
We conducted a retrospective review of children age 0–18 years with a diagnosis of UPJ obstruction who underwent pyeloplasty from 1/1/1999 to 9/1/2009 using the PHIS database. Data collected included patient factors (race, gender, insurance type, APR-DRG severity of illness) and hospital factors (annual case volume, census region, academic status). Outcomes assessed were: age at surgery and hospital readmission within 1 year of surgery. Data were analyzed using logistic regression and Cox PH for multivariate analyses.
Results
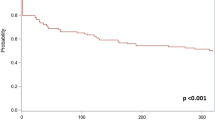
4499 children met study criteria. Minority race (OR 1.55), male gender (OR 1.49), public insurance (OR 1.37), high severity of illness (OR 3.60), Southern region (OR 1.44), and low hospital volume (OR 1.37) were significant predictors of early surgery (p < 0.05). Only early surgery (HR 2.42; 95 % CI 1.67–3.49 2.42) was associated with increased risk of readmission.
Conclusions
In children with UPJ obstruction, age at surgery is associated with patient demographic and hospital factors. Early surgery is associated with higher rates of readmission, suggesting that variations in age at surgery may be associated with significant differences in outcomes.
Similar content being viewed by others
Abbreviations
- APR-DRG:
-
All patient refined diagnosis related groups
- PHIS:
-
Pediatric health information system
- UPJ:
-
Ureteropelvic junction
- UTI:
-
Urinary tract infection
References
Kitchens DM, Herndon CD (2009) Antenatal hydronephrosis. Current Urol Rep 10(2):126–133
Ponsky TA, Huang ZJ, Kittle K, Eichelberger MR, Gilbert JC, Brody F, Newman KD (2004) Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA 292(16):1977–1982. doi:10.1001/jama.292.16.1977
Nelson CP (2007) Evidence of variation by race in the timing of surgery for correction of pediatric ureteropelvic junction obstruction. J Urol 178 (4 Pt 1):1463–1468; discussion 1468. doi:10.1016/j.juro.2007.05.167
Nelson CP, Park JM, Dunn RL, Wei JT (2005) Contemporary trends in surgical correction of pediatric ureteropelvic junction obstruction: data from the nationwide inpatient sample. J Urol 173(1):232–236. doi:10.1097/01.ju.0000148439.22885.b4
Onen A, Jayanthi VR, Koff SA (2002) Long-term followup of prenatally detected severe bilateral newborn hydronephrosis initially managed nonoperatively. J Urol 168(3):1118–1120. doi:10.1097/01.ju.0000024449.19337.8d
Ulman I, Jayanthi VR, Koff SA (2000) The long-term followup of newborns with severe unilateral hydronephrosis initially treated nonoperatively. J Urol 164(3 Pt 2):1101–1105
Muldoon JH (1999) Structure and performance of different DRG classification systems for neonatal medicine. Pediatrics 103 (1 Suppl E):302–318
Sedman AB, Bahl V, Bunting E, Bandy K, Jones S, Nasr SZ, Schulz K, Campbell DA (2004) Clinical redesign using all patient refined diagnosis related groups. Pediatrics 114(4):965–969. doi:10.1542/peds.2004-0650
Berry JG, Hall DE, Kuo DZ, Cohen E, Agrawal R, Feudtner C, Hall M, Kueser J, Kaplan W, Neff J (2011) Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA 305(7):682–690. doi:10.1001/jama.2011.122
Shone LP, Dick AW, Brach C, Kimminau KS, LaClair BJ, Shenkman EA, Col JF, Schaffer VA, Mulvihill F, Szilagyi PG, Klein JD, VanLandeghem K, Bronstein J (2003) The role of race and ethnicity in the State Children’s Health Insurance Program (SCHIP) in four states: are there baseline disparities, and what do they mean for SCHIP? Pediatrics 112(6 Pt 2):e521
