Abstract
Objective
Improvements in diagnostic testing and genital repair have significantly advanced the management of disorders of sex development (DSD). Challenges however, still exist in the management of DSD. This study evaluated the types, challenges of surgical management, and outcome of DSD in south-east Nigeria.
Methods
Retrospective analysis of 39 children with DSD managed from January 2005 to December 2013 at the University of Nigeria Teaching Hospital, Enugu, Nigeria.
Results
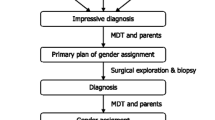
Types of DSD were: 46, XX DSD in 17 (43.6 %) cases; 46, XY DSD 16 (41 %); Ovotesticular DSD 5 (12.8 %); and one (2.6 %) 46, XY Ovotesticular DSD. Median age at definitive gender assignment was 3 years (range 2 months–14 years). Gender assignment was female for 20 (51.3 %; all 46, XX DSD, one each of 46, XY DSD, Ovotesticular DSD and 46, XY Ovotesticular DSD), and male for 19 (48.7 %; 15 of 46, XY DSD, 4 of Ovotesticular DSD). Eight cases reared as male before presentation required gender reassignment after evaluation and counselling. Genital repair was undertaken at mean age of 4.1 years (range 6 months–14 years). After average follow-up of 22.5 months (range 1 month–7 years), a total of eleven (28.2 %) developed procedure-related complications. Challenges were delayed diagnosis, inadequate diagnostic facilities, and need for gender reassignment.
Conclusion
There is a wide spectrum of DSD in our setting. Time to diagnosis, evaluation, and outcome may be improved by public enlightenment initiative, focused education of healthcare personnel and provision of relevant diagnostic facilities through enhanced funding and collaboration.


Similar content being viewed by others
References
Ostrer H (2014) Disorders of sex development (DSDs): an update. J Clin Endocrinol Metab 99(5):1503–1509
Houk CP, Hughes LA, Ahmed SF, Lee PA et al (2006) Summary of consensus statement on intersex disorders and their management. Pediatrics 118(2):753–757
Erdoğan S, Kara C, Uçaktürk A, Aydın M (2011) Etiological classification and clinical assessment of children and adolescents with disorders of sex development. J Clin Res Pediatr Endocrinol 3(2):77–83
Hiort O (2014) Long-term management of patients with disorders of sex development (DSD). Ann Endocrinol (Paris) 75(2):64–66
Mieszczak J, Houk CP, Lee PA (2009) Assignment of the sex of rearing in the neonate with a disorder of sex development. Curr Opin Pediatr 21(4):541–547
Creighton S, Chernausek SD, Romao R, Ransley P, Salle JP (2012) Timing and nature of reconstructive surgery for disorders of sex development—introduction. J Pediatr Urol 8(6):602–610
Maharaj NR, Dhai A, Wiersma R, Moodley J (2005) Intersex conditions in children and adolescents: surgical, ethical, and legal considerations. J Pediatr Adolesc Gynecol 18(6):399–402
Thyen U, Richter-Appelt H, Wiesemann C, Holterhus PM, Hiort O (2005) Deciding on gender in children with intersex conditions: considerations and controversies. Treat Endocrinol 4(1):1–8
Osifo OD, Amusan TI (2009) Female children with ambiguous genitalia in awareness-poor subregion. Afr J Reprod Health 13(4):129–136
Abdullah MA, Saeed U, Abass A, Lubna K, Weam A, Ali AS et al (2012) Disorders of sex development among Sudanese children: 5-year experience of a pediatric endocrinology clinic. J Pediatr Endocrinol Metab 25(11–12):1065–1072
Gnassingbe K, da Silva-Anoma S, Akakpo-Numado GK, Tekou AH, Kouame B, Aguehounde C et al (2009) Transfer of surgical competences in the treatment of intersex disorders in Togo. Afr J Paediatr Surg 6(2):82–84
Furtado PS, Moraes F, Lago R, Barros LO, Toralles MB, Barroso U Jr (2012) Gender dysphoria associated with disorders of sex development. Nat Rev Urol 9(11):620–627
2006 Population Census of the Federal Republic of Nigeria. Analytical report at the National level. National Population Commission 2011
Sowande OA, Adejuyigbe O (2009) Management of ambiguous genitalia in Ile Ife, Nigeria: challenges and outcome. Afr J Paediatr Surg 6(1):14–18
Lee P, Schober J, Nordenström A, Hoebeke P, Houk C, Looijenga L et al (2012) Review of recent outcome data of disorders of sex development (DSD): emphasis on surgical and sexual outcomes. J Pediatr Urol 8(6):611–615
