Abstract
Purpose
It is common to evaluate children who have sustained minor head trauma with computed tomography (CT) of the head. Scalp swelling, in particular, has been associated with intracranial injury. A subset of patients, however, present in delayed fashion, often days after the head trauma, as soft tissue edema progresses and their caregiver notices scalp swelling. We explore the value of further workup in this setting.
Methods
We conducted a retrospective review of a prospectively collected cohort of children ≤24 months of age presenting to the Texas Children’s Hospital with scalp swelling more than 24 h following a head trauma. Cases were collected over a 2-year study period from June 1, 2014 to May 31, 2016.
Results
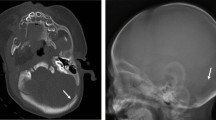
Seventy-six patients comprising 78 patient encounters were included in our study. The mean age at presentation was 8.8 months (range 3 days–24 months). All patients had noncontrast CT of the head as part of their evaluation by emergency medicine, as well as screening for nonaccidental trauma (NAT) by the Child Protection Team. The most common finding on CT head was a linear/nondisplaced skull fracture (SF) with associated extra-axial hemorrhage (epidural or subdural hematoma), which was found in 31/78 patient encounters (40%). Of all 78 patient encounters, 43 patients (55%) were discharged from the emergency room (ER), 17 patients (22%) were admitted for neurologic monitoring, and 18 patients (23%) were admitted solely to allow further NAT evaluation. Of those patients admitted, none experienced a neurologic decline and all had nonfocal neurologic exams on discharge. No patient returned to the ER in delayed fashion for a neurologic decline. Of all the patient encounters, no patient required surgery.
Conclusions
Pediatric patients ≤24 months of age presenting to the ER in delayed fashion with scalp swelling after minor head trauma—who were otherwise nonfocal on examination—did not require surgical intervention and did not experience any neurologic decline. Further radiographic investigation did not alter neurosurgical management in these patients; however, it should be noted that workup for child abuse and social care may have been influenced by CT findings, suggesting the need for the future development of a clinical decision-making tool to help safely avoid CT imaging in this setting.
Similar content being viewed by others
References
Kraus JF, Fife D, Conroy C (1987) Pediatric brain injuries: the nature, clinical course, and early outcomes in a defined United States’ population. Pediatrics 79:501–507
Kraus JF, Fife D, Cox P, Ramstein K, Conroy C (1986) Incidence, severity, and external causes of pediatric brain injury. Am J Dis Child 140:687–693
Kraus JF, Rock A, Hemyari P (1990) Brain injuries among infants, children, adolescents, and young adults. Am J Dis Child 144:684–691
Quayle KS, Jaffe DM, Kuppermann N, Kaufman BA, Lee BC, Park TS, McAlister WH (1997) Diagnostic testing for acute head injury in children: when are head computed tomography and skull radiographs indicated? Pediatrics 99:E11
Masters SJ, McClean PM, Arcarese JS, Brown RF, Campbell JA, Freed HA, Hess GH, Hoff JT, Kobrine A, Koziol DF et al (1987) Skull X-ray examinations after head trauma. Recommendations by a multidisciplinary panel and validation study. N Engl J Med 316:84–91
Schutzman SA, Barnes PD, Mantello M, Scott RM (1993) Epidural hematomas in children. Ann Emerg Med 22:535–541
Pietrzak M, Jagoda A, Brown L (1991) Evaluation of minor head trauma in children younger than two years. Am J Emerg Med 9:153–156
Greenes DS, Schutzman SA (1998) Occult intracranial injury in infants. Ann Emerg Med 32:680–686
Greenes DS, Schutzman SA (1999) Clinical indicators of intracranial injury in head-injured infants. Pediatrics 104:861–867
Lloyd DA, Carty H, Patterson M, Butcher CK, Roe D (1997) Predictive value of skull radiography for intracranial injury in children with blunt head injury. Lancet 349:821–824
Dietrich AM, Bowman MJ, Ginn-Pease ME, Kosnik E, King DR (1993) Pediatric head injuries: can clinical factors reliably predict an abnormality on computed tomography? Ann Emerg Med 22:1535–1540
Ros SP, Cetta F (1992) Are skull radiographs useful in the evaluation of asymptomatic infants following minor head injury? Pediatr Emerg Care 8:328–330
Greenes DS, Schutzman SA (2001) Clinical significance of scalp abnormalities in asymptomatic head-injured infants. Pediatr Emerg Care 17:88–92
Kleinman PK, Spevak MR (1992) Soft tissue swelling and acute skull fractures. J Pediatr 121:737–739
Greenes DS, Schutzman SA (1997) Infants with isolated skull fracture: what are their clinical characteristics, and do they require hospitalization? Ann Emerg Med 30:253–259
Gruskin KD, Schutzman SA (1999) Head trauma in children younger than 2 years: are there predictors for complications? Arch Pediatr Adolesc Med 153:15–20
Schutzman SA, Barnes P, Duhaime AC, Greenes D, Homer C, Jaffe D, Lewis RJ, Luerssen TG, Schunk J (2001) Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics 107:983–993
Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39:800–812
Lindberg DM, Lindsell CJ, Shapiro RA (2008) Variability in expert assessments of child physical abuse likelihood. Pediatrics 121:e945–e953
Wood JN, Christian CW, Adams CM, Rubin DM (2009) Skeletal surveys in infants with isolated skull fractures. Pediatrics 123:e247–e252
Sheets LK, Leach ME, Koszewski IJ, Lessmeier AM, Nugent M, Simpson P (2013) Sentinel injuries in infants evaluated for child physical abuse. Pediatrics 131:701–707
Pierce MC, Kaczor K, Aldridge S, O'Flynn J, Lorenz DJ (2010) Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics 125:67–74
Arrey EN, Kerr ML, Fletcher S, Cox CS Jr, Sandberg DI (2015) Linear nondisplaced skull fractures in children: who should be observed or admitted? J Neurosurg Pediatr 16:703–708
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sellin, J.N., Moreno, A., Ryan, S.L. et al. Children presenting in delayed fashion after minor head trauma with scalp swelling: do they require further workup?. Childs Nerv Syst 33, 647–652 (2017). https://doi.org/10.1007/s00381-016-3332-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3332-7