Hwang AH, Hwang MM, Xie HW, Hardy BE, Skaggs DL (2005) Access to urologic care for children in California: medicaid versus private insurance. Urology 66(1):170–173. doi:10.1016/j.urology.2005.01.065
Skinner AC, Mayer ML (2007) Effects of insurance status on children’s access to specialty care: a systematic review of the literature. BMC Health Serv Res 7:194. doi:10.1186/1472-6963-7-194
Langford AT, Resnicow K, Davis RE, Alexander GL, Calvi J, Weise C, Tolsma D (2010) Ethnic Identity predicts loss-to-follow-up in a health promotion trial. Contemp Clin Trials 31(5):414–418. doi:10.1016/j.cct.2010.06.006
Longpre M, Nguan A, Macneily AE, Afshar K (2012) Prediction of the outcome of antenatally diagnosed hydronephrosis: a multivariable analysis. J Pediatr Urol 8(2):135–139. doi:10.1016/j.jpurol.2011.05.013
Liang CC, Cheng PJ, Lin CJ, Chen HW, Chao AS, Chang SD (2002) Outcome of prenatally diagnosed fetal hydronephrosis. J Reprod Med 47(1):27–32
Averill RF, Goldfield N, Hughes JS, Bonazelli J, McCullough EC, Steinbeck BA, Mullin R, Tang AM, Muldoon J, Turner L, Gay J (2003) All Patient Refined Diagnosis Related Groups Version 20.0 Methodology Review. http://www.hcup-us.ahrq.gov/db/nation.nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf. Accessed 17 Dec 2014
Somme S, Bronsert M, Morrato E, Ziegler M (2013) Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics 132(6):e1466–e1472. doi:10.1542/peds.2013-1243
Chu DI, Lloyd JC, Balsara ZR, Wiener JS, Ross SS, Routh JC (2014) Variation in use of nephron-sparing surgery among children with renal tumors. J Pediatr Urol 10(4):724–729. doi:10.1016/j.jpurol.2013.12.019
Minnillo BJ, Cruz JA, Sayao RH, Passerotti CC, Houck CS, Meier PM, Borer JG, Diamond DA, Retik AB, Nguyen HT (2011) Long-term experience and outcomes of robotic assisted laparoscopic pyeloplasty in children and young adults. J Urol 185(4):1455–1460. doi:10.1016/j.juro.2010.11.056
Braga LH, Lorenzo AJ, Farhat WA, Bagli DJ, Khoury AE, Pippi Salle JL (2008) Outcome analysis and cost comparison between externalized pyeloureteral and standard stents in 470 consecutive open pyeloplasties. The Journal of urology 180 (4 Suppl):1693–1698; discussion 1698–1699. doi:10.1016/j.juro.2008.05.084
Bayne AP, Lee KA, Nelson ED, Cisek LJ, Gonzales ET Jr, Roth DR (2011) The impact of surgical approach and urinary diversion on patient outcomes in pediatric pyeloplasty. J Urol 186(4 Suppl):1693–1698. doi:10.1016/j.juro.2011.03.103
Braga LH, Lorenzo AJ, Bagli DJ, Keays M, Farhat WA, Khoury AE, Salle JL (2008) Risk factors for recurrent ureteropelvic junction obstruction after open pyeloplasty in a large pediatric cohort. The Journal of urology 180 (4 Suppl):1684–1687; discussion 1687–1688. doi:10.1016/j.juro.2008.03.086
Sutherland RW, Chung SK, Roth DR, Gonzales ET (1997) Pediatric pyeloplasty: outcome analysis based on patient age and surgical technique. Urology 50(6):963–966. doi:10.1016/s0090-4295(97)00397-x
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vemulakonda, V.M., Wilcox, D.T., Crombleholme, T.M. et al. Factors associated with age at pyeloplasty in children with ureteropelvic junction obstruction. Pediatr Surg Int 31, 871–877 (2015). https://doi.org/10.1007/s00383-015-3748-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3748-2