Guerra Júnior G, de Mello MP, Assumpção JG, Morcillo AM, Marini SH, Baptista MT (1998) True hermaphrodites in the southeastern region of Brazil: a different cytogenetic and gonadal profile. J Pediatr Endocrinol Metab 11(4):519–524
Nimkarn S, Likitmaskul S, Sangacharoenkit P, Pathomvanich A, Sawathiparnich P, Wacharasindhu S et al (2002) Ambiguous genitalia: an overview of 22 years experience and the diagnostic approach in the Pediatric Department Siriraj Hospital. J Med Assoc Thai 85(Suppl 2):S496–S505
Parisi MA, Ramsdell LA, Burns MW, Carr MC, Grady RE, Gunther DF et al (2007) A gender assessment team: experience with 250 patients over a period of 25 years. Genet Med 9(6):348–357
Sharma S, Gupta DK (2008) Gender assignment and hormonal treatment for disorders of sexual differentiation. Pediatr Surg Int 24(10):1131–1135
Ocal G, Berberoğlu M, Siklar Z, Bilir P, Uslu R, Yağmurlu A et al (2010) Disorders of sexual development: an overview of 18 years experience in the pediatric Endocrinology Department of Ankara University. J Pediatr Endocrinol Metab 23(11):1123–1132
McCann-Crosby B, Mansouri R, Dietrich JE, McCullough LB, Sutton VR, Austin EG et al (2014) State of the art review in gonadal dysgenesis: challenges in diagnosis and management. Int J Pediatr Endocrinol 2014(1):4. doi:10.1186/1687-9856-2014-4
Hiort O, Birnbaum W, Marshall L, Wünsch L, Werner R, Schröder T et al (2014) Management of disorders of sex development. Nat Rev Endocrinol 10(9):520–529
Tchaou M, Adjenou K, Sonhaye L, Agoda-Koussema LK, N’timon B, Songne B et al (2010) Value of genitography after late discovery of abnormal sexual development: 5 cases in Lome, Togo. Med Trop (Mars) 70(4):410
Warne GL (2008) Long-term outcome of disorders of sex development. Sex Dev 2(4–5):268–277
Ekenze SO, Adiri CO, Igwilo IO, Onumaegbu OO (2014) Virilized external genitalia in young girls: clinical characteristics and management outcome in a low-resource setting. J Pediatr Adolesc Gynecol 27:6–9
Tambiah SJ (1989) Bridewealth and dowry revisited: the position of women in Sub-Saharan Africa and North India. Curr Anthrop 30:413–435
Zainuddin AA, Grover SR, Shamsuddin K, Mahdy ZA (2013) Research on quality of life in female patients with congenital adrenal hyperplasia and issues in developing nations. J Pediatr Adolesc Gynecol 26(6):296–304
Nelson CP, Gearhart JP (2004) Current views on evaluation, management, and gender assignment of the intersex infant. Nat Clin Pract Urol 1(1):38–43
Houk CP, Lee PA (2010) Approach to assigning gender in 46, XX congenital adrenal hyperplasia with male external genitalia: replacing dogmatism with pragmatism. J Clin Endocrinol Metab 95:4501–4508
Lee PA, Houk CP, Husmann DA (2010) Should male gender assignment be considered in the markedly virilized patient with 46, XX and congenital adrenal hyperplasia? J Urol 184:1786–1792
Coran AG, Polley Jnr TZ (1991) Surgical management of ambiguous genitalia in the infant and child. J Pediatr Surg 26(7):812–820
Krege S, Walz KH, Hauffa BP, Körner I, Rübben H (2000) Long-term follow-up of female patients with congenital adrenal hyperplasia from 21-hydroxylase deficiency, with special emphasis on the results of vaginoplasty. BJU Int 86:253–258
Acimi S (2008) Clitoroplasty: a variant of the technique. Urology 72:669–671
Sultan C, Paris F, Jeandel C, Lumbroso S, Galifer RB (2002) Ambiguous genitalia in the newborn. Semin Reprod Med 20:181–188
Wright I, Cole E, Farrokhyar F, Pemberton J, Lorenzo AJ, Braga LH (2013) Effect of preoperative hormonal stimulation on postoperative complication rates after proximal hypospadias repair: a systematic review. J Urol 190(2):652–659
Springer A, Krois W, Horcher E (2011) Trends in hypospadias surgery: results of a worldwide survey. Eur Urol 60(6):1184–1189
Castagnetti M, El-Ghoneimi A (2010) Surgical management of primary severe hypospadias in children: systematic 20-year review. J Urol 184(4):1469–1474
Castagnetti M, El-Ghoneimi A (2011) The influence of perioperative factors on primary severe hypospadias repair. Nat Rev Urol 8(4):198–206
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ekenze, S.O., Nwangwu, E.I., Amah, C.C. et al. Disorders of sex development in a developing country: perspectives and outcome of surgical management of 39 cases. Pediatr Surg Int 31, 93–99 (2015). https://doi.org/10.1007/s00383-014-3628-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3628-1